COVID-19 is short for coronavirus disease 2019, which causes severe acute respiratory syndrome (SARS). The virus found to cause the illness is structurally similar to other SARS-causing coronaviruses, and was therefore named SARS-CoV-2 (Tang et al, 2020a).
The viral pandemic originated in China's Wuhan region at the end of 2019 (Sohrabi et al, 2020) and was declared a global health emergency by the World Health Organization (WHO) (2020) a month later. It was another 3 weeks before Public Health England (PHE) (2020a) released its first novel coronavirus-specific guidance for ambulance services; this has since been adapted numerous times, as knowledge increases and evidence emerges.
The outbreak has been established as having such a sustained spread in the UK that any patient encounter (within 2 metres) requires a degree of personal protective equipment (PPE) (PHE, 2020a). High demand and low supply of PPE, along with helicopter emergency medical services (HEMS) staff being redeployed to frontline ambulance services have left some air ambulance services with a lack of PPE and some having to ground helicopters (Yorkshire Air Ambulance, 2020).
Hampshire and Isle of Wight Air Ambulance (HIOWAA) holds central professional cooperatives with Babcock, which supplies aviation services, and University Hospital Southampton (UHS), which employs and governs HEMS paramedics. The HEMS doctors are consultants who hold substantive posts at various hospitals in Hampshire. HIOWAA has been able to continue operations throughout the pandemic and expand its efforts into other areas in anticipation of a regional or national caseload surge.
Paramedics have been redeployed to the UHS emergency department to work alongside nursing and medical staff. HIOWAA is one of few charity air ambulances supporting a Royal Air Force COVID-19 task group in long-distance national aeromedical retrieval (Bullock, 2020). These changes have been facilitated by reducing assets from two double-staffed vehicles per day (one helicopter and one response car) to a single helicopter response with three medical crew members. This ensures that the service maintains HEMS operations, and provides a ‘clean’ crew member to manage logistics and communications.
Transmission and protection
Symptoms of COVID-19 were initially described as being flu-like, with a persistent cough and shortness of breath as leading features. A loss of smell or taste has also since been identified as a hallmark symptom, particularly following a fever (Centers for Disease Control and Prevention (CDC), 2020; PHE, 2020b; Yan et al, 2020). A correlation has also been found between COVID-19 and ketoacidosis in people with diabetes, which should trigger a clinician's suspicion if encountered (Bornstein et al, 2020; Li et al, 2020).
Gastrointestinal symptoms and faecal transmission have been thought to be significant (Wong et al, 2020), and PHE (2020c) advises that any patient-generated liquid with the exception of sweat should be treated as potentially infectious. WHO and Unicef (2020) dismissed the risk of transmission through faecal matter as low, stating it is unlikely despite the evidence demonstrating otherwise. Zheng et al (2020) established high viral loads in stool only 2 days before guidance from WHO and Unicef were published. It is therefore reasonable to maintain caution around any bodily secretion and excretion.
Droplets from the respiratory tract are the main concern for transmission, and are also of most relevance to prehospital teams. These droplets can infect through primary exposure and secondarily via contact with surfaces (PHE, 2020c). As the lower airways have been shown to hold a significant viral load over the course of the disease as well as after the end of symptoms, there is a risk of producing airborne particles when performing aerosol-generating procedures (AGPs) (Wölfel et al, 2020). AGPs are defined by the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) an expert committee of the Department of Health (DH), which informs the guidance produced by PHE.
Aerosol-generating procedures
Currently, the list of aerosol-generating procedures includes:
Administration of nebulised medication has been advised against by the Australian Department of Health (2020), the CDC (2020) and the Norwegian Institute of Public Health (2020). However, nebulisation has yet to be recognised as an AGP in UK guidance, although its potential to spread organic particles from a patient receiving treatment has been demonstrated (O'Neil et al, 2017; Tang, 2020b). As many nebuliser masks do not incorporate a valve or filter, there is a theoretical risk of droplets from exhalation or coughing in particular being propelled into the ‘acorn’, and subsequently aerosolised and spread through the environment.
Cardiopulmonary resuscitation
Interaction with any patient (within 2 metres) requires the use of level 2 PPE (Figure 1) as a minimum, and any AGP must only be undertaken while wearing level 3 (Figures 3 and 5; Table 1).





| Personal protective equipment (PPE) | |
|---|---|
| Level 2 | Level 3 |
| Disposable gloves | Disposable gloves |
| Disposable apron | Fluid-repellent coveralls/long-sleeved apron/gown |
| Fluid-repellent surgical mask | FFP3* or powered respirator hood |
| Eye protection (if risk of splashing) | Eye protection |
Given this, cardiopulmonary resuscitation (CPR) has become a contested topic. Guidance from the Resuscitation Council (UK) has treated chest compressions as an AGP since the beginning of April (2020a). This position was asserted in a statement published on 20 April, which challenged PHE's decision to not identify chest compressions as aerosol-generating (Resuscitation Council (UK) (RCUK), 2020b). Presumably in response to this, PHE updated its guidance 4 days later, reiterating that chest compressions were a non-AGP (PHE, 2020d).
HIOWAA adopted AGP guidance from both PHE and RCUK and extended this to include chest decompression by both needle and scalpel technique, as well as procedural sedation. There is no published evidence to support these being aerosol-generating, but they were included by rationale. Chest decompression is performed to release pressure, which can be caused by a pathologic conduit between the lung and chest cavity, as in a closed pneumothorax. The procedure itself can create an iatrogenic passageway using either technique. Procedural sedation is not aerosolising, but adverse effects of oversedation or ketamine-induced laryngospasm would trigger airway instrumentation (Royal College of Emergency Medicine, 2019).
Preventing transmission
Many of the skills added by HEMS teams are defined as aerosol-generating, requiring level 3 PPE. HIOWAA uses a set-up of FFP3 face masks, surgical caps, full face visors, generic high-density polyethylene fibre suits and double gloves, with one pair being high-hilted. As an added measure, a paramedic crew member will avoid getting within 2 metres of the patient and remain with the equipment, preparing the drugs or technical equipment required.
Most materials used by HIOWAA are similar to those used by the local ambulance service, which makes it easier for the HEMS team to limit exposure of its own equipment, while still adding advanced drugs, video laryngoscopy and surgical airway equipment, surgical skills and prehospital blood transfusion (Figure 4).
The revised HIOWAA standard operating procedure for prehospital emergency anaesthesia (PHEA) has been amended to fit with new guidance. Airway management is designated exclusively to the most experienced airway interventionist in the team, and should be done using video laryngoscopy (Cook et al, 2020). To limit the spread of aerosols, ventilations are withheld until the circuit has been closed by cuff inflation and a micro-particle filter and a closed in-line suction circuit are used.
No patient by air unless confirmed negative
At the time of writing, no patients are transported by air unless they have been confirmed to be negative for COVID-19 because of difficulties in decontaminating aviation instruments. Babcock (2020) has taken steps to mitigate this by the installing a separation curtain, and PHE (2020a) has changed its guidance to allow for air transfer, which may precipitate a shift towards operations similar to before the pandemic.
Most of air ambulance Helimed 56's (Figure 2) local primary response area has excellent road infrastructure, and the critical care team's modus operandi was to ‘deploy by air, deliver by road’ in the majority of cases, even before the pandemic. It seems appropriate to limit the risk of aircraft contamination, especially as HIOWAA has only a single aircraft at its disposal.
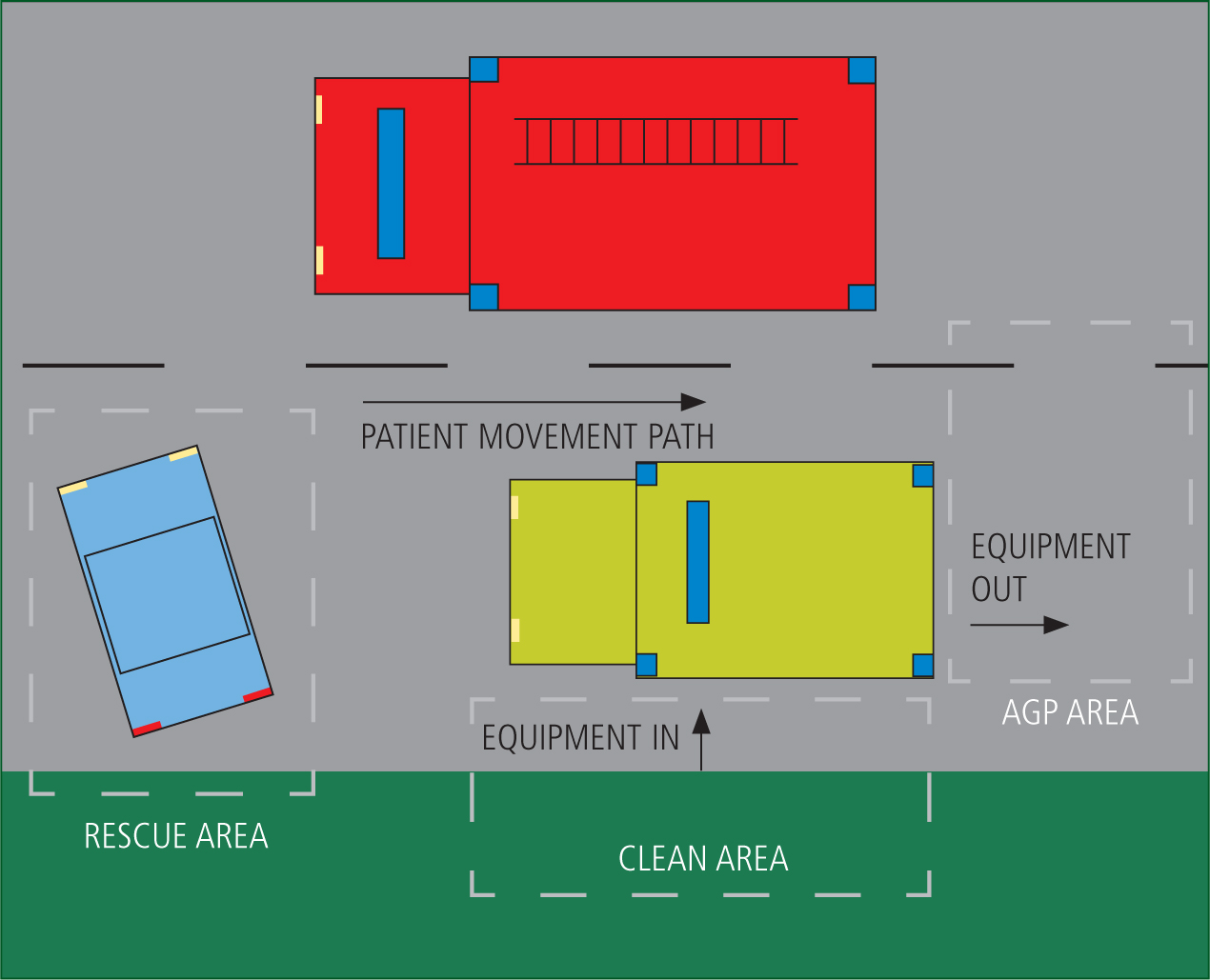
When Helimed 56 attends an incident, the lead clinician and the most suitable other crew member will don appropriate PPE. The third crew member will designate a clean area where they can work and, if possible, an area where AGPs are performed unless this must take place where the patient is situated. The role of the third crew member yields a high task load and it can help if there are uncontaminated health professionals who can work in the clean area. In any case, communication and logistics must be clear at all times to ensure the integrity of equipment and crew.
The clean area should be upwind of any AGP, and it can be beneficial to use the ambulance as an intermediary space between a clean and a contaminated site when circumstances and vehicle design allows. In Figure 6, the third crew member established a cordon on the left-hand side of the ambulance where no patient-facing personnel would be allowed, and designated the rear of the ambulance for the anticipated AGP. A fire truck was parked on the right hand side of the ambulance, creating a natural canal for the patient to be transported into the AGP zone. The inside of the ambulance is treated as contaminated, and kit can delivered in from the side, where it becomes accessible to contaminated personnel from the rear of the vehicle. It is already typical for Helimed 56 to perform PHEA and surgical procedures on the ambulance stretcher at the back of the attending ambulance.
This allows 360° access to the patient, a short distance to retrieve spares in case of equipment failure (other than that accounted for in preparation) and quick access to the inside of the ambulance to keep momentum towards definitive care. An added benefit is that the AGP is performed in a well-ventilated area, adhering to WHO (2020) recommendations. This also reduces contamination to contact surfaces once the patient and practitioners are inside the ambulance, as long as the circuit remains closed throughout.
The front compartment of the ambulance remains clean throughout. To maintain this, the clean HEMS crew member will assist the driver in a safe doffing procedure developed by the HIOWAA clinical management team. The clean crew member can then keep equipment clean in the front cab, and prepare and pass any equipment required to the clinical team. At the end point after hospital handover, the safe doffing procedure is, again, adopted by the clinical team. As a rule, a minimal amount of non-consumable equipment requires decontamination, and can be decontaminated with disposable viricidal wipes, making the HEMS team ready within minutes.
In summary
COVID-19 is caused by SARS-CoV-2, and is now assumed to be widespread in the populace. It poses a risk to healthcare personnel, particularly through transmission by droplets and subsequent contact with affected surfaces.
The novel coronavirus infects the respiratory tract throughout the course of illness, causing procedures and instrumentation that convert droplets to aerosols to pose particular high risk. These require people to be more mindful around safe distancing and the use of PPE. Constantly changing and unpredictable environments are a hallmark of prehospital practice, and critical care teams operating in these conditions must remain adaptive and resilient.
Equally, operation strategies are changing rapidly as new knowledge around COVID-19 emerges. Readily available processes are necessary to keep healthcare providers and patients safe, and clear communication and understanding of roles can enforce this at the roadside.
Although the case study presented herein is not readily generalisable, many of its underpinning principles are.

