Primary angioplasty as an alternative to intravenous thrombolysis for patients with acute ST-elevation myocardial infarction (STEMI) has been shown to reduce mortality, re-infarction, stroke and the need for coronary artery bypass grafting (Keeley, 2003). Thrombolysis is fairly cheap to administer and can be delivered in a range of settings. Primary angioplasty, on the other hand, requires specialist staff and facilities, is more costly to deliver, but is associated with a shorter hospital stay.
Speed of treatment is strongly linked to outcomes for both methods of reperfusion (Boersma et al, 2006), and there have been huge improvements in call-to-needle times for thrombolysis; in part, due to improvements in prehospital thrombolysis, as well as call-to-balloon times (CTB) for angioplasty over the past decade (Myocardial Ischaemia National Audit Project (MINAP), 2010). Economic analyses show that if both treatments are routinely available, primary angioplasty is likely to be cost-effective, compared to thrombolysis if it can be delivered in a timely manner (Bravo et, 2007).
In the UK, provision of primary angioplasty had traditionally been poor compared with other European countries, and in 2004, the British Cardiac Society and the Department of Health (DH) set up a working group to consider the feasibility of implementing a countrywide primary angioplasty service for patients with STEMI in England. Ten hospitals offering primary angioplasty took part in the National Infarct Angioplasty Project (NIAP) during 2005/6 and collected data on call and treatment times, clinical measures, and outcomes for all patients admitted to their hospitals during the year.
The authors were commissioned to undertake an evaluation of these NIAP pilot sites, alongside a small number of control sites who did not routinely offer primary angioplasty facilities, to examine the real-world implications of implementing a countrywide primary angioplasty service. This included describing the different service models available, assessing the workforce implications and impact upon staff of the new service, exploring the patient experience, and estimating the cost-effectiveness of primary angioplasty-based care in the real world.
The results of this project were published in 2008 (Goodacre et al, 2008) and the DH announced that primary angioplasty would take over from thrombolysis as first-line of treatment of STEMI (DH, 2008). Since the evaluation of NIAP, there has been a dramatic increase in the proportion of patients receiving primary angioplasty, with almost half of patients with STEMI receiving primary angioplasty in 2008/9, compared to 27% in 2007/8 (MINAP, 2010). However, due to the importance of speed of treatment for patients with STEMI, there remain a number of challenges to providing an equitable reperfusion service nationally.
In this article, we summarize the main findings from our study, some of which have been published elsewhere (Wailoo et al, 2009; Carter et al, 2010; Sampson et al, 2010). We present some of the results relating to the role of prehospital care in the successful treatment of STEMI.
Methods
We undertook a mixed methods study incorporating four main components: description of the models of service delivery, evaluation of workforce and organizational issues, patient and carer evaluation, and economic evaluation.
For the description of models of service delivery, we collected information regarding the service setting and infrastructure for each of the intervention and control sites involved in the evaluation from site visits and various sources of routine data. We also analyzed a dataset created specifically for the NIAP pilot sites in order to summarize activity levels, routes into hospital and patient characteristics for the intervention sites.
We undertook the evaluation of workforce, implementation and feasibility using a variety of methods. We conducted stakeholder interviews, teamworking interviews, focus groups and a questionnaire survey with members of staff involved in primary angioplasty and with staff working on the boundaries of the service (i.e. ambulance staff, bed managers) at six intervention sites. Data from direct non-participant observation were also collected during fieldwork at sites. A questionnaire was administered to all staff with a role within the angioplasty delivery group at all of the six hospitals involved in the interviews, plus one further intervention site.
We undertook an evaluation of the patient and carer experience using face-to-face semi-structured interviews with patients from the NIAP sites, followed by a postal survey of patients and carers at four intervention and four control sites. The questionnaire consisted of 27 satisfaction items using a 5 point Likert scale. Items included communication with staff, speed and efficiency of treatment, and management of pain and comfort. We then undertook further telephone interviews with patients who had responded to the survey to examine issues raised in earlier interviews and the postal survey further.
For the economic evaluation, we used data collected by the NIAP sites along with additional data from five control sites to estimate the costs and time to treatment of providing primary angioplasty and thrombolysis in routine NHS practice. Multilevel models were used to estimate the mean cost of thrombolysis and primary PCI, adjusting for patient characteristics and treatment location. These data were then used to populate and develop an existing cost-effectiveness model of primary angioplasty. This model uses synthesized evidence from 22 randomized trials to estimate the short-term rate of stroke, death, revascularisations and myocardial infarction, and then extrapolates over the longer term using registry data.
Mortality estimates were adjusted to take into account presentation delay and treatment delay, using data from NIAP and control sites. The model was used to estimate the cost effectiveness of operating a comprehensive primary PCI service compared to a thrombolysis-based service, in terms of the incremental cost per quality-adjusted life year (QALY) gained.
Results
Different models of service delivery
There were seven predominantly urban sites, three of which were in London; three were teaching hospitals in major cities, and one was in a district general hospital in a more rural setting (Table 1). The London Ambulance Service established a bypass service whereby they would take patients from anywhere within their catchment area directly to the nearest primary angioplasty site, bypassing the feeder emergency department (ED).
| Site | Model | Primary PCI Location and availability | Size |
|---|---|---|---|
| 1-3 | Major urban. Multiple centre. 3 primary PCI sites plus 7 feeder hospitals, 3 teaching | 3 teaching hospitals, 2 with EDs and 1 tertiary referral centre with no ED. All offer primary PCI 24/7 ambulance bypass for patients in catchment for feeder hospitals | 1.7 |
| 4 | Major urban. Single centre plus 6 feeder hospitals. | Tertiary referral centre with no ED. Primary PCI available 8-4 Mon-Fri. Ambulance bypass for feeder hospitals | 1.6m |
| 5 | Major urban. Single centre plus 2 feeder hospitals | Teaching hospital with ED. Primary PCI available 24/7, Ambulance bypass for feeder hospitals | 680k |
| 6-7 | Major urban. Multiple centre. 2 primary PCI sites plus feeder hospitals | 2 teaching hospitals with EDs. Primary PCI available 8-4 Mon-Fri | 430k |
| 8 | Urban. Single centre | District general hospital with ED. Primary angioplasty available 24 hours during weekdays, no service weekends | 340k |
| 9 | Major urban. Single centre. 1 site with 1 feeder hospital | Teaching hospital with ED. Primary PCI available 24/7 | 670k |
| 10 | Large urban. Single centre | Teaching hospital with ED. Primary PCI available 24/7 | 390k |
However, some patients were still taken to the feeder ED site first, either as a ‘brush-by’ where the patient did not leave the ambulance but was seen by a medical team in the ambulance and referred straight on, or occasionally the patient would be taken into the feeder hospital emergency department, assessed and then transported to the primary angioplasty site.
In sites where there were feeder hospitals but no ambulance bypass, patients would be assessed in the ED, then transferred by ambulance to the primary angioplasty hospital.
During the pilot year, the proportion of ambulance patients with suspected STEMI who were bypassing the ED and being brought directly to the catheter laboratory area for assessment increased at many sites. The decision to take the patient to the catheter laboratory was made by the ambulance crew, although two sites were able to seek confirmation of diagnosis by faxing (telemetering) ECGs taken in the ambulance to the coronary care unit at the hospital.
We had data on 2072 patients within the NIAP sites. Most patients (94%) were out of hospital at the time of onset of their heart attack, and 80% of these activated the emergency services (either via their GP or calling 999 direct) and were brought to hospital by ambulance. A greater proportion of patients who went direct to the primary PCI site travelled by ambulance, as some of these patients would have been direct ambulance bypass patients.
Patient treatment pathways
Just over two thirds of patients (70%, 1449/2072) in the NIAP year were admitted directly to the primary PCI site, while the remaining 30% (623/2072) were admitted to a hospital without a primary PCI service on site (termed hereafter as a ‘non-primary PCI site’), of whom 70% were transferred to the primary PCI hospital. The treatment received and median CTB times of different referral routes are summarized in Figure 1. Overall, median CTB times were 131 minutes, 161 minutes for patients who went via a non-primary PCI centre, and 120 minutes for those who travelled direct to the primary PCI site. Median CTB by hospital ranged from 83 minutes to 184 minutes.
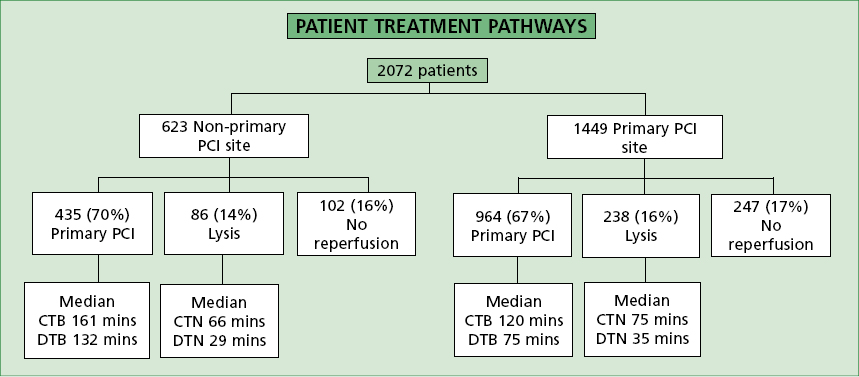
CTB times were longer when patients were transferred from a non-PCI centre. The time delays incurred were such that promptly administered thrombolysis at the non-PCI centre or prehospital thrombolysis may have been as effective as PCI in these circumstances.
The location of place of assessment is a key variable in improving CTB times (Figure 2). The majority of patients (89%, 387/435) who were transferred from a non-PCI site were brought straight to the catheter lab for assessment in the primary PCI centre, with only 7% (29/435) of patients being assessed in the ED. For the patients who travelled directly to the PCI centre, 48% (466/964) were assessed in the ED, with 30% (285/964) being taken directly to the catheter lab for assessment.
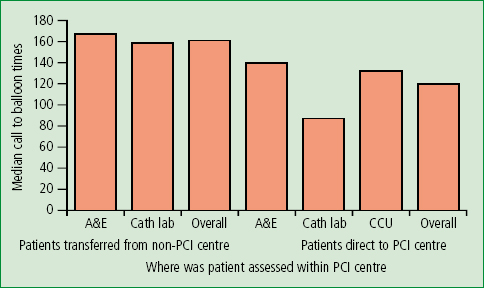
For patients who went directly to a PCI site, those who went directly to the catheter lab for assessment had significantly lower CTB times than those who were assessed in the ED or coronary care unit. This difference is not evident in the transferred patients, but numbers of patients assessed in the ED was very small.
Organizational and workforce issues
A total of 202 staff from seven different sites returned questionnaires and 142 staff from six sites were involved in the staff interviews, focus groups and questionnaires. This included members of staff involved in all aspects of the patient pathway (e.g. catheter lab nurse, CCU staff, ambulance staff). Issues raised within this component of the research relating to the ambulance service fell into two categories; impact upon the ambulance service (threat) and the role of the ambulance service in improving the service (opportunity).
The ambulance service was seen as a key stakeholder for the angioplasty service but resistance to proposed changes were reported at some, but not all sites. Issues were raised around the need for further training of ambulance staff who had been trained to give thrombolysis but had less understanding of the processes involved in angioplasty. It was felt that ambulance staff needed to be fully aware of the processes involved in angioplasty in order to understand the need to transfer the patient quickly and to be able to manage the patients’ pain and symptoms en-route.
Most of the NIAP pilot sites encouraged crews to stay in the catheter lab during the procedure to familiarize themselves with the process. However, ambulance staff explained that training can cause logistic difficulties to the service as it takes staff away from their regular day-to-day work for long periods of time. There were also concerns that long journeys to regional centres or additional ambulance journeys due to transfers will occupy rural ambulances for long periods of time, placing them out of service use for other emergency patients.
The need for ambulance crews to make the transition from giving early prehospital thrombolysis to delivering a patient to the catheter lab as efficiently as possible for the catheter lab to deliver primary angioplasty raised fears that the increase in primary angioplasty will result in the deskilling of ambulance staff in thrombolysis use.
Discussion of the patient pathway highlighted some areas where the ambulance can play a key role in minimizing the CTB time. The geographical position of the catheter lab was stated as a potential barrier. In some of the pilot sites, the ambulance crew were able to access the catheter lab directly, without having to take the patient through the ED, which decreased CTB times.
Staff at a majority of hospitals agreed that the best entry to the system is a simple pathway going straight from the ambulance entrance to the catheter lab with minimal delay. Several centres had implemented a gate-keeper role where a senior cardiology nurse met the ambulance team at the entrance to speedily facilitate the handover.
The provision of an ECG by the ambulance crew was seen as beneficial to the pathway, particularly where the ECG could be telemetered through to the catheter lab/CCU for confirmation of STEMI, as this reduced the likelihood of calling out the catheter lab team on a false alarm and differences of medical opinion on diagnosis, delaying the decision to call in the catheter lab team.
Patient and carer experience
For the patient and carer component, we interviewed 27 patients and 6 carers and sent surveys to 682 patients and 486 carers. We received a response rate of 87% (595/682) patients and 86% (418/486) for carers. There was no difference in response rates between NIAP sites (86%, 372/432) and control sites (89%, 223/250).
Patient and carer satisfaction with overall care was high at both NIAP and control sites (78% vs 71% patients rated their care as ‘excellent’, P=0.074). Patient satisfaction with speed of treatment was higher at NIAP sites (80% vs 67% ‘excellent’, P=0.001). Carers rated the convenience of visiting lower at NIAP sites than controls (12% vs 1% ‘poor’, P=0.001), as NIAP patients were less likely to be at their local hospital.
Patients were significantly more satisfied with their experience of the ambulance journey at NIAP than control sites (73% vs 59% ‘excellent’, P=0.037). Within the free text comments, respondents expressed gratitude towards staff and praised the speed and professional attitude of ambulance staff in particular, but gave no indication as to why satisfaction was higher in intervention than control sites.
Patients who were transferred swiftly from non-primary PCI sites, or who bypassed their local hospital, praised the speed of the decision made by ambulance staff and felt it was a life-saving decision. There was a perception that patients had had their lives saved by the speed and efficiency of their treatment.
‘This for me was the NHS working at its very best. From the 999 call to coming out of surgery took 3.5 hours’ (Patient 307, survey).
A small number of comments in interviews and surveys were made relating to a lack of comfort during the ambulance journey, due to design of the ambulance rather than poor management by ambulance staff. Concerns about ambulance staff needing additional training to deal with primary PCI patients that were raised within the organizational and workforce component of the research were not reflected in the patient and carer responses.
Economic analysis
A total of 2083 patients treated at NIAP sites and 919 patients treated at control sites were included in the analysis. Patients at NIAP sites were more likely to receive primary PCI than thrombolysis (67% vs 16%) and patients at control sites were less likely to receive primary PCI than thrombolysis (4% vs 73%). The mean cost of the treatment episode was £3509 for thrombolysis at control sites, £4361 for thrombolysis at NIAP sites, and £5176 for primary PCI at NIAP sites. Primary PCI was associated with reduced length of stay in hospital.
The National Institute for Health and Clinical Excellence (NICE) criteria for willingness to pay for health gain suggests a threshold of £20 000 per quality-adjusted life year gained to be appropriate (NICE, 2008). Our analysis showed that primary angioplasty-based care was more expensive than thrombolysis-based care but, at £4520 per quality-adjusted life year gained, would be considered cost-effective according to NICE criteria.
Direct access to the primary PCI hospital catheter laboratory was most likely to be cost-effective, whereas thrombolysis-based care was more effective and less costly when the analysis was limited to those transferred from a non-PCI centre. Primary PCI systems which bypassed the ED or CCU were more likely to be effective and cost effective than those that did not.
If we are willing to pay £20 000 per QALY gained, then the probability that direct to catheter lab primary PCI would be considered cost-effective exceeded 95%. If patients arrived via the ED or CCU, this probability was only 75%. Rapid and direct access to the catheter lab is therefore important for ensuring an effective and cost-effective service.
From the patients at NIAP sites that were treated by primary PCI, 13% (179/1399) had an additional ambulance journey and 7% of those treated by thrombolysis (24/330). These journeys were either emergency journeys to transfer them from a non primary PCI centre to a primary PCI centre, or as patient transport to transfer them back to the feeder hospital following the procedure. These additional costs contributed very little to cost differences between thrombolysis and primary PCI patients.
Discussion
We found that primary PCI based services appear to represent a cost-effective use of resources and are acceptable to patients, although treatment delays impact upon the cost-effectiveness and must be minimized. The cost-effectiveness of primary PCI is mainly driven by effectiveness, which in turn depends upon time delay.
If time delays can be minimized, the effectiveness of primary PCI will be optimized and it will be cost-effective (i.e. the additional costs incurred will be justified by the lives saved by more effective treatment). In particular, transfer of patients from a non-primary PCI site to a primary PCI site was unlikely to be considered cost-effective and may be less effective than thrombolysis-based care. If time delays associated with transfer cannot be reduced, it may be better to give thrombolysis to patients presenting to a non-primary PCI site, than transfer for primary PCI.
The ambulance service frequently represents the beginning of the pathway for patients with STEMI and plays an important role in enabling successful reperfusion, improving survival for STEMI patients. The use of ambulance bypass within this study reduced journey times considerably. Time delays could be minimized if ambulance services can ensure that suspected STEMI patients bypass the non-primary PCI centre, even if it is the nearest hospital, and transport the patient directly to the primary PCI hospital.
Where bypass is not available, quick turnaround at ED and transfer onwards can be facilitated by dialogue between ambulance services and EDs. Ideally, ambulances should be able to bypass the ED and transport patients directly to the catheter lab as this has been shown to decrease CTB times significantly. In Canada, Le May et al (2008) recently found similar delays of approximately one hour when patients were referred from emergency physicians, rather than being transferred directly to the catheter lab by paramedics.
Misdiagnosis can lead to catheter teams being activated unnecessarily, putting the system under pressure and incurring additional costs. The role of prehospital care in minimizing misdiagnosis is key and accurate assessment within the ambulance is vital. This can be facilitated by the use of telemetry so that ECGs can be examined by the primary PCI staff prior to the patient arriving at hospital.
There are understandable concerns about the deskilling of ambulance staff in prehospital thrombolysis. Following a period of time where ambulance crews have been encouraged to undertake prehospital thrombolysis and improve call-to-needle times, crews are now frequently required to withhold thrombolytic therapy in favour of managing the patients and delivering them to the nearest hospital to be able to deliver primary angioplasty.
However, some of the skills developed in administering prehospital thrombolysis such as interpretation of 12-lead ECGs and clinical assessment of the patient are as essential for the management of primary angioplasty patients. In addition, there is still a role for thrombolysis and prehospital thrombolysis was delivered to 5.4% of STEMI patients in 2009/10 (MINAP). Local geographical circumstances must be considered and the results of this study, which was based largely in urban areas, may not be as applicable to more rural areas. It is likely that there will be situations nationwide where inter hospital transfers can be achieved within acceptable time limits and other situations where delays are excessive even with bypass and thrombolysis will be the treatment of choice.
‘The ambulance transfer and awareness of ambulance staff of their role in the heart attack pathway is critical to its success’
Conclusion
Primary PCI was found to be a cost effective service, providing door-to-balloon times can be minimized. The ambulance transfer and awareness of ambulance staff of their role in the heart attack pathway is critical to its success. Ambulance crews involved in primary PCI require regular training and updates as to any changes in the care pathway. Further, as the service is now extending to more rural areas, it would be helpful to study the impact of these longer transfers on door-to-balloon times and the knock-on effect onto other paramedic duties.
