Out of hospital cardiac arrest (OHCA) continues to be a major public health challenge, despite increased scientific knowledge about prevention, cardiac arrest pathophysiology, and acute resuscitation. Many changes have occurred in recommendations and guidelines over the last 50 years of modern-era CPR. Recently, there has been more emphasis placed on the importance of providing high quality CPR, especially in the early phases of resuscitation, with a relative de-emphasis on administering drugs and establishing an early advanced airway. Interestingly, recent data has shown that OHCA patients who received ACLS drug administration had no statistically significant improvement in survival to hospital discharge, or long-term survival compared to patients who received no ACLS drugs. (Olasveengen et al, 2009; Jacobs et al, 2011)
It is becoming more apparent that a key to improving survival may depend on high quality CPR. The challenge we currently face is to define the important components of high quality CPR and how CPR can be best integrated into the full resuscitation effort, including delivery of shocks (Cheskes et al, 2011). Many components of good quality CPR such as chest compression depth, compression rate, and full chest recoil that can potentially affect survival are well appreciated. (Abella et al, 2005; Wik et al, 2005). More recently, newer metrics of high quality CPR have been developed which have also been shown to be associated with increased survival. These new metrics include hands-off time, peri-shock pause and chest compression fraction (CCF). The goal of this paper is to define and discuss the clinical perspectives of these newer CPR metrics including how evolving developments in defibrillator technology can assist paramedics in being able to achieve high quality CPR during resuscitation efforts.
Hands-off time, peri-shock pause and chest compression fraction
Hands-off time is any time interval where chest compressions are not being done while a patient is in cardiac arrest. In general, the goal during CPR is to minimise hands-off time and maximise chest compressions in keeping with the guidelines of both the American Heart Association and European Resuscitation Council (2005 American Heart Association Guidelines; Handley et al, 2005). However, there are several unavoidable reasons for hands-off time including movement of the patient to an optimal location to perform CPR, rhythm analysis, checking for pulse in the event of an organised heart rhythm after a cycle of chest compressions, delivery of shocks, delivering breaths and the performance of endotracheal intubation (Wang et al, 2009).
The peri-shock pause is the hands-off time spanning the time before and after the delivery of a shock. It is comprised of two contiguous time intervals. The pre-shock pause is the time between the last pre-shock chest compression and the delivery of the shock, and post-shock pause is the time between delivery of the shock and the first post-shock chest compression (Figure 1) (Cheskes et al, 2011).
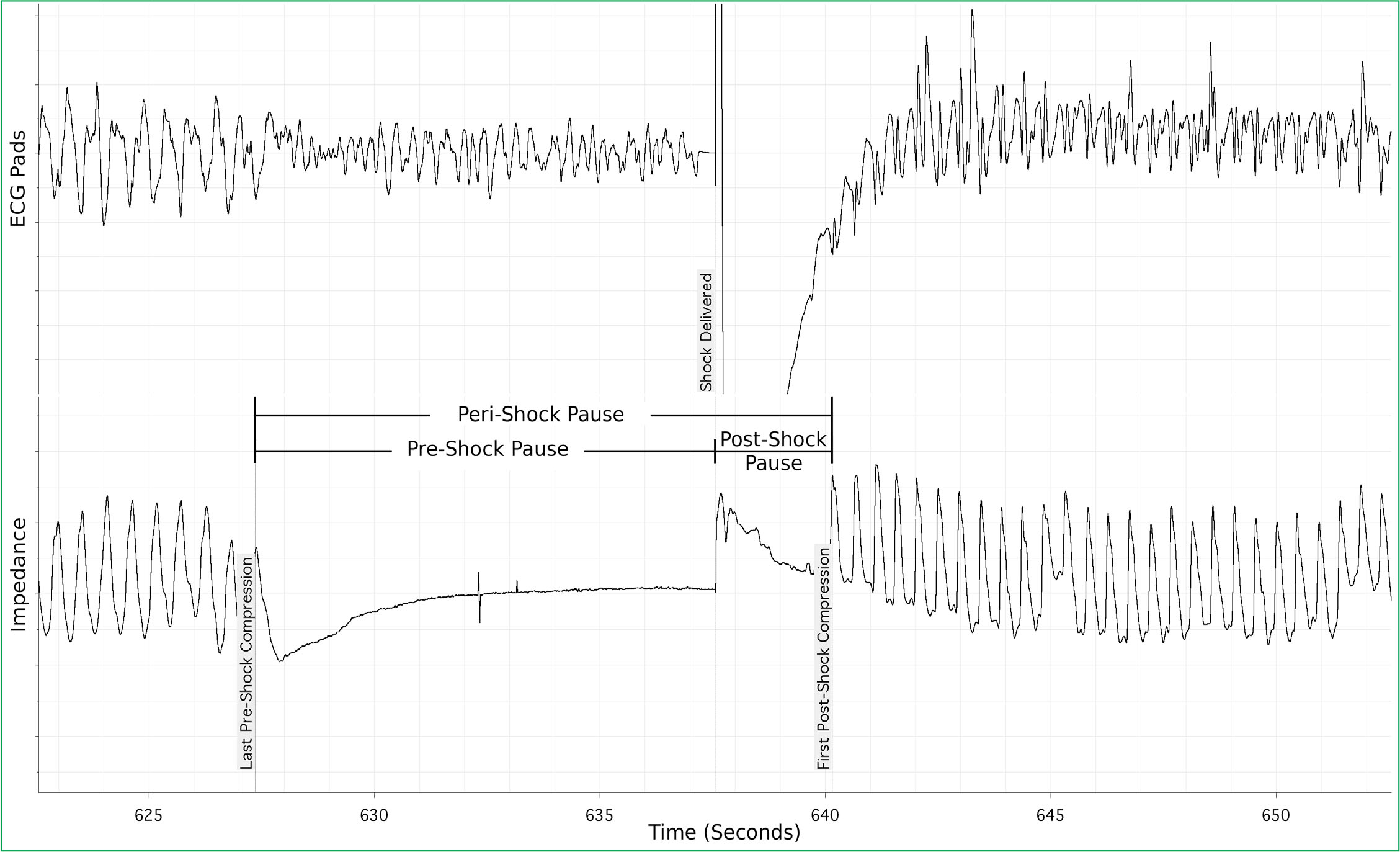
Animal studies have previously indicated a strong relationship between a shorter peri-shock pause and improved outcomes (Berg et al, 2003; Tang et al, 2006). It has been suggested that differences in the peri-shock pause could contribute to a more than two-fold variation in the success of resuscitation efforts (Snyder and Morgan, 2004).
The importance of the peri-shock pause in humans was recently investigated by Cheskes (Cheskes et al, 2011) in a study which reviewed 815 OHCA patients presenting with a shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia). Statistical analysis was done to determine the relationship between survival and the peri-shock pause duration. The analysis showed the odds of survival were significantly lower for patients with a pre-shock pause ≥ 20 seconds (odds ratio, 0.47; 95 % confidence interval, 0.27–0.82) or a peri-shock pause ≥ 40 seconds (odds ratio, 0.54; 95 % confidence interval, 0.31–0.97) compared to patients with a pre-shock pause < 10 seconds and peri-shock pause < 20 seconds respectively (Table 1). Survival decreased by 18 % and 14 % respectively for every five second increase in either the pre-shock or peri-shock pause. Interestingly, the post-shock pause was not found to be independently associated with improved survival.
TEMS=emergency medical services, CPR=cardiopulmonary resuscitation, arrival time=time from 911 call dispatch to first vehicle arrival on scene. (Episodes with missing variable data were excluded from the analysis).
The chest compression fraction (CCF) is the proportion of resuscitation time actually spent performing chest compressions while a patient is in cardiac arrest. It can be reported in various ways—either minute-by-minute epochs or for the first few minutes of resuscitation or for the whole resuscitation effort prior to ROSC. As an example, a CCF of 0.75 means that compressions were being done during 75 % of the reported time interval. Obviously the longer the hands off-time, the lower the CCF.
Christenson (Christenson et al, 2009) has shown that an increased CCF is independently associated with survival in patients presenting with a shockable heart rhythm. This study included 506 adult OHCA patients with confirmed ventricular fibrillation or pulseless ventricular tachycardia and no defibrillation before emergency medical services arrival. Electronic waveform tracings of chest compressions prior to and including the first shock were reviewed in one minute intervals. Patients were followed until discharge from the hospital or in-hospital death. It was found that the adjusted odds ratio of surviving to hospital discharge in patients with a CCF of 61–80 % and 81-100 % compared to patients with a CCF of 0–20 % were 3.01 (95 % confidence interval 1.37–6.58) and 2.33 (95 % confidence interval 0.96–5.63) respectively.
These newer concepts demonstrated in these observational human trials aid to solidify our understanding of the importance of high quality CPR and suggest that we should do our best to incorporate them into clinical practice. Fortunately, these concepts are readily adaptable to the clinical setting in conjunction with the modifications and technological advances in defibrillator/monitor technology. We describe below how these defibrillator modifications may decrease shock pause duration and increase chest compression fraction, hence improving the quality of CPR performed.
Defibrillator Technology and High Quality CPR
Defibrillator mode
The use of a defibrillator in the ‘automated external defbrillator’ (AED) mode typically requires obligatory hands-off time for rhythm analysis. This may result in a prolonged pre-shock pause duration. In a study of the variation in CPR interruption among seven AEDs, a wide variation was observed in pre-shock pause ranging from 5.2 to 28.4 seconds with only one AED achieving an interruption of < 10 seconds (Snyder and Morgan, 2004). This variation is related to the differences in imposed hands-off time during automated rhythm analysis amongst defibrillators studied.
On the other hand, using a defibrillator in manual mode eliminates the need for AED-driven heart rhythm analysis. This can decrease the pre-shock pause and has the impact of increasing CCF since the interruption to CPR is minimised. This is only achieved, however, if paramedics minimise the time spent on performing manual rhythm analysis. It is critical to make a ‘quick decision' on whether or not a shockable rhythm is present. The tendency to ask partners for a ‘second opinion’ and ‘running through the chest leads’ to try to differentiate asystole from fine VF must be avoided. If a provider is uncertain as to whether a rhythm is shockable, training should focus on immediate CPR minimising CPR interruption in these instances. This technique may decrease the reported risk during manual mode rhythm analysis of shocking nonshockable rhythms, which is noted to be as high as 20 % in one literature review (Edelson et al, 2010).
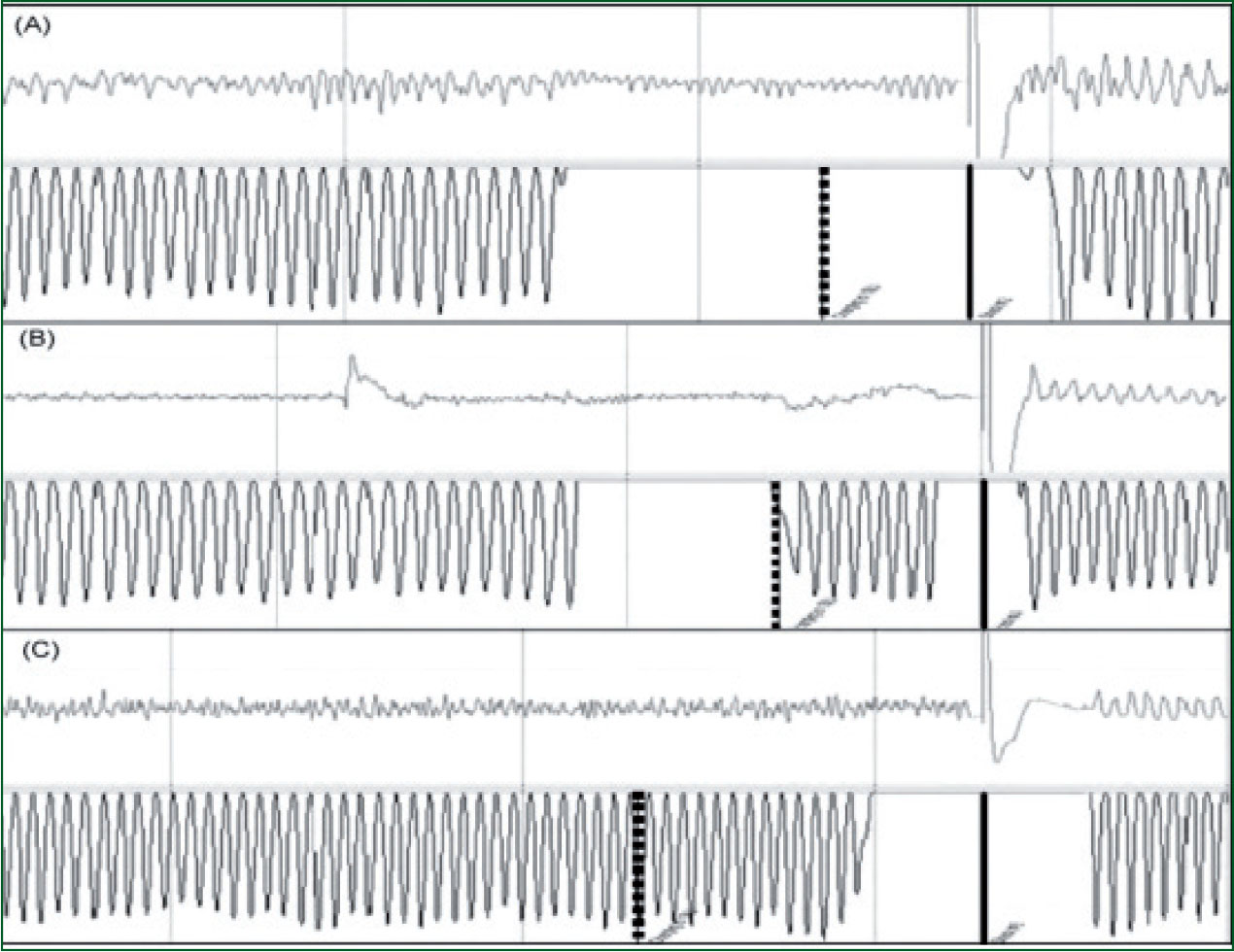
Whether using a defibrillator in the AED or manual mode, the pre-shock pause can be further prolonged if chest compressions are not performed while the defibrillator is charging. In an attempt to minimise these pauses, the American Heart Association recommends performing chest compressions during the defibrillator charging phase (Edelson et al, 2010) Chest compressions during charging is underused in clinical practice. This technique (Figure 4, tracing B) has recently been shown to contribute to decreased hands-off time preceding defibrillation with minimal risk to patients or rescuers (Edelson et al, 2010). Another way of stating this is that its use is associated with a decreased pre-shock pause and an increase in CCF which increases the likelihood of termination of ventricular fibrillation (Cheskes et al, 2011).
Defibrillator charging during compressions
A relatively new technology that is available on some models of defibrillator is a feature that allows charging of the defibrillator capacitor while CPR is ongoing. The result is the defibrillator being ready to deliver a shock as soon as rhythm analysis is completed which obviates the need for chest compressions during charging. This technology can reduce the pre-shock pause significantly. In defibrillators that are being used in manual mode without a ‘charging during compressions’ feature, the equivalent result can be accomplished by pressing the charge button during the last few seconds of a cycle of chest compressions prior to rhythm analysis being performed (Figure 5, tracing C). This has recently been demonstrated to be safe and to decrease the pre-shock pause by up to 10.7 seconds. (Edelson et al, 2010)
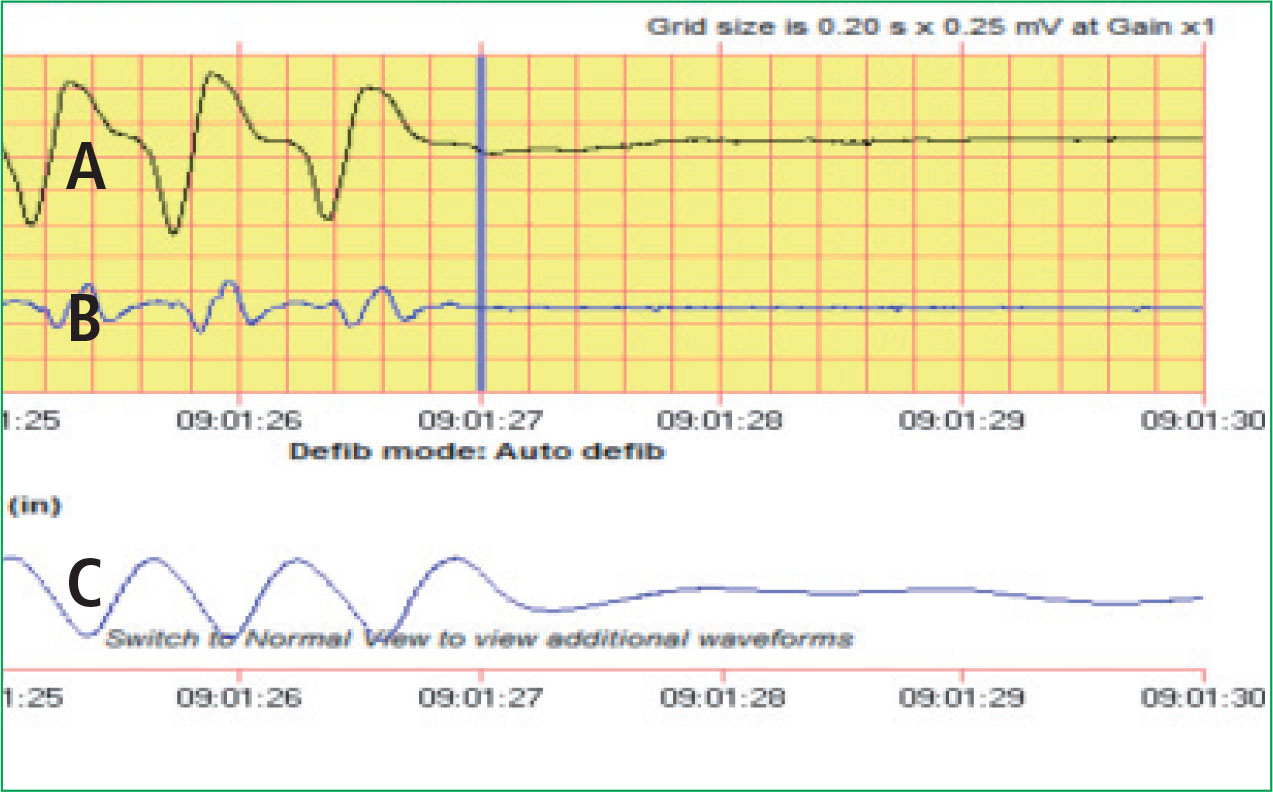
‘See through’ CPR
‘See through’ CPR technology uses filtering software that can remove, in real time, chest compression waveform artifact from the heart rhythm tracing on the monitor. This allows for clearer visualisation of the patient's true underlying heart rhythm during CPR and has the potential to minimise interruptions in chest compressions for analysis while CPR is ongoing. Figures 2 and 3 demonstrate the potential of ‘see through’ CPR when used during real-time cardiac resuscitation.
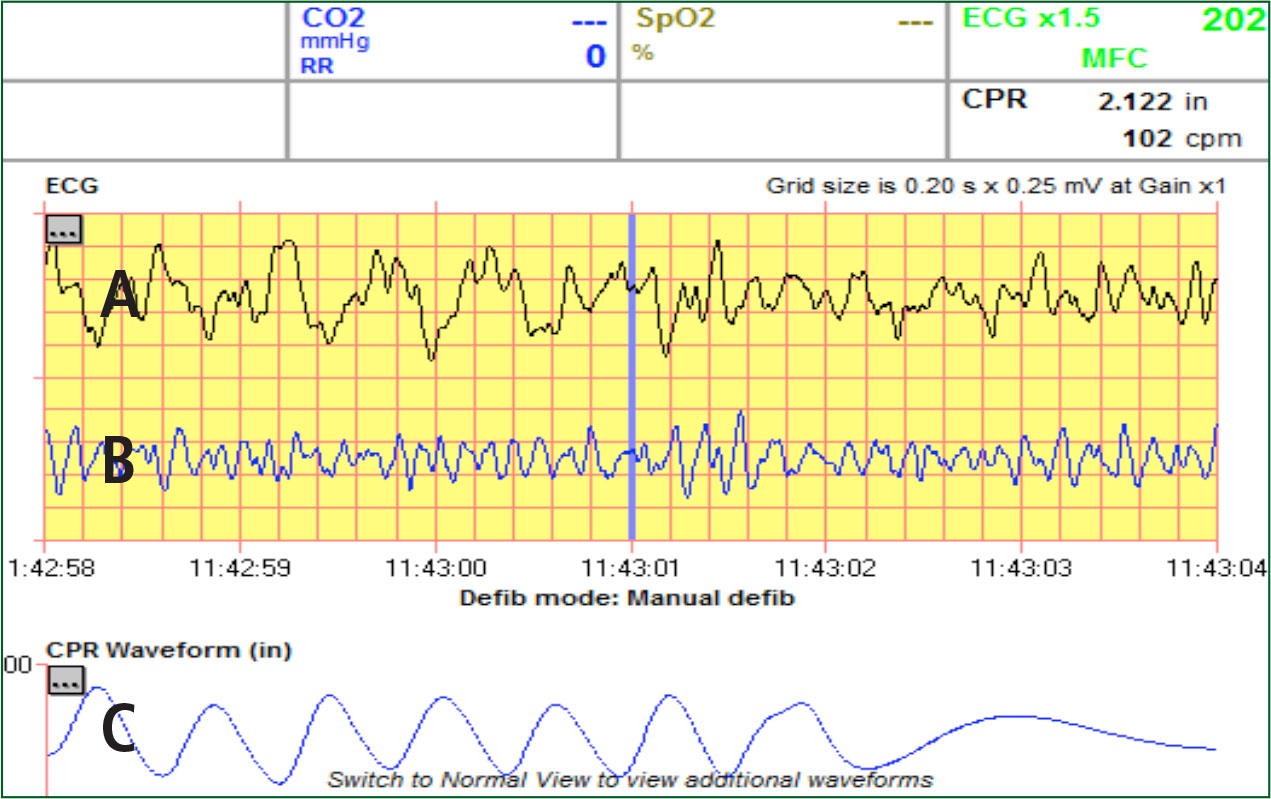
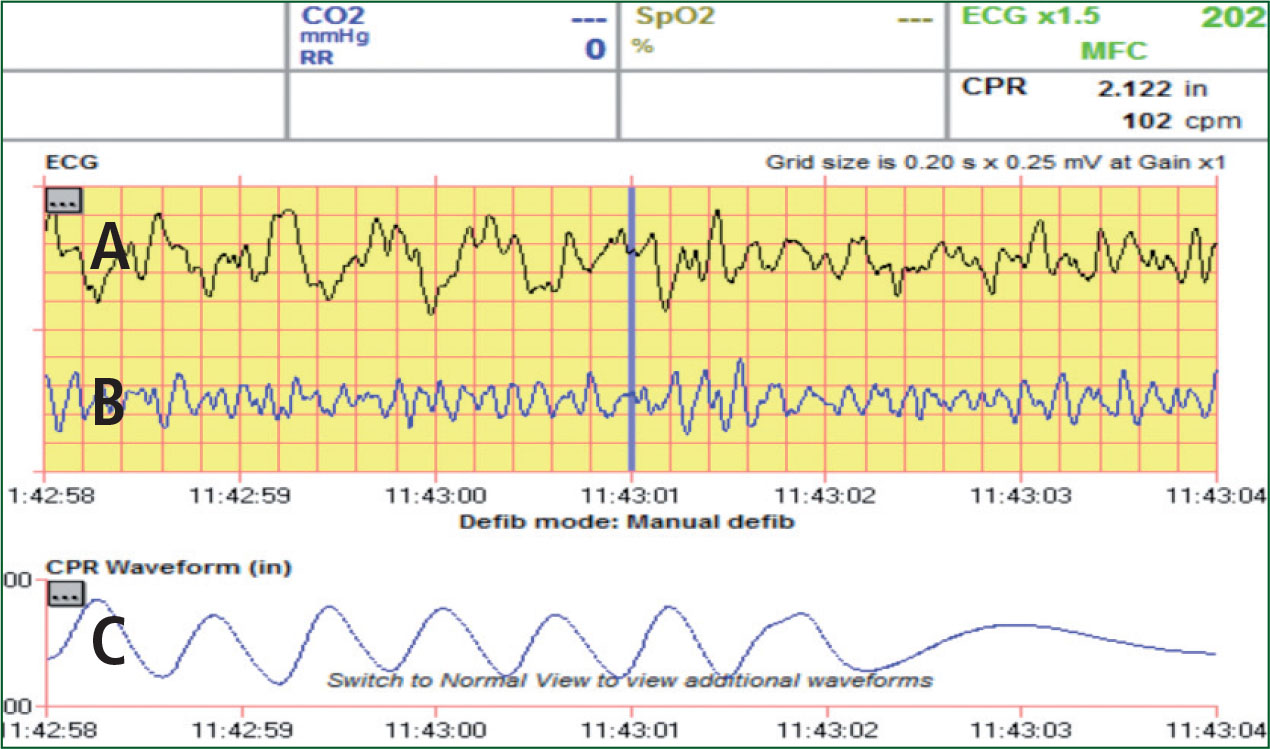
The ability of the fltering software to remove CPR waveform artifact appears to be inversely related to the depth of compressions hence with greater compression depth the ability of the software to filter is diminished. This occurs most commonly with patients in asystolic rhythms (Figure 5) and limits its usefulness in these situations. At this point in time, see-through CPR appears to be a very promising technology which needs to be further evaluated before being implemented on a widespread basis.
Implications of defibrillator technology for paramedic performance
Traditionally recognised concepts of good quality CPR include appropriate chest compression rate and depth, allowing full chest recoil, switching chest compressors after every CPR cycle and completing consistent full cycles of chest compressions. In addition to these, the newer concepts of minimising hands-off time, minimising the peri-shock pause (especially the pre-shock pause) and maximising CCF should be incorporated into paramedic practice. This will result in moving from good quality CPR to high quality CPR.
All this can be readily achieved by beginning chest compressions as soon as possible and interrupting chest compressions only when absolutely necessary. Manual rhythm interpretation is preferable if done quickly and decisively. Ideally a defibrillator with “charging during compressions” capability should be used, but if not available, chest compressions should be done during defibrillator charging or manually charging the defibrillator during the last few seconds of chest compressions prior to a manual rhythm analysis. Chest compressions should be restarted immediately after a shock is given or if asystole is noted during rhythm analysis. In the event of an organised heart rhythm being noted, a pulse check should be limited to less than 10 seconds.
In our region, dedicated training of paramedics in the concepts of hands-off time, pre- and peri-shock pause, CCF and performing high quality CPR has resulted in an overall decrease in median pre-shock pause from 18.5 seconds to 11.1 seconds, with a concomitant increase in the median CCF from 0.62 to 0.78.
Conclusion
Sudden cardiac death is an epidemic with an extremely high mortality rate and continues to challenge emergency medical services (EMS) systems. Hands-off time, peri-shock/pre-shock pause, and chest compression fraction are key modifiable aspects of high quality CPR. Ongoing attention to improving the quality of CPR provides hope that further increases in survival from OHCA are possible.
