Affecting children, predominantly those under the age of five, Kawaski disease (KD) is one of the main causes of heart abnormalities in children in the UK and USA—older children and teenagers can also contract KD, though such cases are very rare. KD promotes virus–like symptoms which can lead to inflammation in the blood vessels, arteries, veins and capillaries of the patient. Although there has been extensive research into this potentially fatal illness, the cause is still unknown, despite many hypotheses having been put forward over the years.
Statistics show that approximately eight in 100 000 children have Kawasaki disease (KD) within the UK, with the majority of cases being in boys (BUPA, 2010). Affecting children under the age of five, KD is one of the main causes of heart abnormalities in children in the UK and USA (Brogan et al, 2002), although older children and teenagers can contract KD, though such cases are very rare (Kawasaki Disease foundation, 2012).
KD promotes virus like symptoms that lead to inflammation in the blood vessels, arteries, veins and capillaries of the patient. Although there has been extensive research into this potentially fatal illness, the cause is still unknown and therefore many hypotheses have been put forward over the years (Kawasaki Disease foundation, 2012).
Although KD is relatively rare, it still affects hundreds of children within the UK and due to the various complications that can arise from KD as it develops the importance of early recognition and transport to hospital is high.
This article will provide a guide for the recognition of KD symptoms for paramedics in the pre-hospital setting, with a brief look at electrocardiogram (ECG) changes, pathophysiology and psychological effects that may be encountered. Unfortunately, there are currently no pre-hospital pharmacological interventions currently available to paramedics, therefore this article will look at pharmacological interventions available in the hospital setting. Finally this article will analyse current studies and research, paying attention to long–term consequences of KD and how having a background knowledge of KD can help pre-hospital paramedics manage patients more efficiently.
What is Kawasaki disease?
Kawasaki disease is an acute systemic inflammatory illness of young children that can result in coronary artery aneurysms, myocardial infarction and sudden death in previously healthy children (Rowley et al, 2010).
Dr Tomisaku Kawasaki, a paediatrician from Japan, documented visiting a four year old child with a rash, fever and an unknown presenting illness. He monitored fifty Japanese children with similar symptoms over a period of six years before finally documenting KD as a diagnosis in 1967 (Burns et al, 2004). Although positive that KD was a potentially fatal disease, other professionals disagreed. Other pathologists and paediatricians from Japan challenged Dr Kawasaki’s prognosis arguing that KD had no long–term side effects (Burns et al, 2000). This debate continued until a report was published in 1970 looking at ten autopsy reports from deceased children who had KD (Burns et al, 2000). The reports showed that patients had died as a result of coronary artery aneurysms secondary to KD demonstrating the long–term health repercussions for those with the disease. Since this initial diagnosis, KD has been seen in almost every country throughout the world (Brogan et al, 2002).
KD has more cases reported in Japan than any other country (Brogan et al, 2001) although there has been no evidence suggesting that direct person–to–person contact increases the risk of spreading the disease (Tizard, 2005).
Similarly, infantile polyarthritis nodosa (IPN) has been closely linked to KD since its diagnosis due to the close clinical signs of the two conditions. IPN is a rare and chronic condition affecting children, generally below the age of two. IPN affects small and medium arteries causing ischaemia and infarction (Thatayatikom et al, 2011), and, although paramedics are unlikely to be able to differentiate between IPN and KD in the pre-hospital environment, background knowledge of both is important in order to recognise and understand clinical changes in the presenting patient. It should be noted however that there are currently no protocols for the management of adult patients who have previously had KD during their childhood (Gordon, 2009).
Causes of KD
The aetiology of KD is still not known although many theories have been suggested, including the proposal that KD develops from a response to microorganisms within the body and/or a virus with which healthy children would experience no negative health effects from.
A response to carpet cleaning materials has also been suggested, as well as the proposal that disease is manifested from a source of infection although no sound proof has been found in either case (Scheinfeld, 2012).
Coronary arteries affected by KD
Coronary arteries keep the heart supplied with oxygen and nutrients from the blood they carry to it. There are two main coronary arteries, the left and right coronary arteries, which supply that oxygen and nutrient rich blood to the atria, ventricles and septum of the patient’s heart (Figure 1). The left coronary artery branches off to the left anterior descending branch which supplies the anterior region of the heart. The left circumflex branch supplies blood to the posterior and the left lateral aspect of the heart. The right coronary artery supplies the right and inferior aspect of the heart (Gregory et al, 2010).
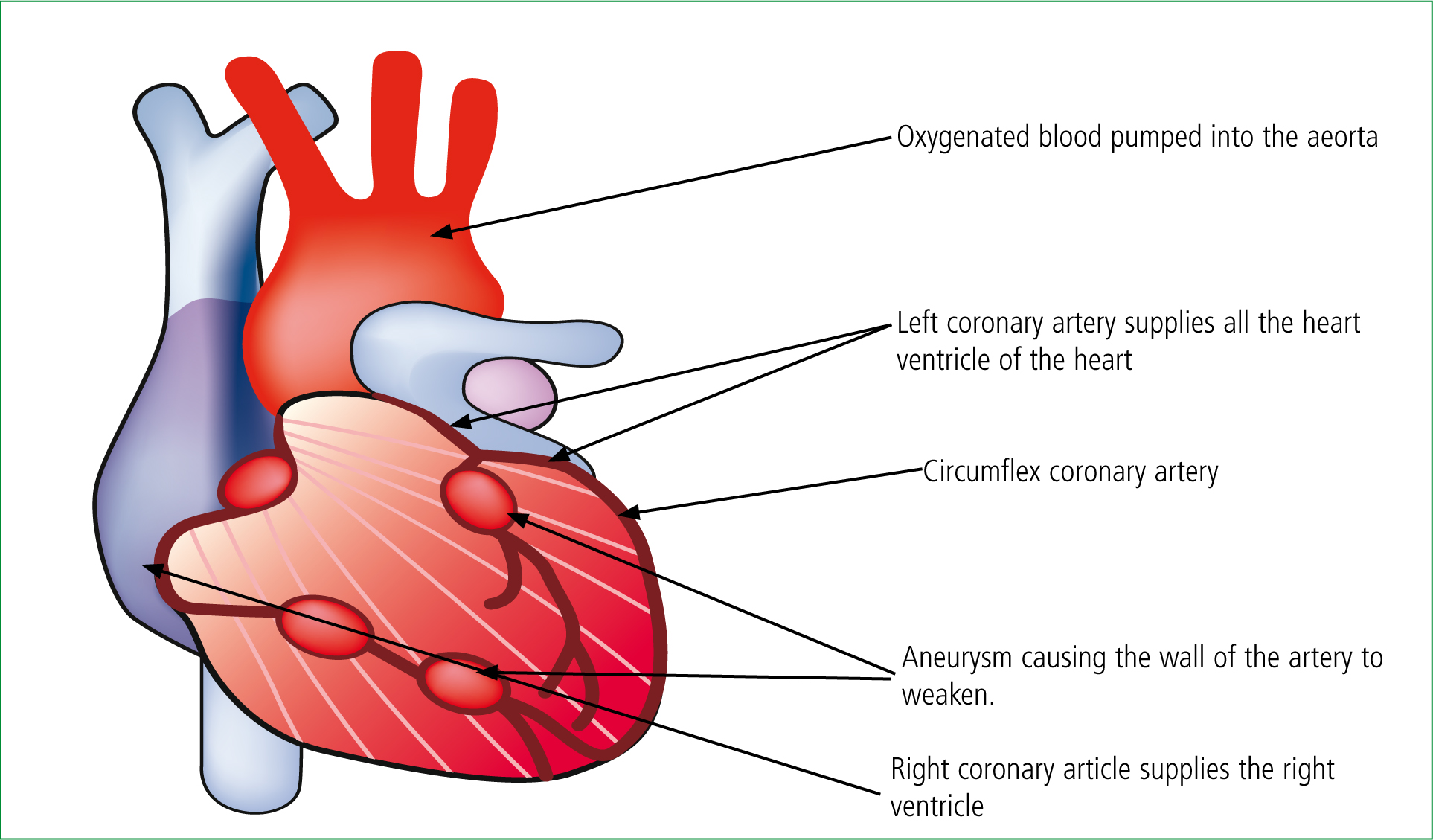
KD affects these coronary arteries by causing inflammation and reducing oxygen and nutrient enriched blood from reaching the heart. Coronary artery aneurysms are an increased risk factor for children with KD due to the inflammation of the coronary walls, and are defined as dilatation in the diameter of a coronary artery segment to more than 1.5–fold normal (Cohen, 2008)—this mass over time has the potential to rupture.
ECG changes in KD
ECG changes have been noted in children during the acute phase of KD if coronary artery dilation is present, and 12-lead ECG tracings were conducted on twenty patients during their KD phases (Hiew, 1992).
Eleven patients presented with elevated S-T segments and eleven with deep Q–waves, highlighting the need for ECG interpretation in the pre-hospital environment to determine the severity of the disease if KD is suspected.
Pathophysiology of KD
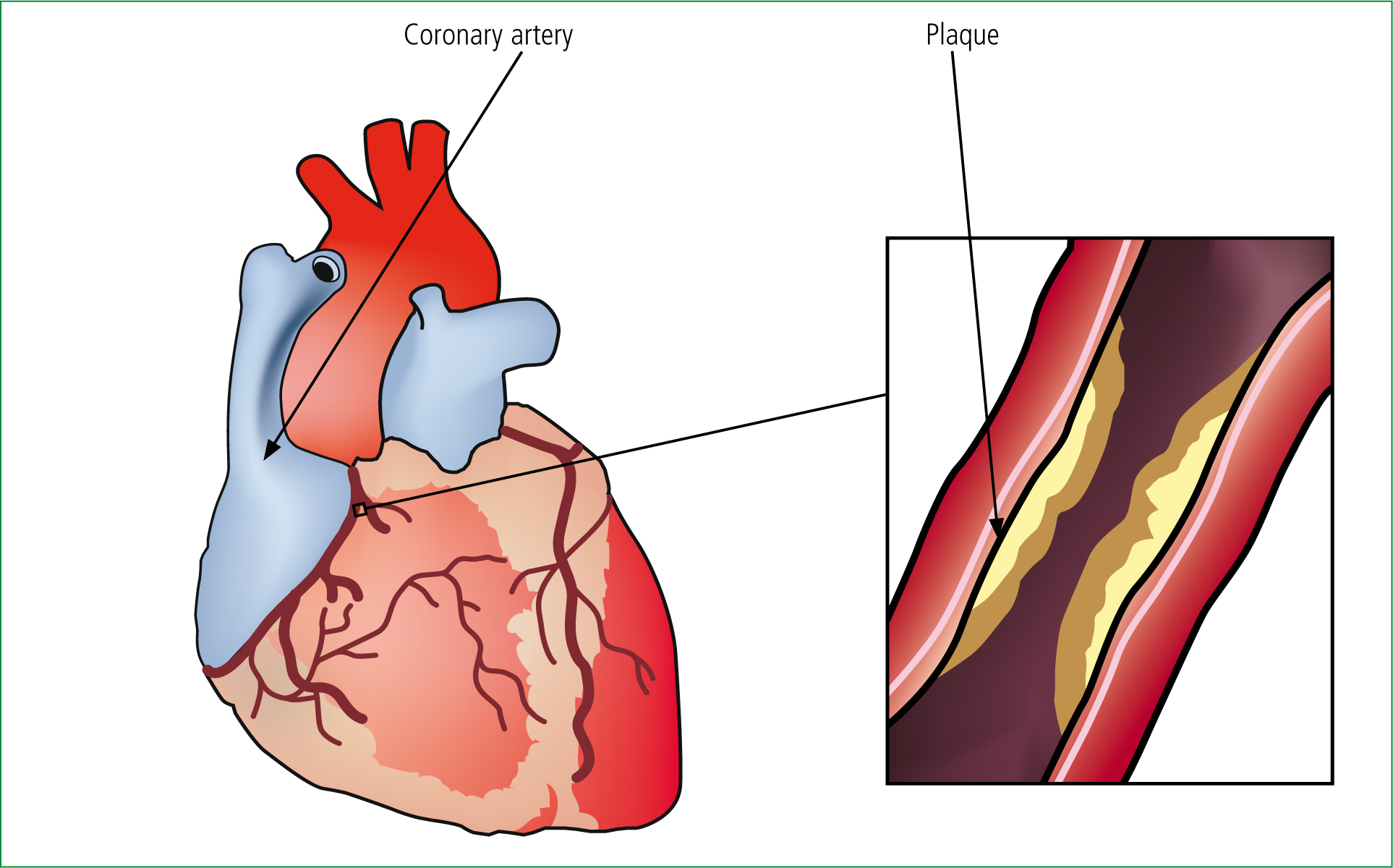
KD is an inflammatory disease that progresses with an extended fever. The inflammatory response this rare condition has on the coronary arteries potentially causes Coronary Artery Aneurysm (CAA) which can be fatal if gone undiagnosed (Burns et al, 2000). Due to inflammatory effect, the heart receives less oxygen and nutrient enriched blood, potentially leading to ischemia of the heart. Current research suggests that matrix metalloproteinase (MMP) play a key role in the formation of aneurysms in KD patients. MMP or matrix-ins are located in the extracellular level of cells. MMP are responsible in many functions including shaping of cells, wound healing and remodelling of damaged cells after injury (Nagase, 2005). In KD patients, oedema and neutrophil fill the coronary artery walls leading to MMP developing around the site. MMP attacks and begins to break down the elastic lamina and media leading to stenosis (Figure 2) and the formation of aneurysms (Senzaki, 2006). There are three phases as KD develops in the patient:
Febrile phase
During this phase the child may become irritable with a fever lasting four days or more. The tongue and lips will start to become red. Erythema and oedema will start to develop on the hands and feet restricting the walking ability of the child. It has been noted in some cases of cardiac abnormalities being present including myocarditis. Conjunctivitis and a rash are also present in the first stage of KD.
Subacute phase
This phase of the condition should cease beyond the fourth week. If fever is still persistent at this stage, the outcome is normally not as good due to the increased risks of cardiac abnormalities. Peeling of toes and fingers are apparent during this phase and the mortality rate is also higher.
Chronic phase
This phase of the illness only occurs if patients have developed cardiac abnormalities. Cardiac effects may progress into adulthood and the risk of abruption of aneurysms is increased.
The causes of each of the phases above is suspected to be related to the systemic inflammatory reaction. The reasons behind the gradual reduction in fever without improvement in this condition are still not fully understood (Burns et al, 2004).
Recognising KD
There are currently no testing methods available to diagnose KD (Brogan et al, 2001), and therefore recognition of the classic signs and symptoms of this condition is the main role of the paramedic in the pre-hiospital environment. However, there are potential indications of KD in children with a fever lasting five days or more, and who do not respond to conventional child fever medicine) (Table 1). Some of the key indicatiors include:
| Criteria | Description |
|---|---|
| Fever | Period of five or more days, PLUS four of the following: |
| 1 Conjunctivitis | Bilateral, bulbar non-supportive |
| 2 Lymphadenopathy | Cervical > 1.5 cm |
| 3 Rash | Polymorphous, no vesticles or crusts |
| 4 Change to lips/oral muscosa | Red, cracked lips; strawberry tounge; diffuse erythema of oropharax |
| 5 Chage of extremities | Initial stage: erythema and odema of palms and soles. Convalescent satge: peeling of skin from fingertiops. |
Adapted from Brogan et al 2001
It must be highlighted that children with a fever lasting more than 5 days who do not respond to normal fever medication may still have KD even if not all of the symptoms mentioned above are present. (Brogan et al, 2001). Any child presenting with five day or more fever should be considered to have KD and be transported to the nearest accident and emergency (A&E) facility (NICE, 2007).
The symptoms associated with KD generally dissipate within the first 10 days of onset of the disease regardless of whether or not the child has received treatment. Research suggests that 20–25 % of these cases develop coronary artery aneurysms (CAA) that may not be detected until early death later in life due to myocardium infarction. Treatment of KD within the frst 10 days of onset dramatically reduces the chance of CAA development (Burns et al, 2004). This is significant for paramedic’s pre-hospitally and further emphasises the importance of early hospital admission.
Pharmacology interventions
Due to the inflammatory response that KD imparts on patients, one thought for treatment is to tackle the inflammation. The use of corticosteroids was examined in a randomised control trial (Newburger, 2007). The trial looked at the use of corticosteroids in conjunction with immunoglobulin (IVIG) and high doses of aspirin. Two groups took part in the trial. Group 1 received corticosteroids with the conventional KD treatment drugs and Group 2 received a placebo.
On completion of the trial, both groups of patients produced similar results in terms of length of fever time, recovery period and adverse reactions to KD drugs and therefore the findings of the study showed no evidence for beneficial use of corticosteroids (Newburger, 2007). In terms of aspirin, to date, the only trial looking at high dose aspirin treatment alone showed that 20–40 % cases developed CAA later in life. The combination of high dose aspirin and IVIG reduced that number to around 9 % (Taubert el al, 1999). This appears to be the reason behind aspirin not being indicated in the pre-hospital setting. This is significant for paramedics to emphasise the importance of rapid transfer.
Current pharmacological interventions are only available in the hospital setting. During the acute phase, aspirin is given as an anti-infammatory therapy 30–100 mg/kg/day. As previously discussed, KD promotes inflammatory effects across the body therefore a higher dose of aspirin is required to combat this.
As the fever begins to reduce, aspirin is then given as an antiplatelet therapy at 2–5 mg/ kg every day. The aim of this is to reduce the chances of formation of CAAs. This will continue until ECG abnormalities are reduced. It is well recognised that aspirin has the potential to cause gastric bleeding during therapy, though it has also been recorded that this side effect is rare in the treatment of KD (Matsubara et al, 1996). National Institute for clinical excellence (NICE) published a guidance in 2007 to prompt health care professionals to consider KD in children under five with a prolonged feverish illness not alleviated with conventional child medications such as paracetamol.
Current research and evidence within the UK advises that KD be treated with combined intravenous immunoglobulin (IVIG) and high doses of aspirin (NICE, 2007). IVIG are antibodies that fight infections and bacteria, they are naturally occurring in the human body which produces these antibodies of its own accord (Tortora et al, 2009). In KD patients, donor IVIG is administered in an attempt to boost the patient’s immune system. IVIG is not licenced for paramedics to carry or administer (Joint Royal Colleges Ambulance Liaison Committee (JRCALC), 2006) due to the lack of accurate tests available to diagnose KD, diagnosis is solely made on the basis of the symptoms present. As the disease progresses, the likely development of cardiac problems dramatically increases (Burns et al, 2004). From the research currently available it appears that due to the lack of controlled studies into high–dose aspirin and administration alone being of any benefit, it has yet to be indicated for paramedics to administer drugs within the pre-hospital environment for KD.
The combination of aspirin and IVIG appears to be the only approved treatment therefore this would highlight the importance of early recognition of symptoms by paramedics with swift transport to A&E.
Psychological effects from KD
As previously discussed, children with KD will have a fve–or–more days history of fever. The lack of relief from conventional medicines such as Calpol will undoubtedly have the child in a state of despair and it is likely that both family and child will be distressed during this time and subsequently a calm and gentle approach will be required when managing the situation.
Carlton-Conway et al (2005) released a paper which look at the behavioural changes in KD sufferers—the study showed that KD can be associated with behavioural sequelae and it was highlighted that future follow–up care for emotional support or referral to a clinical psychologist may also be required.
Further studies have been released linking KD with long term behavioural problems. King et al (2000) released a paper whereby 32 patients with past diagnoses of KD were examined for cognitive, behavioural and academic deficits. While the findings of the study showed no cognitive or academic deficits, it did show that the patients had an insufficiency in attention–based behaviour. Unfortunately, the value of this study is somewhat weak as a relatively small group of patients was used, and there was no mention of a control group with similar hospital admission times. A case has been reported from India in which a six–year–old boy developed bilateral facial nerve palsy (FNP) secondary to KD, and Lim et al’s (2009) subsequent paper suggested that FNP was an indicator of higher coronary damage.
The department of paediatric cardiology, Bristol, has continued to carry out investigations relating to psychological changes in patients with previous diagnosis of KD, in one such study (Carlton-Conway et al, 2005) MRI scans of seven children were performed, and the department concluded that although some evidence was of value, a more detailed and larger cohort of patients was needed in order to account for more reliable data (Carlton-Conway et al, 2005). Currently, all available research in this area appears to be rather vague though it does appear that there is a link to psychological changes in patients post–KD, though the current evidence is not strong enough to fully support this claim at present.
Future research
The aim of this article is to give paramedics some background knowledge of KD and the ability to recognise the main symptoms associated with this potentially fatal disease.
Although KD has been studied and researched since it was first discovered in 1967, there is still very little known about the disease, and from the studies and cases described in this article, many conclusions found appear to be based on hypothesis, though the combined use of high–dose aspirin and IVIG appears to be well researched, with some strong, supporting evidence for its use in the pre-hospital field. All pre-hospital literature for KD steers towards early recognition and transport with ECG monitoring. The lack of controlled studies showing good evidence into the benefit of pre-hospital pharmacological interventions restricts paramedics somewhat at the moment. CAA development is also well researched with evidence to support this, and due to the severity of this condition and the consequences of delayed treatment, it is important that paramedics understand the pathophysiology of this condition and the importance for A&E treatment.
It is hoped that with further research and studies, pre-hospital interventions will become available for paramedics and a more in-depth understanding of this condition will be made available, leading to better care for the patient.
