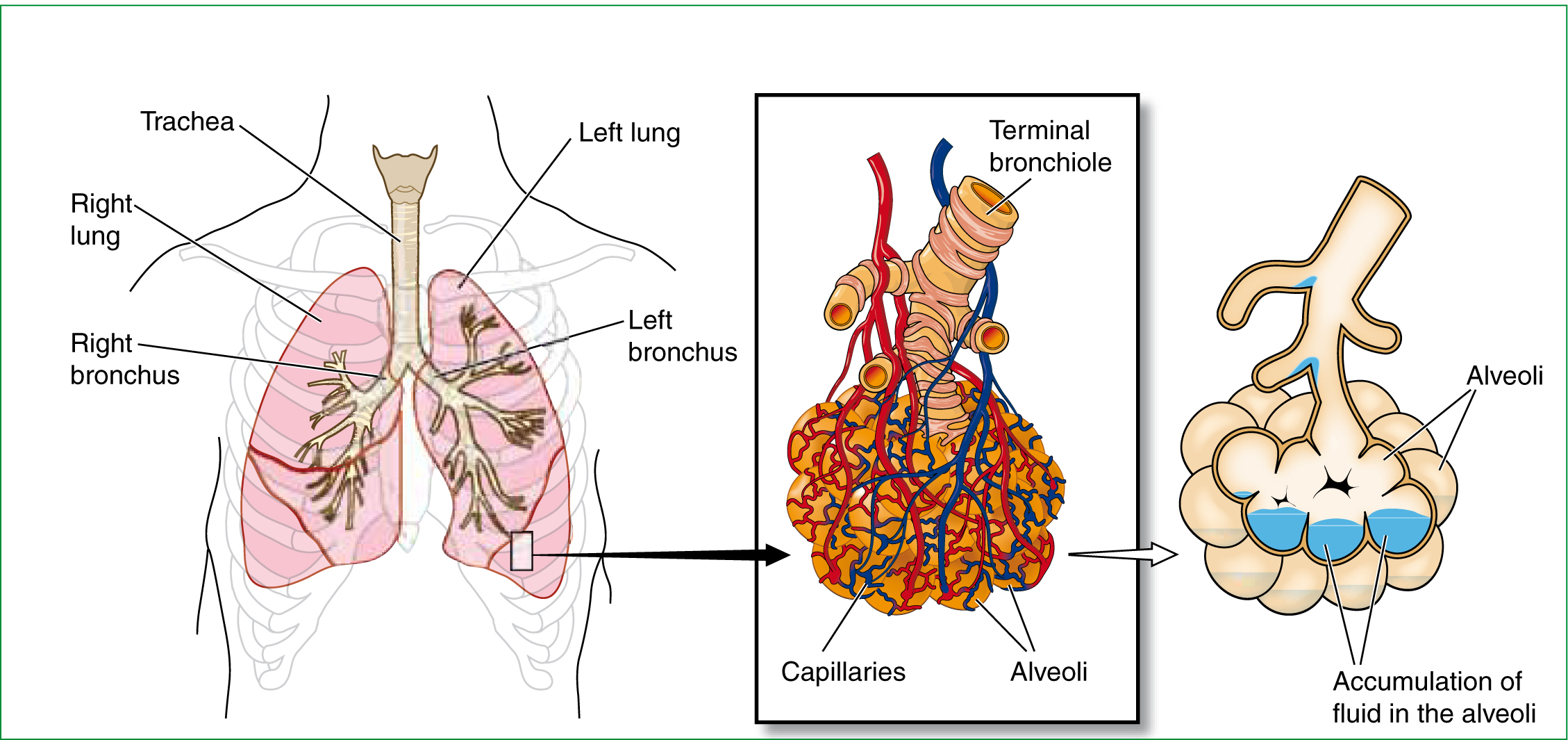
This is the second part in a series of two articles seeking to critique the potential of continuous positive pressure ventilation (CPAP) devices for acute cardiogenic pulmonary oedema (ACPO) (Figure 1). Part one focused on the in hospital literature—it revealed how the pathogenesis of acute heart failure leading to ACPO, when recognized, offers scope for paramedic intervention to reduce the spiral of deteriorating respiratory and cardiac function.
Adherence to current JRCALC guidelines offers optimum management. Despite this, when medical intervention has been exhausted, application of CPAP is increasingly advocated—as studies show, improved physiological variables, reduced need of endotracheal intubation (ETI), and palliation of breathlessness.
However, confounding factors such as variance in the standard of medical treatments, severity of illness and setting limit the ability to attribute observed benefits to its application. A more recent study (Grey et al, 2009) addressed many of these issues, and despite finding improvements in physiological variables and palliation of breathlessness, improved survival did not follow.
Prehospital use of CPAP may present unique opportunities, such as non-invasive means of supporting ventilation prior to ETI, palliation of breathlessness or earlier restitution of physiological variables leading to improved mortality. Therefore, part two aims to present the critique of the prehospital literature surrounding CPAP.
Methods
A comprehensive English language literature search of MEDLINE and CINAHL from 2000 to November 2010 was conducted using a broad search strategy. The subject heading ‘CPAP’ was used including the subheadings of: ‘pulmonary oedema’, ‘pulmonary edema’ ‘ACPO’, ‘heart Failure’ ‘pre hospital’ and ‘paramedic’ as key words. A second search was conducted using ‘non invasive ventilation’ as a subject heading along with subheadings above.
The author decided a priori that randomized control trials, met analysis and systematic review on in hospital CPAP would be deemed eligible. Case reports, letters, editorials and comments in addition to quantitative studies with a surveillance sample size of less than 25, were excluded. In hospital studies were limited to 10 for review. Review articles that contained no original data were ultimately omitted, but their bibliographies were hand searched.
Given relative scarcity in prehospital care literature, all articles regarding miscellaneous topics such as cost, compliance, psychosocial aspects and quality of life were selected for review. These were manually scanned for relevance and eligibility. The search yield is shown in Table 1.
| Term | And | CINAHL | Medline |
|---|---|---|---|
| CPAP | Pulmonary Oedema | 12 | 142 |
| Pulmonary edema | 43 | 142 | |
| ACPO | 3 | 4 | |
| Heart failure | 41 | 253 | |
| Paramedic | 0 | 4 | |
| Pre hospital | 2 | 5 | |
| Non invasive | ACPO | 1 | 4 |
| Ventilation | Heart failure | 2 | 173 |
| Pulmonary Oedema | 18 | 119 | |
| Pulmonary edema | 24 | 119 | |
| Paramedic | 1 | 4 | |
| Pre hospital | 1 | 49 |
| Study | Setting/clinician | Sample Size & method | Inclusions | Exclusions | Outcomes analyzed | Result |
|---|---|---|---|---|---|---|
| Plaisance et al (2007) | Urban France Physician | 124, single centre, RCT | Clinical symptoms without evidenc of aspiration or infection, SPO2 90% despite O2 therapy | COPD, asthma, stenotic valvular e disease, cardiovascular collapse or an impaired GCS | Effect of CPAP on Effect of CPAP on and ABG's. Incidence of ETI, inotropic support, and in-hospital mortality | CPAP had a greater effect than medical treatment on the clinical score (P=0.0003) and PaO2 (P < 0.0003). Six patients in ‘early CPAP’ group vs 16 in ‘late group needed ETI [P=0.01, Dobutamine was used only in the ‘late CPAP’ group (P <0.02) |
| Thompson et al (2008) | Pre Hospital, Canada online physician | 71 RCT, non-blinded | Severe respiratory distress, respiration rate>25/min Hypoxia | Respiratory arres or near arrest Respiration rate <8/min Periods of apneoa | Need for ETI out-of hospital. Mortality and length of stay | In usual care group, 17 ETI V 7 of CPAP group ( [OR] 0.25; 95% [CI] 0.09 to 0.73; adjusted OR 0.16; 95% CI 0.04 to 0.7; number needed to treat 3; 95% CI 2 to 12). Mortality was 12 in the usual care vs 5 in the CPAP group (unadjusted OR 0.3; 95% CI 0.09 to 0.99) |
| Hubble et al (2006) | Pre hospital USA | 215 non-randomize control group | All consecutive d patients presenting to EMS with a field impression of ACPO | Need for ETI, Mortality, Physiological parameters and self reported dyspnea score | Need for ETI 8.9% of CPAP V 25.3% control group (P=0.003), mortality in the CPAP group 5.4% vs 23.2% in control (P=0.000). CPAP resulted in improvement in resp rate (-4.55 vs -1.81; P=0.001), pulse rate (-4.77 vs 0.82; P=0.013), and dyspnea score (-2.11 vs -1.36; P=0.008) | |
| Hubble et al (2008) | Pre hospital and ED Physician and Paramedic | Univariate and multivariate sensitivity analysis | Published reports on pre hospital and emergency department CPAP | Cost of consumables, equipment, and training | The theoretical system would expect to use CPAP 4 times per 1000 patients saving 0.75 additional lives per 1000 cost of $490 per life saved | |
| Gardtman et al (2000) | Sweeden mobile coronary care unit (MCCU) | 158 observational study. 158 patients in each group | Consecutive patients with acute severe heart failure | ACPO, Physiological measures, mortality | On admission of the ambulance 60% had ACPO during period 1 vs 78% during period 2 (P<0.0001). On admission to hospital 93% during period 1 vs 76% during period 2 (P<0.0001). Mortality during the first year remained high during both periods (39.2% and 35.8%, P=0.64) | |
| Kallio et al (2002) | Finland mobile intensive care unit | 121 retrospective cohort study | Consecutive patients with a clinical picture of ACPO | Changes in SpO2, need for ETI or ventilatory support Possible morbidity associated with the CPA therapy | 2 CPAP patients (1.7%) received ETI, in the field six patients required ETI before hospital, 6 others later. CPAP P resulted in elevation in Spo2 (P < 0.0001) and reductions in respiratory rate (P < 0.0001), systolic Bp (P= 0.0002), and heart rate (P=0.0017) | |
| Kosowski et al (2001) | Urban EMS system USA, Paramedics | 240 Prospective case-series analysis | Respiratory rate > 25, labored, shallow breathing, and ‘presumed ACPO,’ | Treatment intervals, vital signs, complications, nee for ETI, and mortality | 15 patients met all 4 criteria for CPAP. d Four patients hypotenive or potential for airway compromise making CPAP inadvisable. Among the 11 remaining patients, median transport time was 20 minutes | |
| Frontin et at (2010) | France prehospital Physician | 124 RCT | >18 years with clinical symptoms of ACPO | Cardiovascular collapse or an Impaired GCS AMI, immediat need for ETI. History of gast surgery and vomiting | The primary outcome considered treatment success: respiratory ratee <25/min, SPO2>90% at 1-hour. Secondary endric points: death at 30 days. | Primary outcome 22 (35.5%) of 62 patients considered as treatment success in the usual care group vs 19 (31.7%) of 60 in the CPAP group (P = .65). Seven patients died within 30 days in the usual care group vs 6 in the CPAP group (P=.52) |
| Dieperink et al (2009) | Ambulance nurses, Pre hospital Netherland | 32 prospective cases | ACPO diagnosed on clinical signs and SpO2 | Physiological responses, clinical outcomes of the patients were collected from ambulance and hospital records, and ambulance nurses and patients received a questionnaire | With CPAP, median (IQR) SpO2 increased from 79% (69–94%) to 96% (89– 98%) within 20 min. The median (IQR) duration of BCPAP treatment was 26 min (21–32). The patients had no negative recollections of the treatment. Ambulance personnel were satisfied with the CPAP therapy. |
Prehospital management of ACPO
The JRCALC (2006) currently advises on the standards of practice for UK paramedics. Their advice on the management ACPO is aimed at improving oxygenation of the patient, reducing pre load and after load. This includes:
There are occasions when this standard treatment may not reduce respiratory distress, and the main risks of failure in medical treatment is demonstrated by half of patients with ACPO being admitted to hospital showing hypercapnia and severe acidosis (Masip et al, 2007). Patients close to respiratory failure may then require rapid initiation of ventilation support through ETI and mechanical ventilation (Ursella 2007), with the main goals to improve oxygenation, and permitting a sufficient period for medical therapy to decrease pulmonary vascular congestion (Mehnta et al, 2004).
Prehospital ETI
Despite its role in prehospital care, there is much debate whether prehospital ETI is achieving its intended goals. Lecky et al (2009) undertook a Cochrane review of emergency ETI for acutely ill and injured patients. 452 trials were reviewed, three RCT's were deemed eligible. The review found no difference between ETI and other airway securing strategies for reducing mortality. In hospital ETI is generally performed on fasted, optimized patients, sedated by anaesthetists who are expert in airway management, therefore severe complications are rare (Cheney et al, 2006).
Conversely, the prehospital phase of care is recognized as being a high-risk environment for the administration of drugs utilized in sedation prior to ETI (Bredmose et al, 2009). Subsequently, sedation prior to ETI is not an option for most UK paramedics. This presents challenges when dealing with ACPO requiring ETI on non-fasted, awake or combative patients (Gunning et al, 2009).
The potential pitfalls to ETI include: bronchotracheal, and oesophageal perforation or injury, pneumothorax, pneumonitis (aspiration) and acute respiratory distress syndrome (ARDS) (Mort, 2004; Wang, 2008). Griesdale et al (2008) conducted a cohort study of 136 ETI patients; the overall risk of complications was 39%, which included: severe hypoxemia (19.1%), severe hypotension (9.6%), oesophageal intubation (7.4%) and frank aspiration (5.9%).
Unrecognized oesophageal intubation is the pitfall which has the most fatal implications, as it deprives a patient of their airway, resulting in ventilation failure and hypoxaemia. Studies of paramedics have found ETI tube misplacement rates ranging from 5.8% to 25% ( Jemmett et al. 2003; Jones et al, 2004). Jemmett et al (2003) evaluated 109 paramedic ETI's they found greater than 25% of ETI tubes were misplaced. Katz and Falk (2001) conducted a study of 108 paramedic ETI's, similar tube misplacement rates of 12%, were revealed, indicating that out-of-hospital ETI is potentially prone to detection bias where errors go undetected.
The debate surrounding prehospital ETI is beyond this article, and whilst the papers presented above are based on dated studies within a non–UK setting, they do offer a glimpse of potential pitfalls. Many of these pitfalls present to all levels of practitioner, however the absence of the ability to sedate prior to ETI offers little option to the paramedic faced with ACPO in a patient close to respiratory failure. Likewise, the practical implications of assisting ventilation with bag valve and mask in a moving ambulance fails to offer a realistic optimum for maintaining ventilation in ACPO.
Prehospital literature
Gartman et al (2000)
Gartman et al (2000) evaluated the outcome following an introduction of intensified treatment in the ambulance of patients with AHF. The study had no randomization or blinding. Data were collected from patients during phase one which included standard treatment, and phase two, following the introduction of CPAP, Nitrates and Frusemide. While a statistically significant reduction in pulmonary oedema of 93% during period 1 vs 76% during period 2 (P<0.0001) was achieved, as with earlier studies, it tells us little in terms of which therapy is most effective: CPAP, nitrates or Frusemide. Gartdman also failed to show a reduction in mortality.
Kosowski (2000)
Kosowski (2000) conducted a prospective case-series analysis on the use of a CPAP for ACPO by paramedics. While a mean rise in saturation pressure of oxygen (SPO2) from 83.3% to 95.4% was recorded, and this study highlights the potential for prehospital use of CPAP by finding no technical difficulties, claims that CPAP may avert the need for ETI are unjustified, as seven of the nineteen patients eventually required ETI.
Kalio et al (2003)
Studying an EMS system in Helsinki where CPAP had been routinely applied for the past ten years, Kalio et al (2003) sought to describe its pre hospital use on 121 patients with acute severe pulmonary oedema. They demonstrated significant reductions in Sp02 (P<0.0001), respiratory rate (P<0.0001) and systolic blood pressure (P<0.0002).
The diagnosis of ACPO was made by a physician staffed ambulance, based on clinical symptoms. Physicians are rare in UK prehospital care, and as they had a wide range of drugs available, many of which are beyond the scope of UK paramedic practice. This presents limits to the transferability into current UK practice, and such results should be viewed with caution.
Plaisance (2007)
Plaisance (2007) sought to assess the benefit of CPAP as a first line treatment of ACPO out-of-hospital, through a single centre, prospective, randomized, intention-to treat clinical trial of 176 patients. They found immediate application of CPAP to significantly improve the physiological variable of PaO2 (P=0.0003), and also significant improvement in relief of symptoms in dyspnoea clinical score (P=0003). However, they do not offer measures to validate scoring of symptoms, thus it appears subjective. During the study period, one patient received ETI early in CPAP group versus eight in the late group (P=0.01), yet as it was non-blinded, investigators may have delayed intubation.
Once again, the protocol of this trial does not reproduce the UK prehospital practice, as the ambulance response always included a physician. 25.26% of patients in the control group required ETI vs 8.92 in the CPAP group (P=0.03), and the mortality rate of those with confirmed ACPO was 5.55% in the CPAP group vs 25% in control (P=0.001). There was lack of heterogeneity between groups, patients in CPAP group were younger (P=0.03), both the incidence and prevalence of heart failure increase steeply with age (NICE, 2005), therefore the CPAP group may have included subjects with a better cardiac function and prognosis.
Patients in the CPAP group received lower mean dose of Furosemide (P=0.008), Morphine (P=0.000) and Nitroglycerine (P=0.000), this also points to the possibility that CPAP subjects presented with a better prognosis, requiring less medical intervention.
Thompson (2008)
Through a prospective, non blinded RCT, including seventy one patients, Thompson (2008) sought to determine whether out-of-hospital CPAP reduced need for ETI in patients in severe respiratory distress, where paramedics assessed as requiring some degree of positive-pressure ventilatory support. 17 of 34 (50%) patients received ETI in the usual care group vs 7 of 35 (20%) in the CPAP group (unadjusted OR 0.25; 95% CI 0.09 to 0.73). Paramedics were trained to facilitate non– cardiac arrest intubation, with topical anaesthesia and small titrating doses of Midazolam.
Whilst this is out of the scope of UK paramedics, it did not involve full sedation as in other studies— therefore patients would have presented as they do for UK paramedics prior to ETI, as non-fasted, awake or combative patients (Gunning et al 2009) in a critical state, near to total respiratory failure.
Thompson (2008) encountered similar difficulties to other investigators in studying CPAP. Blinding would not have been possible, and given that ETI is the primary outcome, they provide no objective criteria for ETI, relying on a degree of paramedic judgment, which potentially bias the study results.
No inferential statistics were used to compare the characteristics of both groups, yet the saturation pressure of oxygen (SpO2) was 75% in the standard group vs 81.5% CPAP, and the pulse rate was 121.2 in the standard group vs 112.4 (25.2) in CPAP.
This demonstrates that the CPAP group presented with better physiological variables and less respiratory distress, thus they had a potentially more favourable outcome without the application of CPAP. As with other studies, Thompson (2008) does not reassure the reader that the potential confounding factor such as co-interventions were controlled for.
Diagnosis of ACPO
Paramedic diagnostic accuracy of ACPO when correlated to the discharge diagnosis ranges from 77 to 86% (Pozna, 2003; Giuseppe et al, 2008; Bosomworth 2008). In the UK, Jenkinson et al (2008) found that less than 50% of patients with ACPO were identified in their sample of 1115 patients. The sensitivity of paramedics in diagnosing ACPO was 32.4% (22.0—44.3%) and specificity 96.8% (95.5—97.7%), indicating that many patients may be denied appropriate treatment.
Jenkinson et al (2008) also measured positive and negative predictive values, Greenhalgh (2001) advocates their use in directly ruling a particular diagnosis in or out. A positive and negative predictive value of 38.3% (26.1—51.8%) was found, indicating that 61.7% of those with a positive diagnosis could have been treated inappropriately.
The clinical significance of misdiagnosis is demonstrated in Hubble et al (2006) who compared the effectiveness of CPAP with standard pharmacological treatment in the management of ACPO. The control group received standard treatment including oxygen, nitroglycerine, morphine and furosemide, the intervention group received CPAP in addition to the standard treatment. Although only 24% received a diagnosis other than ACPO, the leading misdiagnosed conditions were COPD, acute respiratory failure and pneumonia, in line with other studies (Bosomworth, 2008; Giuseppe et al, 2008; Dieperink et al, 2009).
The treatment regime Hubble (2006) used for ACPO included the use of morphine, yet retrospective studies have shown morphine to be harmful in respiratory disease, increasing ETI rates (Peacock et al, 2005). ETI rates between CPAP and control were 8.92 and 25.26 (P<0.005) respectively, however the control group were given significantly higher doses of morphine than the CPAP group 1.22 mg vs 5.00 mg P(0.000) respectively. Arguably, the increased ETI rates in the control group may have been due to increased use of morphine and detrimental effects on COPD.
Conclusion
When standard paramedic treatment fails to reduce respiratory distress in ACPO, the paramedic is faced with limited options, leading to respiratory failure currently being managed by ventilation support through bag valve mask, ETI and mechanical ventilation. Despite this, the prehospital phase of care is recognized as being a potentially high-risk environment for sedation prior to ETI, resulting in few UK paramedics having the option to sedate prior to ETI.
The potential benefits of ETI for ACPO are mitigated by this in ability to perform ETI prior to respiratory failure, resulting in ventilation being supported through bag valve mask.
CPAP offers the benefits of adjunctive airway support, allowing temporary oxygenation and ventilation for respiratory distress in lieu of ETI. JRCALC appear to advocate adoption of CPAP into prehospital practices for ACPO, citing studies suggesting its feasibility and expert opinion. Despite this, the studies presented are dated and more recent studies such as 3cpo (Grey et al, 2009) offers scope for reviewing current thinking.
Co-interventions such as the use of nitrates, statistically significant differences in demographics between groups, and skill level of responder, all present difficulties in attributing observed benefits to the application of CPAP. Recent prehospital studies however have found significant improvements in PaO2, relief of dyspnoea, mortality, and reduced ETI rates following application of CPAP. While encouraging, many of the results are based on a physician response, and as paramedic diagnostic accuracy of ACPO ranges from 77% to 86%, this presents questions over its transferability into UK paramedic practice. A large proportion of the literature points to the benefits of CPAP for ACPO, however controlling for confounding factors such as co-interventions and skill level are equally consistent in demonstrating difficulties in studying CPAP. The 3Cpo trial robustly reveals that whilst improvements on physiological parameters can be demonstrated, increased survival does not naturally follow.
We cannot be sure that the benefits of CPAP are not lost or gained with earlier application in the prehospital environment. Factors such as transport pressures, diagnostic uncertainty, equipment failures, and limited clinical expertise, may limit its use. Conversely, the palliative effects on relief of breathlessness, and earlier intervention on physiological variables and reducing the need to ETI may present opportunities distinct to the prehospital environment.
UK paramedic practice is faced with a decision around ventilatory support for ACPO. It is clear that those close to total respiratory failure who stand to benefit most from ETI are receiving sub optimal management by use of bag mask valve on moving ambulances. Therefore unless the scope of paramedic practice seeks to include this skill, prehospital CPAP may reveal opportunities in the management of ACPO yet to be demonstrated in the hospital. A UK based prehospital study of CPAP is urgently needed.
