LEARNING OUTCOMES
After completing this module the paramedic will be able to:
Respiration can vary in numerous ways as a result of different underlying pathologies. Examples include tachypnoea and hyperventilation. Tachypnoea is defined as the respiratory rate of an individual exceeding the expected value for their age group while hyperventilation is overbreathing above the required rate for carbon dioxide elimination resulting in respiratory alkalosis (Whited and Graham, 2019).
Hyperventilation syndrome (HVS) is one of many conditions that present with an increased respiratory rate among other symptoms. The symptoms of HVS were first recognised during the American Civil War when DaCosta (1951) described Union Army soldiers as having an ‘irritable heart’ (Evans, 2005). Kerr et al (1938) were the first to use the term HVS and related it to the presentation of hyperventilation associated with anxiety or panic. Because the characteristics of HVS are poorly defined, the term has been misused, and is often used interchangeably with panic or anxiety disorders.
Defining HVS is controversial because of the lack of research on the subject. Schildkrout (2005) defines hyperventilation as a type of panic disorder whereas Lum (1975) claims panic is the cause of hyperventilation where no physiological cause can be found. Folgering (1999) defined HVS as the minute ventilation of an individual exceeding their metabolic demands.
Nowadays, an alternative term such as behavioural breathlessness or psychogenic dyspnoea may be more appropriate (Kern and Rosh, 2016). Derbyshire Community Health Services NHS Trust (2012) defines HVS as a collection of physical and emotional symptoms that arise from breathing too quickly.
HVS is thought to have both a chronic and an acute form. Waites (1978) believed that the acute form accounted for 1% of patients with this syndrome. Saisch et al (1996) believe the label of HVS in a patient with hypocapnia is not beneficial to the person's recovery and therefore suggested that the term be abandoned. They understood that hyperventilation occurred because of a complex interaction between multiple organ systems and that the label of HVS prevented investigation into the original cause.
Pathophysiology
Blood acidity, measured as a pH, is determined by the concentration of hydrogen ions (H+) present. Blood is comprised of 55% blood plasma, of which at least 90% is water (Institute for Quality and Efficiency in Health Care, 2015). When dissolved in water, carbon dioxide becomes part of an equilibrium in which the forward reaction produces carbonic acid (H2CO3). Once formed, carbonic acid becomes part of a further equilibrium through dissociation, producing bicarbonate (HCO3–) and hydrogen (H+) ions. This equilibrium is the basis for homeostatic balance of blood pH.
Both oxygen and carbon dioxide can chemically bind to haemoglobin for transportation around the body (Marieb and Hoehn, 2016). Haemoglobin also acts as a buffer, collecting excess hydrogen ions which would otherwise cause acidosis.
Figure 1 shows the oxygen-haemoglobin dissociation curve—a sigmoid curve—and the variables that can cause it to shift to the left and right, influencing affinity at different partial pressures (Broaddus et al, 2016). Haemoglobin's affinity for oxygen is influenced by the levels of carbon dioxide and hydrogen ions, which change as a result of hyperventilation and the resulting hypocapnia; this is called the Bohr effect.
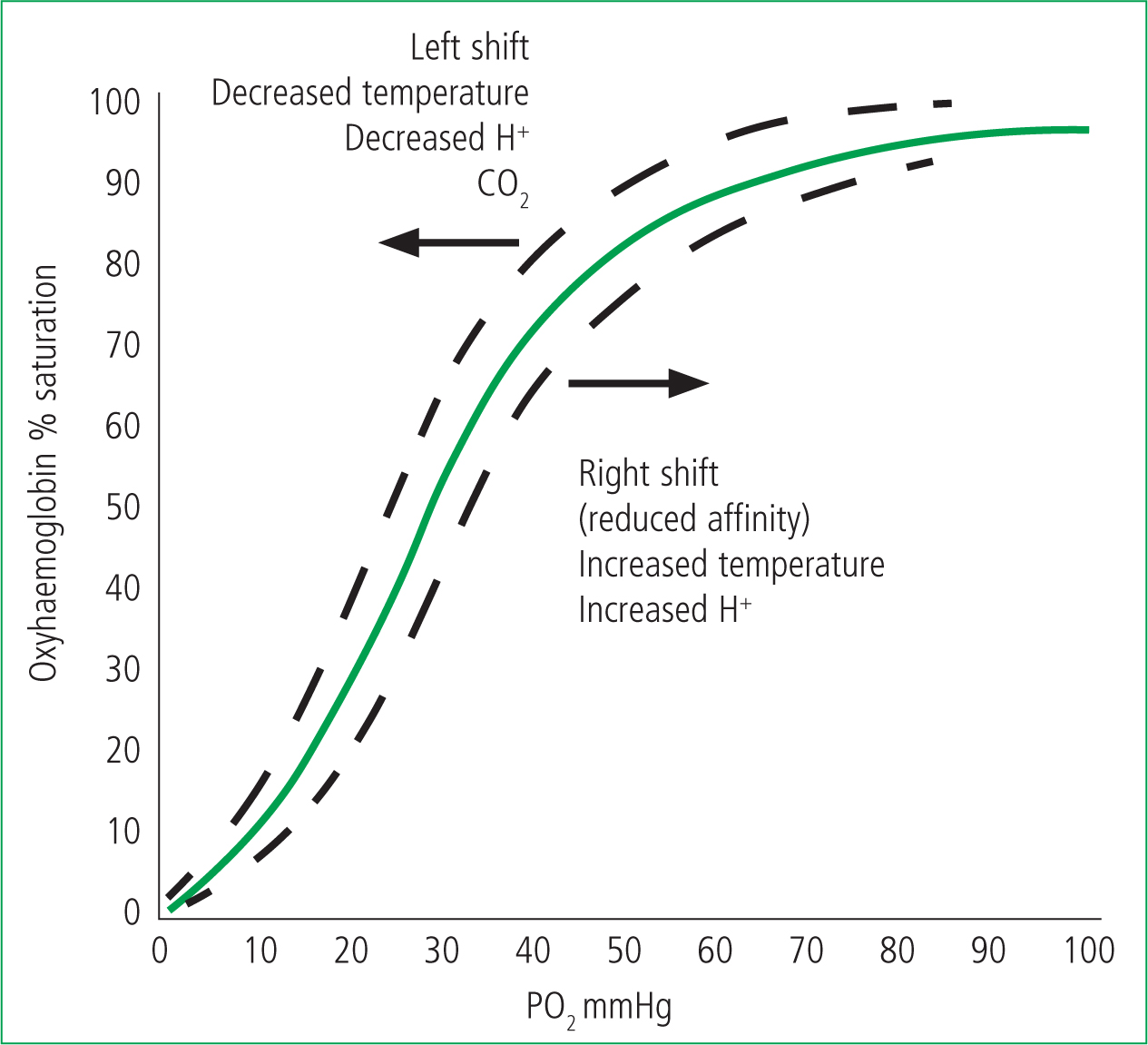
Hyperventilation leads to excessive exhalation of carbon dioxide, and a left shift in the oxygen-haemoglobin dissociation curve, resulting in respiratory alkalosis (Patel and Cooper, 2018). This in turn leads to an impaired release of oxygen within the peripheral tissues, causing the irregular firing of nerves and therefore paraesthesia.
Because hypocapnia occurs during hyperventilation, the vasoconstrictive effects of carbon dioxide are reduced (Cipolla, 2009). This leads to a relative hypotension and an estimated reduction in cerebral perfusion pressure (CPP) of 30–40%, which is more noticeable in patients who have autonomic failure (Pickering, 2000). This contributes to the most frequently reported symptom of dizziness in patients presenting with hyperventilation (Evans, 2005). To compensate for the reduction in blood pressure, the heart rate and stroke volume increase (Marieb and Hoehn, 2016). Tachycardia is a frequently experienced symptom associated with both anxiety disorders and HVS, and often presents as palpitations.
Presentation
The signs and symptoms of HVS vary a great deal between patients, with some experienced frequently while others are rarely present. These symptoms are thought to be caused by the metabolic alkalosis and alterations in blood flow that result from hyperventilation. A wide range of symptoms can be noted across the systems of the body (Table 1).
| General | Fatigue, nausea, diaphoresis |
|---|---|
| Neurological | Headache, visual disturbances, dizziness, paraesthesia, syncope |
| Cardiovascular | Palpitations, tachycardia, chest pain |
| Gastrointestinal | Dysphagia, epigastric discomfort, belching, dry mouth, flatulence |
| Psychological | Altered concentration, anxiety |
| Respiratory | Tachypnoea, chest tightness |
| Musculoskeletal | Tremors, weakness, tetany, muscle pains |
Although there is little consistency regarding the diagnosis and definition of HVS, symptoms are often similar. The most commonly experienced feeling is of dizziness or light-headedness. Others include paraesthesia in the extremities and muscle cramps, and seizures have been reported in the most extreme cases. Peripheral and central tetany are rare, and have been recorded in a small minority of patients. Schildkrout (2005) reported derealisation and depersonalisation; however, no other sources have reported this as a symptom.
The dizziness that is often reported is likely to result from a combination of the reductions in blood pressure and CPP. When this occurs, the body's blood supply centralises to ensure oxygen delivery to essential organs (Marieb and Hoehn, 2016). Assuming there is no underlying pathological cause, these symptoms resolve upon resuming eupnoeic breathing once the excess in exhalation of carbon dioxide has been reversed (Evans, 2005). The sensation of a dry mouth results from rapid breathing through the mouth (Tavel, 1990).
Diagnosis
HVS has both chronic and acute presentations. The chronic form is primarily diagnosed by the patient's GP after extensive testing. The acute form is encountered significantly more often in the out-of-hospital setting. There is a lack of prognostic criteria for HVS as there is much controversy among the medical community regarding which procedures allow for an accurate diagnosis.
One diagnostic method for chronic HVS is the hyperventilation provocation test. This involves the patient voluntarily overbreathing for long enough to induce hypocapnia. At this point, if the previously experienced symptoms return, the result is determined to be positive. Hornsveld and Garssen (1996) found that the hyperventilation provocation test gained a positive result in 66% of patients and 60% of a control group. Because of the low specificity of this test, it has largely been discounted, with the scientific background surrounding the hyperventilation provocation test highlighting its flaws. The theory that symptoms will be reproduced upon voluntary hyperventilation is supported by the physiology of overbreathing regardless of diagnosis. This test was also discounted as a diagnostic tool when Howell (1997) found that the reproduction of symptoms was not reliant on a fall in carbon dioxide, thereby rendering the test invalid.
An alternative method of diagnosing chronic HVS is the Nijmegen questionnaire. This is a list of symptoms relating to respiratory distress, which are scored from 0 to 4 regarding the frequency at which they are experienced. A score above 23 out of a maximum 64 points indicates HVS. This questionnaire has been found to differentiate between those with HVS and those who do not have HVS. Van Dixhoorn and Duivernvoorden (1985) found it had a sensitivity of 91% and a specificity of 95% in relation to the clinical diagnosis of chronic HVS. D'Alba et al (2015) conducted similar research, comparing paediatric patients with and without asthma using the Nijmegen questionnaire to assess for HVS, and found it be an accurate tool.
One of the more rudimentary diagnostic methods for chronic HVS revolves around the exclusion of any organic (physiologic) cause (Lum, 1975). This has been used to diagnose both the chronic and acute forms and can be conducted in the out-of-hospital setting. It involves assessing all organ systems in depth for any pathologies that may result in hyperventilation. Only when all other differentials have been discounted can HVS be diagnosed.
Often, when no cause was found, patients with these symptoms were misdiagnosed as having an anxiety-related issue. As a result, they were often not given appropriate treatment or guidance on how to manage their condition. This procedure has generally been discounted, as it does not identify the cause of dysfunctional breathing. However, it is still used in the out-of-hospital setting.
When paramedics are presented with a patient who is experiencing some of the aforementioned symptoms prehospitally, it is essential to establish the cause by excluding other differentials. Conditions that present with hyperventilation or tachypnoea include infection, pulmonary embolism and diabetic ketoacidosis. If the increased respiratory rate is caused by an underlying pathology for which the body is attempting to compensate, reversing the abnormal breathing pattern can cause further harm. It is therefore important to discount other causes before starting treatment.
The characteristic low levels of carbon dioxide in a hyperventilating individual can be measured using capnography. Capnography is a non-invasive method of measuring carbon dioxide and can provide information on ventilation and perfusion (Long et al, 2017). It typically produces a quantitative value and a graphic representation of carbon dioxide levels (Brandt, 2010). This quantitative value is referred to as end-tidal carbon dioxide (ETCO2) and is the level of carbon dioxide exhaled.
During hyperventilation, the capnography waveform will be at a higher frequency than the expected range for the individual. The amplitude of the waveform, which represents ETCO2, is also lower than in eupnoeic breathing. When presented with hyperventilation, capnography can be used alongside patient assessment but it is not a standalone test.
Treatment
Once the cause of hyperventilation has been determined as HVS, various treatments that have been formalised with the intention of reducing the frequency and severity of hyperventilation attacks can be given (Laurino et al, 2012). These treatments vary from preventive measures to techniques to use when an attack occurs.
Respiratory rehabilitation has been used to educate individuals on methods to reduce their breathing rate. This involves training in techniques such as diaphragmatic breathing or hypoventilation to combat overbreathing (Derbyshire Community Health Services NHS Trust, 2012). Diaphragmatic or deep breathing helps reverse any deviations from eupnoeic breathing. Often when an individual hyperventilates, they use accessory muscles in their upper chest. This is an ineffective method of breathing and results in muscle tension which can increase the overall feeling of anxiety, a potential cause of the attack. Ensuring the diaphragm is engaged in the most efficient manner can distract a patient from potential emotional triggers. It actively ensures that deeper and slower breaths are taken, combatting the decline in carbon dioxide.
Swift et al (1988) found that inhalation via the nose and exhalation via the mouth can also help reduce the effects of hyperventilation. The nose acts as a filtration system and both moistens and humidifies the air before it comes into contact with the lungs. When patients inhale through the nose, the lower lobes of the lungs are stimulated to a greater degree than when they inhale through the mouth, which increases the volume of the lungs and overall amount of oxygen distributed to the body. The lower lobes also contain a large quantity of parasympathetic receptors which, when stimulated, will help reduce excitability thus lowering the desire to inhale. In contrast, the upper lobes of the lungs are stimulated by mouth breathing which stimulates a sympathetic response. This encourages hyperventilation and can induce the fight-or-flight response.
An additional acute treatment for HVS is the well known practice of breathing into a paper bag. This means any exhaled carbon dioxide is ‘stored’, increasing the amount readily available to inhale. Brouhard (2019) thought that this rebreathing exhaled air increases carbon dioxide intake, thereby correcting the imbalance created by hyperventilation. This should reduce metabolic alkalinity and so eliminate symptoms. This technique must not be performed for any prolonged period on in an individual who is not experiencing hyperventilation as a result of anxiety, as it could fail to have the desired effect and increase levels of carbon dioxide above average limits. This technique for correcting ineffective breathing techniques must be used only after all pathological causes have been excluded. If a patient is hyperventilating to compensate for metabolic acidosis from an underlying cause, correcting this can have serious repercussions.
The Association of Ambulance Chief Executives (AACE) and the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) produced an algorithm for the assessment and management of HVS that begins with assessing the patient's baseline observations and correcting any of these as problems are identified (AACE and JRCALC, 2016). A rapid transfer must be made when a patient is experiencing an attack with any time-critical features such as cyanosis or a reduced level of consciousness. This transfer to hospital must be performed when it is their first hyperventilation episode or if ‘symptoms have not settled or re-occur within 10 minutes' (AACE and JRCALC, 2016). If the patient has a personalised care plan and can be left in the care of a responsible adult, non-conveyance can be considered. The recommended treatment for an acute episode involves coaching the patient in breathing and providing reassurance. Where possible, the patient should be moved from the source of any potential anxiety; supplementary oxygen is recommended only if hyperventilation is accompanied by hypoxaemia.
Emergency prehospital care
The lack of published research into HVS, particularly within the prehospital setting, may result from a belief that it will have little impact. Clinicians already use the skills in assessing a patient and coaching in breathing that would be required in the management of acute HVS.
Being aware of the alternative differentials that present in a similar way but have a more dangerous pathology may be more important. For example, pulmonary embolism, severe infection or an aspirin overdose all present with an increased respiratory rate and therefore produce the biochemical symptoms, including paraesthesia and dizziness. The AACE and JRCALC guidelines (2016) suggest the most appropriate method to use in assessing this group of patients in the out-of-hospital setting.
Medical attention is sought by 32% of people experiencing panic attacks, which results in extensive and expensive examinations (Coley, 2007). Because of their variety of symptoms, including chest pain and paraesthesia, patients with HVS often seek help for fear their symptoms may represent a more sinister pathology. Wilson et al (2017) found a prehospital diagnosis rate that was near perfect with paramedics and emergency medical technicians. With this high specificity and sensitivity surrounding the acute diagnosis of HVS in the prehospital setting, the option for non-conveyance is pertinent. This would help reduce the economic burden on hospitals as well as patients' anxiety.
Is HVS dangerous?
Although many individuals who experience an HVS episode fear a sinister pathology and seek medical attention, general sources concur that an attack of HVS is unlikely to cause any significant or long-term damage. Although distressing and overwhelming in the moment, the symptoms are in response to hyperventilation. Once eupnoeic breathing recommences and the carbon dioxide debt has been reversed, all symptoms resolve. Although wildly different, there is a consistency within the nature of the experienced symptoms that can be explained by the biochemical alterations that result from overbreathing.
Discussion
After a review of the current research, it may be suggested that there is no exact cause for HVS. As a result, no overall conclusion can be drawn to suggest an ideal diagnostic tool or potential treatment methods. Evidence of HVS often originates from anxiety-related disorders. This often delves into the physical reasons an individual would experience these symptoms, including hyperventilation. However, no research considers the possibility that these ideas are interlinked.
Anxiety and hyperventilation have been shown to be related and it is often thought that the anxiety causes the hyperventilation. However, it may be that, rather than a cause-effect relationship, this is more correlational. Hyperventilation occurs, whether it is of a known pathology or of no apparent cause, and this triggers anxiety. This cycle continues until the individual is in an intense state where they are no longer able to control either the hyperventilation or the anxiety, which would be manageable separately. When they occur simultaneously, the overall result is so overwhelming for the body that it enters a symptomatic loop.
There are significant gaps within the research surrounding HVS with controversy arising from differing opinions. Additional research is required to fill these gaps, with an emphasis on relevance in out-of-hospital settings.
As the scope of prehospital medicine expands, the degree of understanding of pathologies needs to be increased to mirror these changes, which is not possible without additional research.
Conclusion
Different sources give varying definitions of HVS, which has resulted in a poor understanding of the condition and terms often being misused. Collating information to provide a conclusive definition may improve understanding within the medical and non-medical communities.
HVS is a collection of physical and biochemical reactions to an unnecessarily increased respiratory rate that occurs because of an unknown or benign aetiology, often triggered by anxiety in the absence of other external factors. Symptoms include dizziness, headache and anxiety.
A significant lack of research surrounding the cause of HVS has resulted in controversy regarding the ideal diagnostic tool and treatments. It is still unknown whether HVS occurs as a result of an underlying pathology or is anxiety related. More research is essential to allow tools to be created to improve treatment of patients suffering from both acute and chronic HVS.

