In 2010, the International Liaison Committee on Resuscitation (ILCOR) recommended that rescuers deliver cardiopulmonary resuscitation (CPR) in cycles of 30 chest compressions and 2 ventilations (30:2) at a rate of 100 compressions per minute with a compression depth of 4-5 cm (40-50 mm). The National Resuscitation Council and Joint Royal College Ambulance Liaison Committee both recommend a compression depth of 5-6 cm. Given this change to CPR rates from the previous 15:2 to 30:2 (ILCOR, 2005), there is also now greater emphasis on pushing faster and deeper with minimal interruptions. However, it is known that the effective delivery of CPR is physically demanding, requiring quick, consistent application of intense forces which has led to speculation surrounding rescuer fatigue and quality of compressions. It has also been demonstrated by several investigators that physical fatigue in the rescuer occurs as soon as one minute after commencing compressions and most times the rescuer is unaware that fatigue has reduced their compression effectiveness (Gutwirth et al, 2009).
Most studies investigating rescuer fatigue in CPR have been performed in simulated settings using mannequins (Gutwirth, et al, 2009). With the increasing evidence of rescuer fatigue in CPR, an emerging body of knowledge now exists for qualified health professionals experienced in CPR (Gutwirth, et al, 2009). However little is known about rescuer fatigue in students, specifically undergraduate paramedic students when performing CPR. Although recent studies have commented on various aspects of improving basic CPR (i.e. faster and deeper compressions, minimal interruptions and rotating every 2 minutes) the fundamental principle of physical fatigue affecting the provider has received little attention (Hightower et al, 1995).
Given this, physical fatigue should not be dismissed given the deterioration of quality chest compressions over time (Lucia et al, 1999; Ashton et al, 2002; Riera et al, 2007). Therefore the purpose of this pilot study was to determine the level of work intensity and fatigue as assessed by ratings of perceived exertion, heart rate and quality of chest compressions among undergraduate paramedic students during simulated CPR.
Method
Design
This was an observational pilot study of CPR fatigue with a cohort of undergraduate paramedic students using a mannequin model.
Participants
Participants eligible for inclusion in the study were second year undergraduate paramedic students enrolled in the Bachelor of Emergency Health (Paramedic) at Monash University.
Outcome measures
Heart rate and rating of perceived exertion (RPE)
Heart rate was used to indicate levels of physical exertion during CPR. Each participant wore a wireless heart rate monitor incorporating a chest mounted sensor and transmitter belt (Accurate) and watch receiver (Pulse Sonic-K9132, Australia). The Borg scale is a rating of perceived exertion (RPE) which is a widely used standardized tool to quantify and evaluate individuals’ exercise tolerance and level of exertion during graded exercise testing (Chen et al, 2002; Lamb et al, 1999). It comprises of a 15-point graded scale with numbers ranging from 6 to 20, along with descriptive words which are included with every other number and range from very, very light at 7 to very, very hard at 19 (ACSM, 2010). Subjects indicated their momentary perception of their exertion intensity at two minute intervals while CPR was being performed. In this pilot study, the Borg Scale, as an RPE, was used in accordance with its design purposes (ACSM, 2010).
Chest compression rate and depth
Chest compression rate and depth were recorded during CPR using a Resusci Anne CPR Skillreporter (Laerdal Medical Corporation, Stavanger, Norway). A laptop computer connected to the Skillreporter continuously recorded data on compressions using the Laerdal PC Skillreporting System software. The mannequin was calibrated to provide data for adequate CPR quality which was defined as 100 compressions per minute at a depth of 40-50 mm. For the evaluation of fatigue, the 20 minute period was divided into 5 segments of 2 minute periods to assess the number of chest compressions, compression rate and compression depth. Additionally, participant's heart rate and RPE, using the Borg scale were recorded at 2 minutes, then in 4 minute intervals. A 2 minute rest period was recorded and used as a baseline marker to compare the other 2 minute periods throughout the 20 minutes of CPR.
Procedures
All participants completed a purposefully designed questionnaire which included their age and gender, the amount of hours of exercise per week as well as prior CPR experience. All participants were provided with an explanatory statement of the study and gave their consent by signing a consent form before the participating in the study. The ILCOR CPR guidelines were followed with a 30:2 chest compression: ventilation ratio with rescuers changing every 2 minutes on the investigators command, after a baseline heart rate was obtained from the participant.
Each pair of rescuers consisted of a participant and non-participant (BW). Each time the participant completed 2 minutes of chest compression, heart rate was recorded and the participant was asked to rate their perceived exertion using the Borg Scale. This procedure was repeated until the 20 minutes of CPR was completed.
Analysis
Data analysis was undertaken using SPSS (Statistical Package for the Social Sciences Version 17.0, SPSS Inc., Chicago, Illinios, USA). Descriptive statistics were used to report the demographics, means and standard deviation (SD), median, and range was used to report the compression rate, compression depth, and compressions per minute. A oneway ANOVA or t-test was used to compare the differences between the genders and age groups. All tests are two tailed, unless otherwise stated, with the results considered statistically significance if the P value is <0.05, all confidence intervals (CI) are 95%.
Ethics
Ethics approval for this study was granted by the Monash University Human Research Ethics Committee.
Results
Seven students participated (2 males, 5 females). Five students between 21 and 25 years of age, the others were <21 years of age. Of the 7 participants, 85% reported (n=6) planned exercise between 1-5 hours of exercise per week, the remaining reported planning exercise between 6-10 hours per week. The majority of participants 85% (n=6) had not previously performed CPR on a human patient.
Heart rate (HR) and rating of perceived exertion (RPE)
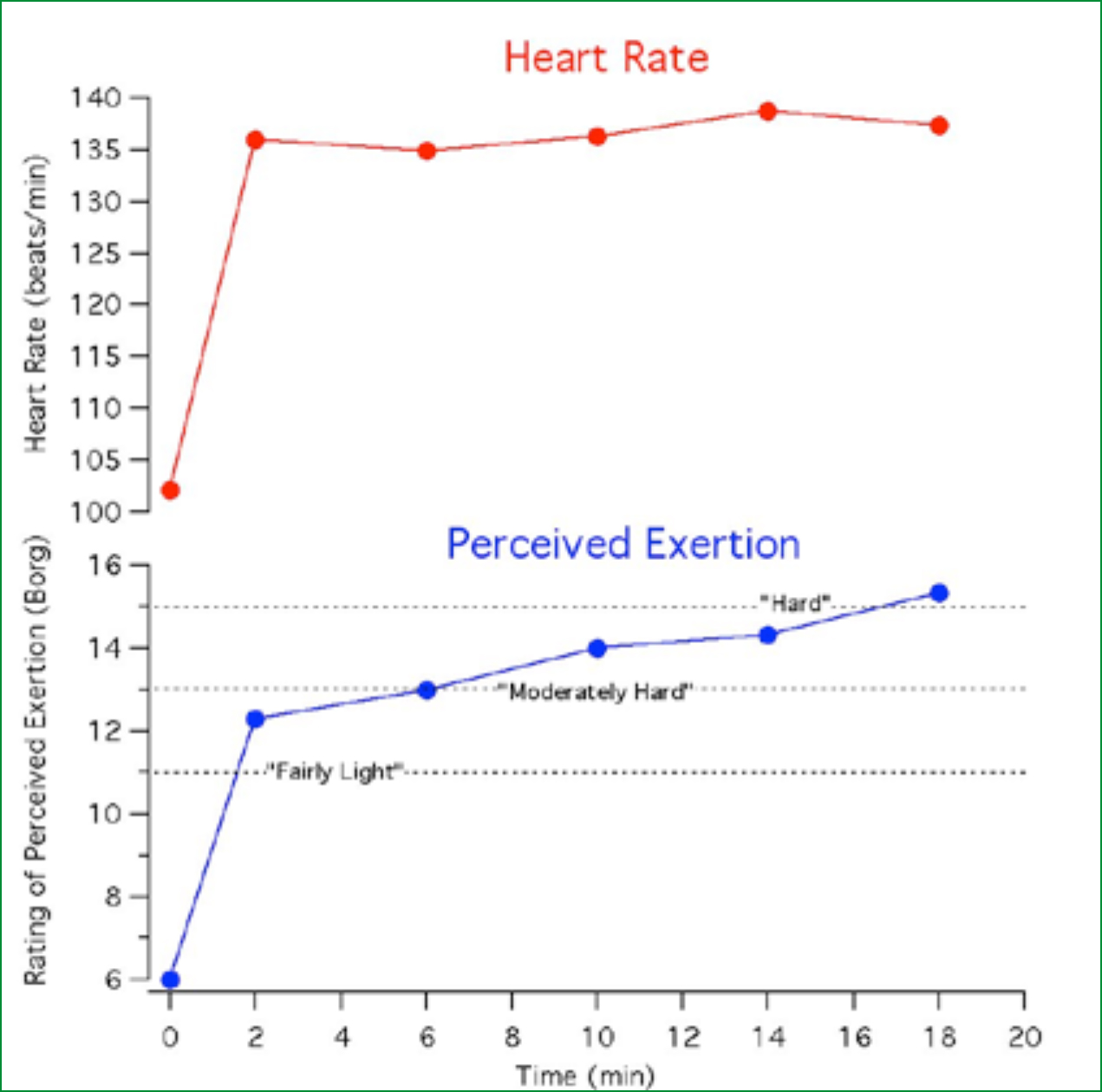
Heart rate of student participants was elevated above rest at the first 2 minute interval, but was not significantly higher until 14 minutes of CPR (138.67 bpm, rest 102 bpm, P=0.045) (Figure 1). Rating of perceived exertion (RPE) increased significantly at the first 2 minute interval while performing chest compressions, and progressively increased at each subsequent intervals at 2 minutes (12.29, P=0.001), at 6 minutes (13, P< 0.0001), at 10 minutes (14, P< 0.0001), at 14 minutes (14.33, P< 0.0001), and at 18 minutes (15.33, P=0.002) (Figure 1). There was no statistically significant difference between the genders and age groups for measures of heart rate and RPE.
Chest compression depth and rate
Across all participants. The mean rate of compressions per 2 minute intervals tended to exceed the recommended 100 compressions per minute (cpm). The mean number of compressions per minute were not statistically significant across participants (n=7) in the first 2 minutes (121.57 cpm) at 6 minutes (121.14 cpm) at 10 minutes (118.51 cpm) at 14 minutes (120.33 cpm), and at 18 minutes (119.67cpm) (Figure 2). However, there was a statistically significant difference between the < 21 years group and 21-25 years group for mean compression rate, 113.4 chest compressions per minute to 136.1 cpm, respectively, P< 0.0001 (Figure 2).
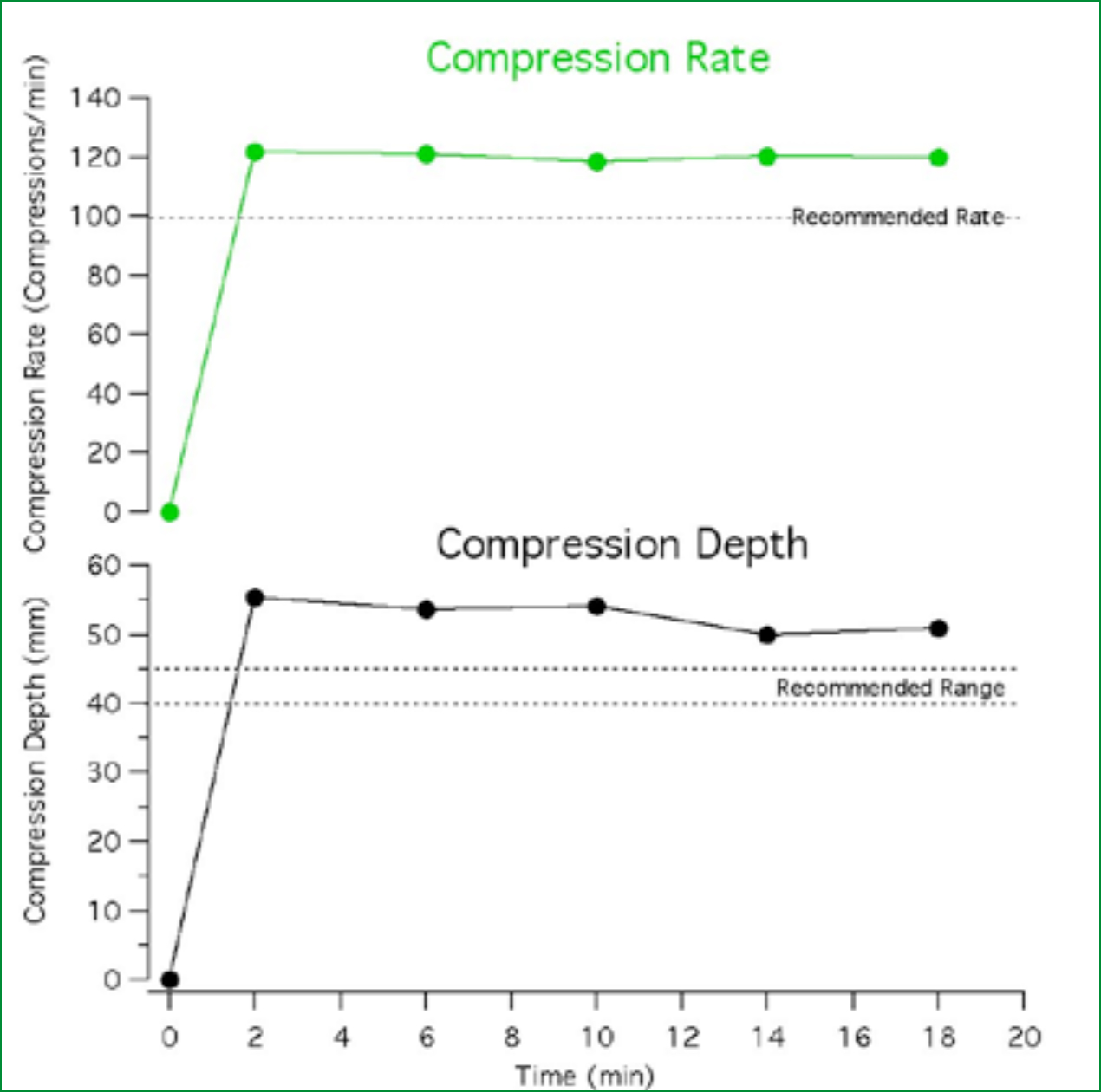
The average compression rates were statistically significant with differences between males and females, 108.0 cpm to 125.6 cpm respectively, P=0.006. Differences in mean compression depth across all participants (n=7) per 2 minute intervals of chest compression were not statistically significant. All participants (n=7) exceeded the recommended compression depth (40-50 mm) at 2 minutes (55.29 mm) at 6 minutes (53.57 mm) at 10 minutes (54.14 mm) and at 18 minutes (50.83 mm) (Figure 2). At 14 minutes, the average compression depth remained within the recommended international guidelines (50.0 mm). For measures of compression depth, there was no statistically significant difference between the genders and age groups.
Discussion
This study has demonstrated that the performance of 20 minutes of 30:2 external chest compressions by paramedic students using the current ILCOR guidelines results in a workload of moderate intensity (as defined by HR), a progressive increase in perceived exertion, and evidence of a decrease in chest compression depth and rate beyond 14 min. These findings importantly add to the paramedic and out-of-hospital body of knowledge regarding CPR and resuscitation more generally.
Heart rate and rating of perceived exertion
External chest compressions performed in this study exceeded both the depth and rate in all participants as reflected in the objective data. However, with the increased number of chest compressions per 2 minutes and increased chest compression depth it would be reasonable to expect that participant's heart rate and rating of perceived exertion would increase over time as reflected in the subjective data. The data for HR indicates that while the workload was of moderate intensity for these participants, but there was no significant rise in HR between 2 minute and 20 minutes of CPR, suggesting cardiovascular/ aerobic systems were coping with the demand. This would suggest that fatigue attributed to cardiovascular/aerobic demands of the exercise was not a major contributor, and points more to muscular fatigue as being a primary factor.
In our study we observed a significant rise in all the participants’ mean heart rate at rest, 102 beats per minute (bpm), prior to commencing the initial 2 minutes (136 bpm) through to 14 minutes (138 bpm) while performing chest compressions. This was similar in another study by Yannopoulos et al (2006) who reported that participant's peak heart rate reached 138 bpm, although their study only performed 5 minutes of continuous chest compressions compared to 10 minutes in this study. They also concluded that 30:2 compression to ventilation ratio resulted in an increased CPR performance and decreased fatigue confirming that uninterrupted chest compressions was well tolerated by rescuers (Yannopoulos et al, 2006).
This was similar in Riera et al's study where participants reported that uninterrupted chest compressions were well tolerated; however their mean value of the participant's heart rate at 2 minutes was 111+ 13 bpm (Riera et al, 2007). In contrast, our study at 2 minutes of uninterrupted chest compressions reported a mean peak heart rate of 136 bpm which may be attributed to the higher compression rates and depth performed by the participants.
These findings may suggest that a certain level of physical fitness may prove to be beneficial for CPR providers to ensure adequate and continuous external chest compressions are performed in cardiac arrest scenarios over a prolong period of time. It has been reported that physical fitness is essential in assisting the rescuer to perform adequate chest compressions during CPR (Lucia et al, 1999).
In a study by Lucia et al (1999), it was reported that subjects with experience in CPR who were physically inactive outside their professional role showed significantly higher heart rate values than those who were not experienced in CPR but were physically active. In our study, the participants reported that they were physically active, 1-6 hours per week of physical activity during personal time; however the majority of them (90%) had not performed CPR before. These findings in our study validate Lucia's et al results. This may indicate the importance of rescuers undertaking some form of aerobic activity in order to improve work capacity for rescuers as well as increase their fitness levels in order to perform adequate and chest compressions during CPR (Baubin et al, 1996; Lucia, et al, 1999).
Compression depth
Previous studies have evaluated the effect of various CPR attempts on perceived fatigue as measured on a visual analogue scale, Likert scale, or Borg RPE (Bridgewater et al, 2000; Yannopoulos, et al, 2006; Chi et al, 2007; Riera et al, 2007; Bridgewater et al, 2008; Trowbridge et al, 2009). This study used the Borg Scale which demonstrated that chest compressions at a ratio of 30:2 for 18 minutes represented a 'somewhat hard ‘exercise from 2-6 minutes to ‘hard’ by 10 minutes. In a similar study by Trowbridge et al (2009), participants reported their perceived exertion using the Borg Scale as 'somewhat hard’ exercise at 5 minutes to ‘hard’ by 10 minutes of external chest compression using the 30:2 ratio (Trowbridge et al, 2009). They also reported increased fatigue levels which contributed to their shift from adequate to inadequate depth of chest compressions (less than 38 mm). These differences may indicate that the physical fitness/capability of the rescuer may be correlated to their ability to perform continuous chest compressions.
In our study there were no significant differences between the participants’ mean compression depths and fatigue levels amongst females and males and across both age groups. Surprisingly, the participants exceeded the recommended compression depth according to the ILCOR guidelines reporting between 50-56 mm regardless of the similar levels of perceived exertion as experienced in the Trowbridge et al (2009) study throughout 20 minutes of CPR.
Considering all data, it is our opinion that this cannot be explained as a sign of exhaustion. One would expect a decline in compression depth rather than an increase in depth to be a sign of exhaustion. An increased compression depth could also reflect a compensation for a decreased compression rate; however this was not the case in this pilot study. Although, we speculate that the resistance to fatigue may reflect the fitness levels in our participants.
Compression rate
Although adequate chest compression depth is important in CPR, equally important is the chest compression rate. In a prospective study by Abella et al (2005), the actual rate of chest compressions demonstrated strong correlation with the initial return of spontaneous circulation with a mean chest compression rate of 90 per minute for initial survivors and 79 per min for non-survivors (Abella, et al, 2005).
According to the European Resuscitation Council (ERC) guidelines, a rescuer should compress the chest at a rate of about 100 min (Handley et al, 2005). In our study, mean chest compression rates exceeded all 2 minute periods within 20 minutes of CPR, which is above the internationally recommended 100 per min. This was similar in studies by Bjorshol et al and Jantti et al who documented mean compression rates between 100 and 140 per min (Bjørshol et al, 2008; Jantti et al, 2009). This has also been documented by other investigators in recent clinical trials (Edelson et al, 2006; Kramer-Johansen et al, 2006; Losert et al, 2006).
However, the findings in our pilot study are in contrast to studies by Ashton et al (2002), Hightower et al (1995), Ochoa et al (1998) and Greingor (2002) which showed some discrepancy with chest compressions deteriorating after the first minute and participants complaining of fatigue after 3-4 minutes. Moreover, rescuers are unable to perceive fatigue when it appears (Gutwirth et al, 2009). In the present pilot study, we assert that the data cannot explain a sign of fatigue. This is based on the expectation that there would be a decrease in chest compression rate rather than an increase in compression rate to be a sign of exhaustion. An increased rate could also reflect a compensation for a decreased compression depth; however this was not the case. However, a possible explanation for the excessive chest compressions in our pilot study may be that undergraduate paramedic participants have not performed CPR before as opposed to hospital-based nursing and medical staff that participated in other studies (Hightower, et al, 1995; Ochoa et al, 1998; Ashton et al, 2002; Greingor, 2002).
According to Lucia et al (1999), training increases work capacity and improves the level of physical fitness, which as a result should have a positive impact on resuscitation quality. This highlights the question surrounding fitness accreditation for rescuer personnel and further research into medical and fitness requirements for new and ongoing health care providers and the change in the compression-ventilation ration to 30:2 (Gutwirth et al, 2009).
Gender
In this pilot study, there was a statistically significant difference in compression rate between genders but not in the compression depth, heart rate and RPE. A study by Ashton et al who was the first to report gender influences on compression performance reported that female subjects achieved significantly fewer satisfactory compressions and poor performance compared to males due to their smaller stature (Ashton et al, 2002).
In contrast, our study reported a statistically significant difference between males and female's compression rates, males having a lower mean 108.0 compared to females with a mean of 125.6 compressions per minute. Furthermore, another study by Ochoa et al reported the effects of fatigue on the efficiency of chest compression are not dependent of gender of the rescuer (Ochoa et al, 1998).
This study did not report any findings on CPR rescuer fatigue associated with gender differences. However, both Ochoa and Ashton studies looked at weight and height as variables that could also influence rescuer fatigue in males and females (Ochoa et al, 1998; Ashton, et al, 2002). Therefore, further investigation into the height and weight of both genders may need to be explored in relation to identifying if a relationship exists between physical attributes and rescuer fatigue.
Limitations
Our study is not without limitations. First, we were unable to gather the rescuers’ physical data to assess whether any chest compression provider factors were linked to external chest compression CPR quality. One might expect such characteristics as physical size to play a role in an individual rescuer's ability to deliver compressions. Another limitation was the small sample size and the lack of blinding which may have affected the study results. It was probably obvious to the participants what the intention of the study was; however, the paramedic students were not blinded to the ratio bringing potential bias to the study results. To note, this study emphasized chest compressions during CPR and subjects were asked to simulate rescue breathing.
It is likely if participants were asked to make sure they were giving adequate rescue breaths, they may take more time in order to provide good ventilations resulting in reduce numbers of total compressions. Furthermore, the Hawthorne effect should be considered as subjects were aware they were being observed. Given this, their chest compression rate and effort may have been greater than if they were performing in a clinical situation.
Chest compressions on a mannequin model do not perfectly resemble clinical CPR and does not take into account physiological differences in patients. Therefore, these limitations in our pilot study results cannot be strictly generalised to clinical practice, however it provides the opportunity to undertake a larger study. Finally, while we have reported significance levels in our results they are likely to be distorted given the small sample size and therefore should be interpreted with caution.
Conclusion
The results from this pilot study suggest that the 30:2 ratio compression-ventilation CPR is well tolerated by undergraduate paramedic students. However, an increase above the internationally recommended guidelines of 100 chest compressions per minute at a depth of 40-45 mm was demonstrated. Although the ILCOR guidelines recommend a change in the provider of chest compressions after 1 or 2 minutes. The trends in our pilot results suggest that changing the rescuer every 2 minutes does not have an effect on rescuer fatigue or chest compression quality using the compression to ventilation ratio 30:2. Further larger scale studies are required to examine this more closely.
