Essex and Herts Air Ambulance Trust (EHAAT) is a publically funded charity that operates two doctor-paramedic pre-hospital care teams to provide support to land ambulance crews in two counties in the South East of England. The service is predominantly helicopter-based but operates a rapid response car outside daylight hours or in poor weather. The total population covered numbers approximately 1.8 million. The team responds to major trauma and medical emergencies, with the latter accounting for approximately 20% of all taskings. The paramedics who work for the service are all employed by the East of England Ambulance Service NHS Trust, and are seconded to EHAAT for a period of 24 months. A comprehensive selection process is undertaken and an extensive training programme covering aviation practice and extended clinical management is in place for successful candidates. In addition, EHAAT paramedics have been among the first to enrol and undergo enhanced skill training in anaesthetics and intensive care medicine as part of a post graduate certificate in advanced paramedic practice in critical care. We believe that one of the strengths of the service provided by EHAAT lies in our paramedics acting as role models and ambassadors for both our service and the ambulance service in general.
The case
We report the case of a 38-year-old male who was working on an industrial site loading 2-tonne paper rolls into the container of a heavy goods vehicle (HGV). When one of the paper rolls slipped off its hoisting mechanism the patient became trapped between two rolls crushing his pelvic area. While waiting for the arrival of the ambulance the patient's colleagues were able to rapidly winch the paper rolls off the patient within approximately 5 minutes of the initial impact.
On arrival of the EHAAT team, a rapid response paramedic was already on-scene and had provided high flow oxygen, cannulated the patient and administered 10 mg intravenous morphine for analgesia. The patient was sitting on a chair six metres in to the back of a HGV container.
On examination the patient was conscious and talking normally with a patent airway and normal respiratory examination. The patient appeared sweaty and pale with significant ongoing pain in his pelvis reported. His heart rate was 100 bpm and his current blood pressure was 103/56 mmHg. Diffuse lower abdominal tenderness was noted in association with a large oblique abrasion over the patient's right anterior superior iliac spine and pain posteriorly over the right sacroiliac joint. Blood was noted at the urethral meatus and the patient held both hips in a flexed position. No other injuries were identified. A working diagnosis of a lateral compression fracture of the patient's pelvis was made with potential for associated haemorrhage and intra-abdominal injury.
Intravenous ketamine was administered to facilitate gently lowering the patient backwards off the chair onto a pre-deployed orthopaedic scoop stretcher with overlying bubble-wrap and a pelvic binder. The patient was packaged with a heating blanket within a thermal bag (Light Emergency Stretcher Systems, Kapp, Norway) to maintain normothermia and carefully removed from the back of the HGV on the hydraulic tail lift. The patient was triaged to the nearest major trauma centre (MTC) by air due to a suspected major pelvic fracture. On loading into the aircraft the patient's blood pressure was noted to drop to 91/45 mmHg so a 1 g bolus of intravenous tranexamic acid was administered and a call made to the MTC to arrange for blood to be available on arrival as part of a major haemorrhage protocol. It was expected that the MTC would have systems in place for immediate investigation, resuscitation, interventional radiology or damage control surgery as indicated (Clamp and Moran, 2011). The team was also aware that the receiving hospital had the ability to provide resuscitative endovascular balloon occlusion of the aorta (REBOA) as part of their resuscitation strategy.
Discussion
Mortality of patients with major pelvic fractures is principally associated with early uncontrollable haemorrhage (Clamp and Moran, 2011). It is therefore intuitive that pre-hospital interventions for such patients are focused upon strategies for minimising blood loss and facilitating timely transfer to a centre capable of providing definitive haemostasis and concurrent resuscitation of other injuries.
Assessment
It is essential that patients with significant pelvic fractures are identified early so that treatment and triage decisions commence swiftly. An appreciation of the mechanism of injury and energy distribution pattern can be key to making this early diagnosis and identifying the likely underlying configuration of fracture. Table 1 highlights the association between mechanism and fracture pattern and Figure 1 demonstrates typical anatomical fracture configurations. Table 2 outlines the common symptoms and signs of pelvic fracture as described elsewhere (Lee and Porter, 2007).
| Mechanism | Fracture |
|---|---|
| Fall from height (landing on one leg) | Vertical shear fracture Unilateral acetabular fracture |
| Fall from height (landing on both feet) | Bilateral acetabular and iliac fractures |
| ‘Front to back’ impact (motorcycle fuel tank strike) | Antero-posterior compression fracture ‘Open book’ |
| ‘Side to side’ impact (T-bone RTC) | Lateral compression fracture |
| Symptoms | Signs |
|---|---|
| Hip pain | ASIS asymmetry/mobility |
| Lower back pain | Sacroiliac joint haematoma |
| Lower abdominal pain | Flexion/rotation of lower limbs |
| Inability to weight-bear | Perineal haematoma |
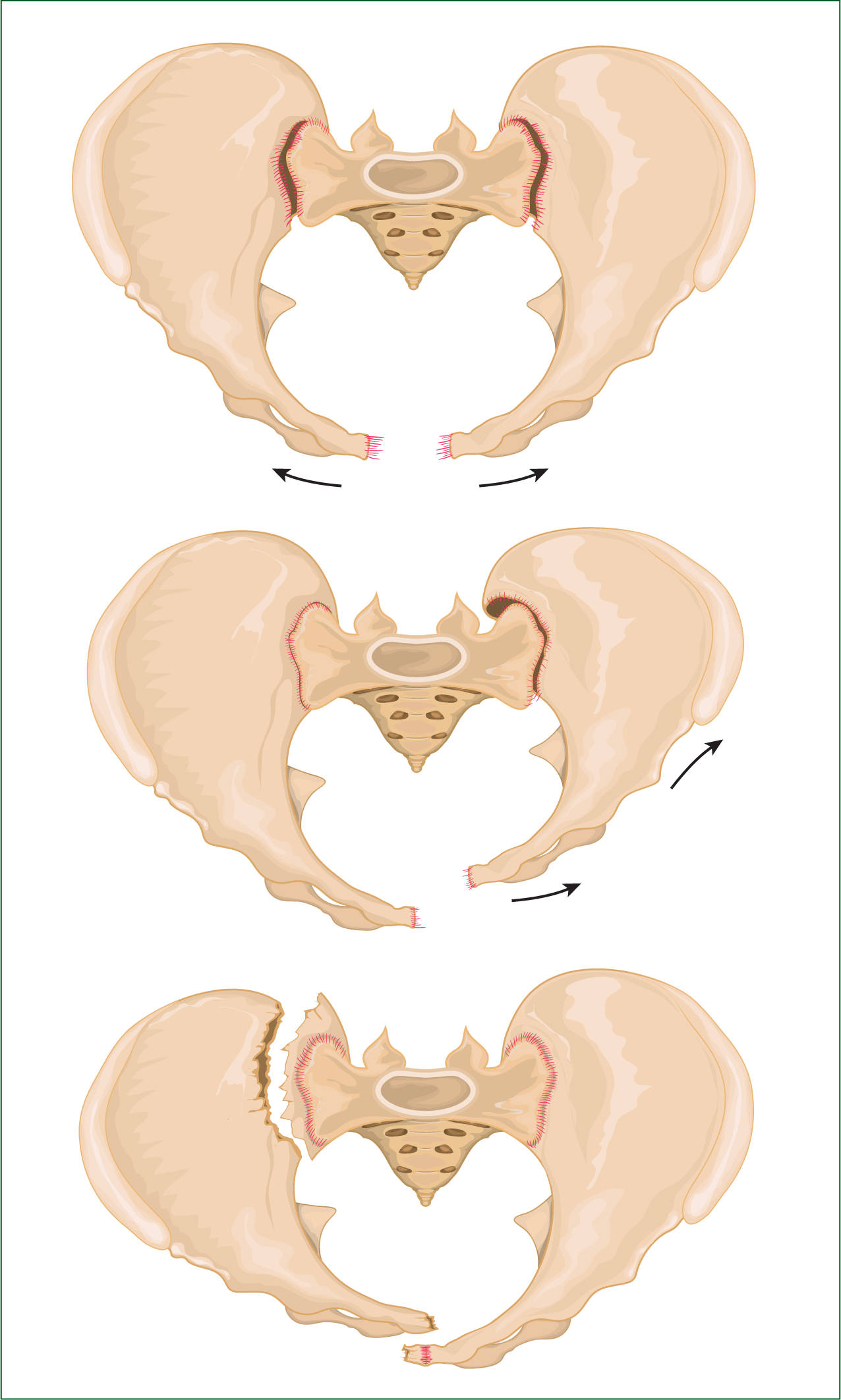
Although not originally intended for the pre-hospital environment, the Tile and Pennal pelvic ring classification can be applied to the mechanism of injury that the pre-hospital clinician is best placed to assess (Pennal et al, 1980). Attention to the mechanism of injury may increase the index of suspicion of a pelvic fracture. Predicting the type of fracture also predicts the anatomical relationship of the bony pelvis and the likelihood of bleeding, and is therefore of great use in deciding the best treatment and triage strategies on scene.
Any pelvic fracture has the possibility of causing major haemorrhage. Anteroposterior compression fractures cause disruption of the venous plexus and tearing of the pelvic floor musculature, which is compounded by bleeding from the fracture ends. Displaced fractures such as those seen in lateral compression injury patterns can damage the internal iliac arteries that run in close proximity to the iliac wings. Interruption of the internal iliac arteries can lead to torrential bleeding within the non-compressible pelvis. However, it is not just vessels that are the source of haemorrhage. Urogenital injuries are common in the lateral compression fracture as disruption of the pubic rami can cause bone ends to penetrate the bladder and transect the urethra. It is possible that a patient may have a combination of fracture patterns. In this case, the patient will bleed from all sites as described above.
Assessment within the pre-hospital environment is based on the clinician's physical assessment of the patient. As such, it is pertinent to note that the historical method of ‘springing’ the pelvis to assess stability and potential for fracture should be deemphasised due to unreliability and potential for iatrogenic injury (Lee and Porter, 2007). Performing this manoeuvre is detrimental to the first clot that has formed and if disrupted, may lead to catastrophic uncontrolled haemorrhage. It is our belief that assessment of the pelvis in this way causes unnecessary pain and risk of demise to the patient and therefore should not be performed.
Management
The key to optimal management of patients with major pelvic injuries is to minimise further bleeding, promote clot formation and stability and facilitate early definitive haemostatic control. If no critical airway or breathing interventions are required, the patient should be examined in the position they are found.
The concepts of careful handling, early splinting of fractures and packaging, should be employed. These interventions should be viewed as critical and therapeutic in themselves.
In blunt trauma patients, minimal movement reduces fractured bone-end disruption with proximity tissue and vascular damage. Once analgesed the patient's clothes should be cut off and a plan verbalised to make the minimal movement required to place the patient ‘skin-to-scoop’. If the patient is found supine, this is generally achieved with 10-degree log rolls (Chesters et al, 2013) to facilitate each half of the scoop stretcher being slid under the patient (as demonstrated in Figure 2 and 3), along with a pre-positioned pelvic binder at the level of the greater trochanters and the addition of any warming devices or blankets.
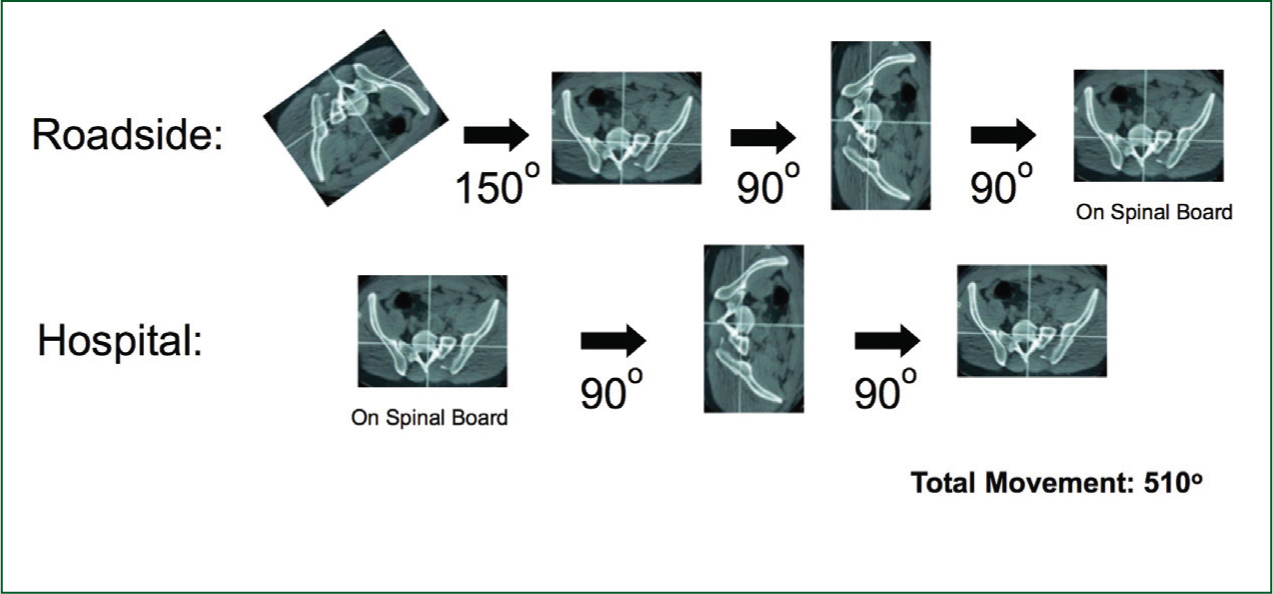
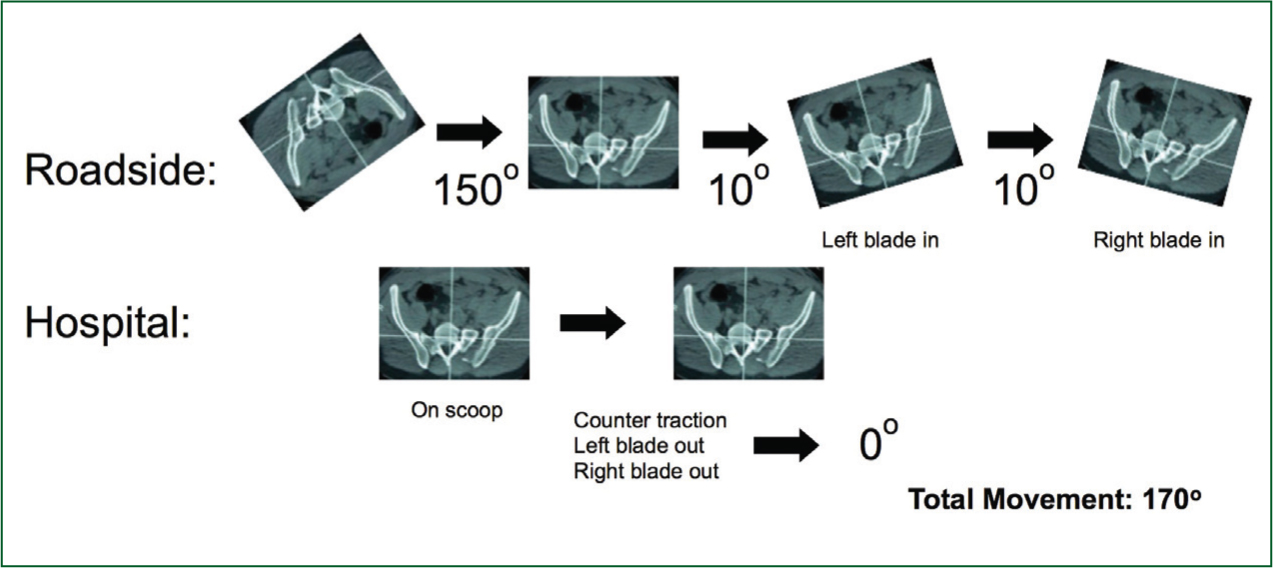
The use of a 10-degree log roll and the orthopaedic scoop stretcher (OSS) compared with traditionally taught methods of patient movement substantially reduces the total amount of rotation through the injured pelvis. Each half of the OSS should be prepared with the scoop blade, thermal bag (or similar heat preserving material), and pelvic binder ready to insert in one motion following the 10-degree log roll. Ideally packaging should be completed with attention to the mitigation of hypothermia, which is associated with poorer outcomes in trauma patients (Martin et al, 2005).
Passive heat control methods include the use of simple blankets, and commercially designed wraps such as the thermal bag, which is used by EHAAT.
This procedure should be performed immediately following primary assessment and application of a pelvic splint should be a priority in the management of this patient group. Applying a pelvic splint will realign the fracture sites and immobilise them in a fixed position, therefore limiting the bleeding from the bone ends, minimising the pain caused by bony movement and tamponading the free blood. However, application of the splint in the incorrect position will reduce the efficacy and potentially cause further injury by inverting the iliac wings if placed too high, and splaying the iliac wings if placed too low. When applied at the level of the greater trochanters the splint encompasses the main body of the pelvis and reduces the diastasis seen at the symphysis pubis. This is particularly important for anteroposterior compression fractures as the space into which potential bleeding can occur is reduced dramatically.
Should a vertical sheer fracture be suspected, the limb of the affected hemi-pelvis can be placed under careful manual traction and the pelvic splint applied in that position. Splinting of lateral compression fractures has caused concern surrounding the potential to inflict further injury by displacement of the lateral compression fracture; however, this force applied is likely to be lower than the original injuring force. When combined with the potential risk of not minimising the bleeding by splinting the fracture, the risks are outweighed by the benefits and therefore splinting of the pelvis should be performed. Application of a pelvic splint should be performed in any blunt trauma patient who is hypotensive.
Resuscitation strategies
Evidence exists that suggests for some patients with injuries associated with haemorrhage it may be advantageous to allow the patient's blood pressure to remain lower than its physiological norm, with the intimation that this may promote clot stability and reduce further bleeding (Clamp and Moran, 2011). For conscious patients with multisystem trauma, the aim should be to maintain a blood pressure that ensures cerebral perfusion—’cerebrating’ (conscious and talking). However, this theory of permissive hypotension may not translate to the very young, elderly and those with marked comorbid disease. This strategy is also likely to be of ‘time-limited’ benefit and may not be an option for remote or rural clinicians with extended pre-hospital times.
Tranexamic acid is an antifibrinolytic which inhibits the conversion of plasminogen to plasmin. It has been shown to improve outcome in bleeding patients with major trauma (Roberts et al, 2013) and its use is becoming more widespread in ambulance service guidelines in the United Kingdom (Association of Ambulance Chief Executives, 2013). As in the case described, the initial 1 g bolus may be administered pre-hospital.
Triage
Local major trauma protocols will determine where patients are triaged to depending on geography and infrastructure. It is crucial that patients with a mechanism and clinical features suggestive of major pelvic fractures are triaged to a major trauma centre (MTC) with orthopaedic and interventional radiology specialists capable of diagnosing and managing such injuries.
The role of enhanced care teams
The provision of pre-hospital critical care teams by land and air for critically ill and injured patients is now well established in the United Kingdom. Patients with major pelvic fractures often have other significant injuries as dictated by the kinetic energy forces involved and may require emergency anaesthesia for traumatic brain injury, surgical intervention for chest injury or enhanced analgesia and sedation for splinting or extrication. A number of enhanced care teams now have provision to administer packed red blood cells out of hospital, which may be advantageous to decompensated patients far down the haemorrhage pathway.
Despite all of the above interventions there is still a group of patients who haemorrhage to death from major pelvic fractures before reaching the hospital. Work continues on novel interventions that may temporarily control bleeding prior to definitive haemostasis. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a possible intervention in such patients (Stannard et al, 2011). This technique involves cannulation of a femoral artery using a needle, allowing a guide-wire and balloon catheter to be thread into the distal abdominal aorta above the bifurcation. When the balloon is inflated blood supply to the pelvis and lower limbs via the common iliac arteries is temporarily arrested allowing a period of haemostasis where the patient can be moved to definitive care. Renewed interest in this technique may lead a place for it in the resuscitation strategy for a small group of patients in the future.
Conclusions
Patients who are bleeding to death from a fractured pelvis depend on a chain of interventions that starts from the moment of impact and ends with the expert rehabilitation provided by a hospital team. Attention to detail in the pre-hospital phase is a crucial link in the chain without which the situation may be unsalvageable by the end time they reach the receiving unit. The management of pelvic fractures within the pre-hospital environment aims to minimise bleeding, promote clot formation and preservation, and stabilise the pelvis. We have outlined some of the anatomical and pathophysiological considerations that are required to understand the treatment of these complex patients. We have emphasised that simple measures, instigated early, can be the difference between a successful outcome and a patient who exsanguinates before reaching the hospital.
