In June 2008 the British Thoracic Society (BTS) produced the frst national emergency oxygen guideline (O’Driscoll et al, 2008). This was endorsed by 21 professional bodies and associations, including the British Paramedic Association, the Joint Royal Colleges’ Ambulance Liaison Committee and the Resuscitation Council (UK).
The emergency use of oxygen is an area where there is a lack of clinical trial evidence, with controversy surrounding both risks and benefts, as well as some strongly held beliefs and it is in this context that this guideline was produced. National audit has suggested that guideline uptake has been encouraging in the inpatient setting, but also highlights the diffculties inherent in changing established practice (O’Driscoll et al, 2011). Our own data suggest that uptake in the Emergency Department (ED) has been less impressive (Wallace et al, 2010) despite widespread guideline awareness among ED physicians (unpublished observation of ED trainees at regional training sessions). While the guideline predominantly covers the use of oxygen in the inpatient setting a section specifcally devoted to pre-hospital care is included and many of the points covered are also applicable to the pre-hospital environment.
Since the publication of the guideline Austin and colleagues (Austin et al, 2010) have demonstrated that, even in the clinical trial setting, adherence to the guideline by paramedics was poor, yet even allowing for this there was signifcantly lower mortality and improved physiological parameters in the guideline arm of their study. This suggests even attempting to follow the guideline will save lives. Encouragingly, an audit of the North West Ambulance Service in the UK showed both good compliance (86 % broad compliance, 73 % full compliance) with the guideline, and an improvement in compliance after an educational intervention (Matthews et al, 2010).
It is in this context that this article has been written, aiming to bring further attention to this comprehensive guideline on the use of oxygen in all emergency situations.
Background
Historically, the belief has generally been that where oxygen is concerned ‘more is better’. The guideline highlights situations where this is not the case, and indeed may even be dangerous, while also acknowledging certain specifc circumstances where it may be true. The main thrust of the guideline is to introduce the concept that oxygen should be prescribed to a target saturation and not by fow rate or concentration, with the aim being to obtain a near normal oxygen level for that patient.
Oxygen has traditionally been administered for three main indications, for correction of hypoxaemia, for ill patients who are not hypoxaemic (either on the assumption they may become so or due to the belief that more is better, especially when ill) and fnally to treat breathlessness. An evidence base only exists for the frst of these, indeed, in the second, the use of oxygen may even be harmful as it may mask a deterioration in clinical condition.
The guideline discusses what levels of oxygenation are normal and what may be harmful to defne upper and lower limits of the target ranges as well as discussing blood gas physiology.
Guideline summary
Target saturations
The guideline refers extensively to the use of oxygen aimed towards target oxygen saturations. In the inpatient setting the guideline recommends that oxygen is prescribed to a target saturation, in the emergency setting a prescription is not required, but the same principles apply and oxygen should be administered with the aim of achieving an appropriate target saturation and both the oxygen provided and the patient’s saturations should be clearly documented once the patient has been stabilised. For these target levels to be set a consensus was reached as to what is normal and what is safe. The normal daytime oxygen saturation in adults is 96–98 %, falling to 95 % in the elderly.
Severe hypoxia may lead to cardiac arrhythmias, renal damage, brain damage and death. In order to set a lower limit for target saturations data was reviewed from altitude and nocturnal oxygenation studies. Acute hypoxaemia is only likely to be dangerous at levels of <6 kPa (approximately equivalent to an oxygen saturation of 80 %), however, the lower limit of normal was defned as 94 % as composite of what is near normal and what is safe.
Sudden onset hypoxaemia is more dangerous than hypoxaemia of gradual onset, oxygen levels may be signifcantly lower in certain chronic medical conditions, even when stable, and in view of the fact that excess oxygen in these groups may potentiate type 2 respiratory failure a lower target range was required. Data suggest that oxygen saturations of 85 % in acute chronic obstructive pulmonary disease (COPD) will be adequate to prevent death, although to allow a margin for error a minimum oxygen saturation of 88 % was set for patients at risk of type 2 respiratory failure. The safety of this approach has since been validated (Austin et al, 2010).
For those at risk of type 2 respiratory failure the upper limit of the target range was based on the work of Plant’s group who demonstrated that the greatest risk of type 2 respiratory failure in those with COPD was in those with a PO2 of >10 kPa, which equates to oxygen saturations of 92 % (Plant et al, 2000), and thus 92 % was set as the upper limit of the target range for those at risk of type 2 respiratory failure.
Why have upper limit to the target range in those not at risk of type 2 respiratory failure?
While the negative effects of excess oxygen in those at risk of type 2 respiratory failure are well described, it has historically been considered that, other than in this group, there is no risk in giving oxygen, indeed, there is a widely held belief that with regards to those not at risk of type 2 respiratory failure, more is better. There is no data to support this practice and there are multiple clinical and theoretical risks of hyperoxia even in those not at risk of type 2 respiratory failure (see Box 2). In view of this, an upper limit was set to the target saturations range equating to the upper limit of normal in healthy subjects of 98 %.
Immediate assessment
Assessment should be performed as per standard practice, including oxygen saturations, with management as per standard ‘ABC’ protocol, followed by obtaining a quick history from the patient and/or family or friends. The respiratory rate is the single best indicator of severe illness, although is not a specifc indicator of oxygegnation, and the same is true for heart rate and blood pressure. Clinical assessment of hypoxia, by attempting to assess for cyanosis, is also ineffective, and therefore it is recommended that wherever oxygen is used, pulse oximetry should also be made available. This also confers a cost saving beneft by reducing unnecessary oxygen usage and it is recommended that oxygen saturations be measured in all breathless and acutely ill patients.
While pulse oximetry is generally accurate to within 1–2 % of directly measured arterial oxygen saturation, it can underread in circumstances of poor peripheral perfusion (though ear lobe monitoring may be performed instead), sickle cell crisis or with false nails or nail varnish (which should always be removed). It is also unreliable in carbon monoxide poisoning and methaemoglobinaemia, where it will give a falsely high reading.
The main aim of pre-hospital assessment is to avoid harmful levels of hypoxaemia in all patients while avoiding harmful levels of hypercapnia in those at risk. After initial assessment, patients can be divided into the following groups:
Oxygen should given to hypoxaemic patients, but is not required if oxygen saturations are >94 %.
Cardiopulmonary resuscitation and critical illness
Table 1 from the guideline summarizes recommended oxygen usage in critically ill patients.
[COPD, chronic obstructive pulmonary disorder disease, PaO2, arterial oxygen tension.]
In cardiopulmonary resuscitation the use of 100 % oxygen is recommended. This is not evidence based, though randomized controlled trials are unlikely to be undertaken and the use of high concentration oxygen to maximise oxygen delivery to the tissues in circulatory collapse would seem intuitive.
Initial high concentration oxygen given via a reservoir mask at a fow rate of 15l/min is recommended in cases of shock, major trauma, sepsis or other critical illness, such as near drowning, anaphylaxis, major pulmonary haemorrhage or major head injury. Initial high concentration oxygen is also recommended for those with initial saturations <85 % not at risk of type 2 respiratory failure.
The guideline recommends that, once estabilised, the aim will then be for target saturations appropriate to any underlying medical condition as below. Since the publication of the guideline, this approach has been further validated, in a retrospective review of data from a large American Intensive Care Unit (ICU) database, those patients post cardiac arrest who were hyperoxic on arrival to the ICU had signifcantly higher in hospital mortality than those that were either normoxic or hypoxic (Kilgannon et al, 2010). This recommendation has also been taken up by the Resuscitation Council (UK) in their most recent Advanced Life Support (ALS) guidelines, who recommend that ‘once return of spontaneous circulation (ROSC) has been established and the oxygen saturation of arterial blood (SaO2) can be monitored reliably (by pulse oximetry and/or arterial blood gas analysis), inspired oxygen is titrated to achieve an SaO2 of 94–98 % (Resuscitation Council (UK), 2010).
Conditions requiring moderate oxygen supplementation:
In almost all patients, the recommended target oxygen saturations will be 94–98 % including:
Treatment can be undertaken with nasal cannula or a standard facemask. If these patients are not hypoxic (oxygen saturations on air are >94%) no supplementary oxygen needs to be given even if the patient is symptomatically breathless or tachypnoeic.
Table 2 from the guideline (reproduced below) summarises recommended oxygen usage in those with serious illnesses requiring moderate levels of supplemental oxygen.
Recommended oxygen therapy in patients who may at risk of type 2 respiratory failure
Conditions which can predispose to type 2 respiratory failure:
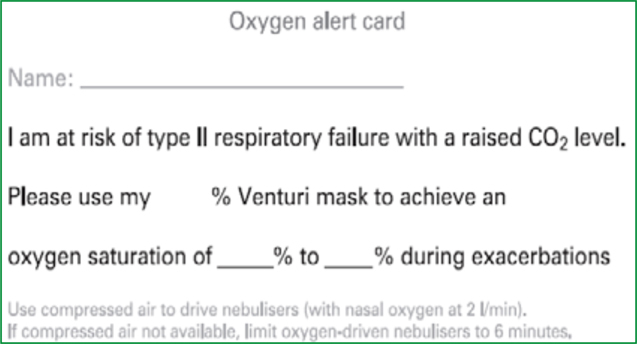
The guideline recommends that those patients with previous hypercapnic respiratory failure be given an alert card (Figure 1) and/or have an entry made in their electronic record, both at the hospital and in the ambulance control system to alert the emergency team of their optimal oxygen dose from previous admissions. The guideline recommends that in the absence of this information, a target saturation range of 88–92 % should be assumed for all patients at risk of type 2 respiratory failure. These patients should also be supplied with a 24 or 28 % venturi mask that they can present to ambulance staff along with their oxygen alert card, this may prove particularly benefcial, as one audit showed that these were not universally available in the ambulance service (Matthews et al, 2010).
These diagnoses are not always clear, some patients are not aware of their diagnosis or have been mislabelled as, or use the term, asthmatic, though other terms may also be used such as chronic bronchitis or emphysema. If the diagnosis is unknown, those over the age of 50 who are long-term smokers or ex-smokers and breathless on minor exertion should be presumed to have COPD.
The guideline recommends starting treatment with a 28 % venturi mask (at a fow rate of 4 l/min) in those at risk of type 2 respiratory failure and up or down titrating to keep the patient’s saturations within the target range, although often on an ambulance journey no change will be required.
Due to the venturi principle, increasing the oxygen fow rate will not increase the inspired percentage of oxygen, only the fow rate of both air and oxygen while keeping the two in the same proportion, and this is likely to be necessary in patients with a respiratory rate greater than 30 breaths per minute.
If a patient at risk (or presumed to be at risk) of type 2 respiratory failure is accidentally treated with excess oxygen, the oxygen therapy should not be discontinued, though should be reduced to 28 % via a venturi mask and then titrated accordingly to target saturations.
The management of other conditions where type 2 respiratory failure is a potential risk are essentially the same as for COPD.
The use of oxygen in those at risk of type 2 respiratory failure is summarised in Table 3 from the guideline reproduced above.
CF=cystic fibrosis; COPD=chronic obstructive pulmonary disease; CPAP=continuous positive airway pressure; IPPV=intermittent positive pressure ventilation; NIV=non-invasive ventilation; PaCO2-arterial carbon dioxide tension; SpO2=arterial oxygen saturation measured by pulse oximetry
Recommended oxygen therapy in special situations
There are a few situations which fall outside the standard guidance, where either high concentration or controlled oxygen is required for reasons other than those listed above.
Conditions requiring high concentration oxygen:
Conditions requiring controlled oxygen:
Oxygen may potentiate lung damage in these conditions, even if given many years later in the case of bleomycin lung injury, and is therefore only recommended if oxygen saturations drop below 90 %.
Nebulisers
A fow rate of >6 l/min is required to drive a standard nebuliser. For patients not at risk of type 2 respiratory failure, either oxygen or compressed air can be used to drive the nebuliser. If compressed air is used, supplementary oxygen, if required, can be given via nasal cannulae. For those at risk of type 2 respiratory failure nebulisers should ideally bedriven by compressed air, again with the provision ofcontrolled supplementary oxygen if required. Wherethis is not possible, oxygen may be used to drivethe nebuliser, but this should be kept to under sixminutes in duration, as six minutes will allow most ofthe drug to be delivered while minimising the risk ofpotentiating type 2 respiratory failure.
Specifc recommendations for the emergency use of oxygen in ambulances
Section 9 and Appendix 4 of the guideline specifcally cover the emergency use of oxygen in ambulances, as well as in the community and other pre-hospital settings.
The guideline recommends that it is essential to provide optimal oxygen therapy at the earliest possible opportunity, target saturations should be used, and therefore pulse oximetry is required to achieve this. As a result, it is recommended that pulse oximetry is necessarily available in all locations where oxygen is being used. It is also recommended that all emergency ambulances and emergency or fast-response type vehicles, as well as ambulance service motorbikes or cycles, should be equipped with oxygen and oximeters appropriate for their means of transport.
Assessment should be carried out as outlined above. Having assessed that the airway is clear, it is recommended that oxygen be used if oxygen saturation is below the target level. Oxygen saturations should then be measured continuously until the patient is stable or arrives at hospital, with the oxygen concentration being adjusted accordingly to maintain saturations within the target range. Oxygenation is reduced in the supine position, and therefore fully conscious hypoxaemic patients should be maintained in the most upright posture possible.
Recommendations are also made on documentation and handover, including the suggestion that all documents that record oximetry measurements should state whether the patient is breathing air or supplementary oxygen, and if so, at what fow rate. The guideline recognises that in most emergency situations oxygen is given to patients immediately without formal prescription and state that the need for a formal prescription should never preclude oxygen being given, but that a subsequent written record should be made as soon as is practical, including documenting oxygen saturations prior to commencing oxygen therapy. On arrival at hospital, all critically ill patients and those at risk of type 2 respiratory failure should be triaged as very urgent, and receive blood gas measurement immediately on arrival.
It is recommended that the following delivery devices should be available in pre-hospital settings where oxygen is administered:
Recommendations regarding implementation of the guideline
Conclusion
This guideline provides the frst comprehensive guidance on the use of oxygen in the emergency setting. Uptake is improving, and it is hoped that this article will continue to improve uptake and adherence to the appropriate guidelines. The key messages to take from the guide are that oxygen should be administered to a target saturation best suited to the patient’s underlying medical condition, and that despite the commonly held belief, more is frequently not better where the administration of oxygen is concerned.
