Emergency Medical Services (EMS) are often frequented to treat outpatient palliative care patients at the end-of-life (EoL). Therefore, paramedics must have knowledge in legal aspects, communication with palliative care patients and their care, and the special aspect of withholding or withdrawing outpatient resuscitation in terminally ill patients (Stone, 2009).
Overall, palliative care patients and patients at the EoL define a major mission for EMS and paramedics (Mengual, 2007). About 3–5% of all pre-hospital emergencies deal with palliative care (Wiese, 2007; 2010). Especially cardio-pulmonary-resuscitation in unresponsiveness palliative care patients offers only a short term success and often limits patients’ self-defined quality of life (Eló, 2005). Mostly, resuscitation is performed reflexly but there is a need to prevent cardio-pulmonary resuscitation in the terminally ill patient (Iserson, 1991).
Pre-hospital emergency medical care itself is defined as a medical care to avoid the death of the patient, to stabilise his vital parameters (e.g. airway, breathing, and circulation), and to transfer the patients into an emergency department to offer them a treatment according to their medicallsymptoms (Iserson, 1991). However, in Germany, there is no regular integration of palliative care and therapeutic decisions at the EoL into emergency medical curricula (Wiese, 2010).
EoL facts should be integrated into pre-hospital emergency medical training curricula, e.g. to avoid unnecessary resuscitation in terminally ill patients (Stone, 2009). In the UK, for example, EoL education is part of the emergency medical curricula. However, this education is limited and often lacking in both content and context.
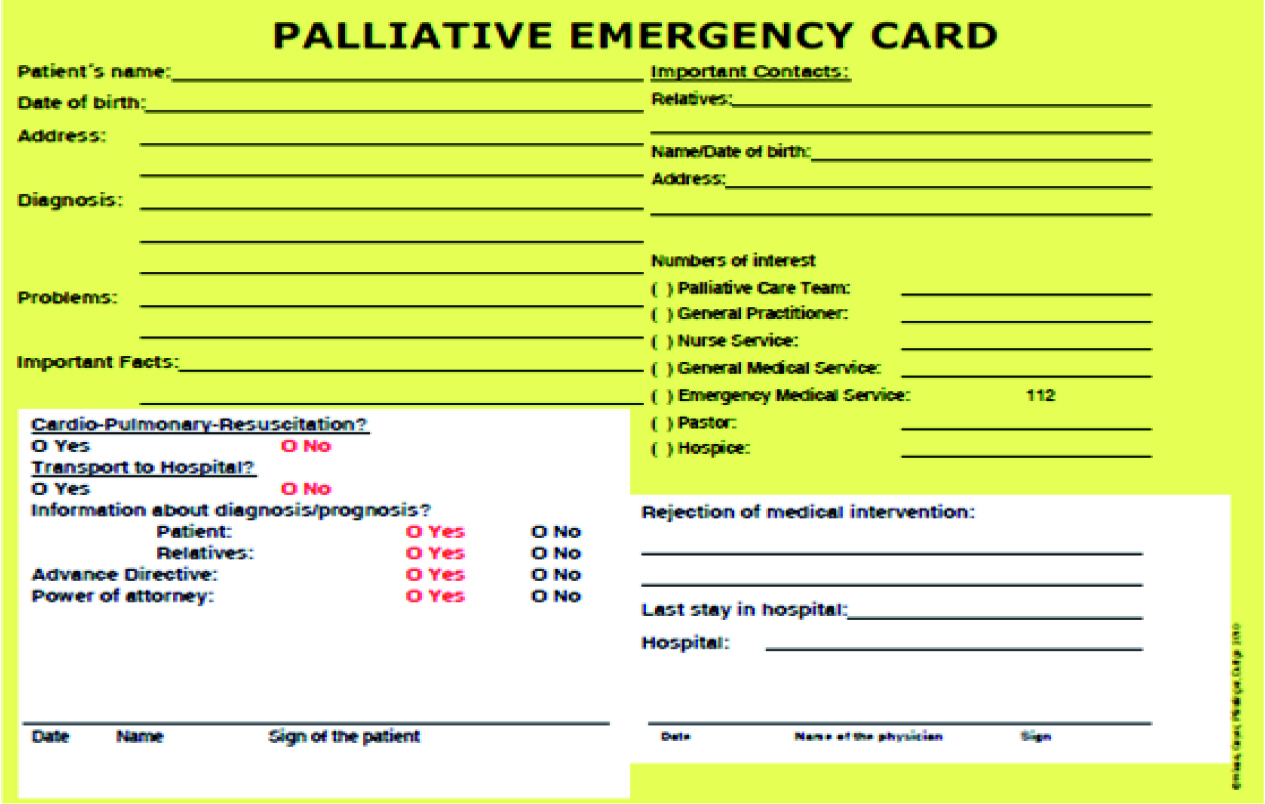
Paramedics in Germany may not be able to withdraw from resuscitation without a directive a pre-hospital emergency physician. Therefore, in the present investigation, paramedics were asked about; (1) the influence of advance directives concerning their pre-hospital treatment of palliative care patients in the case of emergency, (2) legal problems concerning EoL-decisions which were made by paramedics, and (3) the use of ‘Do not attempt resuscitation’ orders (DNAR orders) and/or palliative emergency cards (Figure 1) in according to patients wishes versus the treatment by paramedics. A pallative emergency card (PEC) is used by palliative care patients to not attempt resuscitation if the patient is found pulseless (Taghavi, 2011). Such a pre-hospital emergency sheet is similar to DNAR orders as used in the US and in the UK. A PEC may strengthen the autonomy of palliative
EoL education should be part of emergency medical curricula all over Europe
This study was undertaken to determine paramedics’ understanding of their role in withholding or withdrawing resuscitation/EoL-treatment of palliative care patients when an advance directive is present.
Methods
We contacted 900 paramedics personally (face-to-face contact) during April to September 2008 from Emergency Medical Services at Goettingen and Hamburg in Germany. A written survey was given to all included paramedics. This survey was designed for self-response, using closed questions and free answers.
The following demographic information was asked (brackets indicate possible answers to the question):
As independent variables, we defined (1) ‘occupational/working experience’ (less/more than 10 years, (2) ‘emergency responses’ (less/ more than 100/month), (3) ‘experiences in palliative emergencies’ (less/more than 10 palliative emergencies/year), (4) ‘palliative emergency sheets concerning end-of-life decisions’, and (5) paramedics’ treatment options during resuscitation.
We defined the following dependent variables (brackets indicate possible answers to the question):
Participants
All paramedics of the investigated emergency departments of both cities were integrated into our study. During our investigation, all of them worked actively as a paramedic. The return of the questionnaire was defined as the permission to taking part in the present investigation.
Primary data analysis and ethics
All analyses were done in Microsoft Excel 2003 and SPSS version 16.0. Free answers were analysed by using a five term categorisation. Data from both investigated cities were analysed using a common database. We used the t-test and the Chi-Square test to compare descriptive proportions. We used the analysis of variance test (ANOVA) and the ‘Posthoc-BONFERRONI’ test for group analysis in accordance with the defined group parameters. A P-value of 0.05 was considered to be statistically significant. Data was collected anonymously and anonymity was guaranteed to all participants. Formal approval for our study was obtained from two institutional review boards (University of Goettingen and University of Regensburg); national ethical permission was not required).
Results
Demographics
Responses were returned from 728 respondents over all (total response rate
81%). From Hamburg 620/750 (83%) and from Goettingen 108/150 (72%) responded the questionnaire (Taghavi, 2011).
There were no significant differences between the paramedics of both included towns. Therefore, the following results are presented for all included participants. Overall, 98.5% were male and above 20 years of age. More than 70% of all investigated paramedics dealt with palliative care patients and emergency treatment in patients at the EoL (71%).
Independent variables
The independent variables (taken in accordance with Taghavi, 2011) were (1) ‘occupational experience’ (less/more than 10 years, (2) ‘emergency responses’ (less/more than 100/ month), (3) ‘experiences in palliative emergencies’ (less/more than ten palliative emergencies/year), (4) ‘palliative emergency sheets concerning end-of-life decisions’, and (5) paramedics’ treatment options during resuscitation.
Consideration of the dependent variables depending on the independent ones
‘Advance directives are not legally binding in relation to the emergency medical treatment by paramedics’
A total of n=224 respondents (31% of all participants) answered that advance directives are not legally binding for paramedics in Germany. There were statistically significant (P<0.05) more paramedics with (1) an occupational experience of more than 10 years, (2) with experience in emergency responses in patients in who advance directives led to therapeutic limitations, and (3) with less than 10 resuscitations/years answered that advance directives are not legally binding for paramedics. The following differences were found in the intergroup comparison:
‘Medical treatment referred to in the patient’s wishes may cause legal problems for paramedics’
Overall, 108 participants (15%) declared that medical treatment referred to in the patients’ wishes may cause juridical problems for paramedics. Statistically significant (P<0.05) more paramedics with (1) an occupational experience of less than 10 years, (2) with an emergency response experience of less than 100/month, (3) with less than 10 palliative emergencies per year, (4) with experiences in emergency responses in patients in who advance directives led to therapeutic limitations, and (5) with less than 10 resuscitations/years answered that medical treatment which is referred to the patient’s wishes at the end of life may cause legally problems for paramedics.
The following differences were found in the intergroup comparison:
‘Medical treatment not referred to thepatient’s wishes may include legal problems forparamedics’
Overall, 353 respondents (48%) declared that medical treatment which is not referred to in the patients’ wishes may cause juridical problems for paramedics.
Statistically significant (P<0.05) more paramedics with (1) an occupational experience
Paramedics should have greater legal competence concerning EoL decisions, especially in accordance to resuscitation
‘A palliative emergency card is suitable formedical decisions at the EoL’
Overall, 407 respondents (56%) declared that a palliative emergency card seems to be helpful for medical decisions in patients at the EoL. Statistically significant differences (P<0.05) were seen in respondents with (1) more than 10 years working experience, (2) with less than 100 emergency cases per month, and (3) with more than 10 so called palliative emergencies per year. Those who had more than 10 years working experience, less than 100 emergency cases per month, and (4) more than 10 palliative emergency cases per year declared a palliative emergency card as helpful for their medical decision in patients at the EoL. The following differences were found in the intergroup comparison:
‘A palliative emergency card is not suitablefor medical decisions at the EoL’
A total of 321 paramedics (44%) declared that a palliative emergency sheet seems not to be suitable for medical decisions at the EoL, 220 of those named legal uncertainties as a cause for their decision. Statistically significant (P<0.05) more paramedics (1) with an emergency response experience of less than 100/month, (2) with more than 10 palliative emergencies per year, and (3) with experiences in emergency responses in patients in who advance directives led to therapeutic limitations answered that a palliative emergency card is not suitable for paramedics’ medical decisions at the EoL The following differences were found in the intergroup comparison:
‘Paramedics wished more competencesregarding decisions at the EoL’
Overall, 333 of all investigated paramedics (46%)wish more competences regarding EoL decisions. Statistically significant (P<0.05) more paramedics with (1) more than 10 palliative emergencies per year, and (2) with experience in emergency responses in patients in who advance directives led to therapeutic limitations answered that it would be helpful for paramedics to get more competences regarding decisions in patients at the EoL. The following differences were found in the intergroup comparison:
’Continuous resuscitation by paramedics until the pre-hospital emergency physician decides about the ongoing therapeutically options is legally necessary’
A total of 640 paramedics (88%) may resuscitate the patient reflexly until a pre-hospital physician arrives and decides about the ongoing therapeutic options. Statistically significant (P<0.05) more paramedics with (1) an emergency response experience of less than 100/month, (2) with less than 10 palliative emergencies per year, and (3) with experience in emergency responses in patients in who advance directives led to therapeutic limitations answered that continuous resuscitation by paramedics until the pre-hospital emergency physician decides about the ongoing therapeutically options is legally necessary. The following differences were found in the intergroup comparison:
Discussion
In our investigation, paramedics reported that they often treat palliative care patients and patients at the EoL. Resuscitation is very often started by paramedics in the absence of a pre-hospital emergency physician (EP). The study shows that there is no clarity regarding the EoL treatment given to palliative care patients by paramedics. For this there is a need of EoL training for paramedics as previous investigations have also described (Partridge, 1998; Stone 2009). Into this emergency training curricula, it must be included how to verify an advance directive, juridical problems concerning when to withhold resuscitation, and how to talk to caregiving relatives (Stone, 2009). Also in this regard, similar problems have been described internationally in Canadian and American (US) paramedics (Guru, 1999; Mengual, 2007; Stone, 2009). The integration of palliative medical competences into the emergency medical system may reduce burdensome and questioned therapeutic medical measures of palliative care patients and patient at the EoL (Gisondi, 2010).
In our investigation, about 46% of all paramedics felt that they required a greater level of competence concerning decisions to withhold or withdraw resuscitation in terminally ill patients who have written an advance directive or a palliative emergency card. This fact implies either that they have misplaced confidence in managing such obviously complicated palliative emergencies, or that they actually do have sufficient skills and knowledge, and it is perhaps the legal parameters within which they operate that are actually the problem. Either way, some insight into just how much self-directed or in service training has been provided may help to illicit further evidence to dissect why less than
However, worldwide there is a legal problem concerning the validity of advance directives and palliative emergency cards and the medical therapy given to the patient by paramedics
In the US there are in most states (38/50) legal conditions which underline the patients’ will and its validity when an advance directive exists (Ebell, 1991; Seckler, 1991; Marco, 2005). However, worldwide there is a legal problem concerning the validity of advance directives and palliative emergency cards and the medical therapy given to the patient by paramedics. About 30% of all respondents declared that advance directives are not legally binding for paramedics. This result corresponds with the juridical situation in some countries (for example France, Austria, Switzerland and parts of the US). In the future, there is a need to clarify the legal issues concerning paramedics. An achieved consensus on the role of paramedics in EoL management like in the emergency department seems to be necessary and helpful (Quest, 2011). This need is especially justified by the fact that patients expect respect for their will and their wishes in an emergency situation (Theorovska, 2005; Taghavi, 2011). In the present investigation, about 50% of all paramedics wished for a higher level of competency regarding decisions at the EoL. In the paramedic based pre-hospital emergency medicine area, advance directives and/ or palliative emergency cards seems not to ensure the patients autonomy at the EoL (Brink, 2008; Taghavi, 2011).
Limitations
The present investigation has important limitations. A primary limit of the study lies in its questionnaire based design. Firstly, there was no comparison of respondents to no-respondents. The design of the questionnaire may not represent general opinions and knowledge of the respondents.
The questionnaire was self-administered, therefore, the validity of this instrument was not tested. Moreover, theoretical answers and opinions could not be transferred into practical therapeutic measures objectively and furthermore, the fact that we did not enquire about the competency and prior training in EoL for paramedics completing this survey must be considered as another limitation. It is also worth mentioning that other facts of this investigation, especially concerning the complicated questions about advance directives and palliative emergency cards are published by the working group in Palliative Medicine in 2011 (Taghavi, 2011). In addition, the present article is focused on other parts of the whole investigation and no reiteration of the previously published study.
Conclusions
In conclusion, paramedics play a multifaceted role in the outpatient palliative care. Our results underline the necessity for more training in EoL. Paramedics stated that improved guidelines regarding EoL decisions/advance directives and the possibility to withdrawing resuscitation for appropriative outpatient emergencies in palliative care patients are necessary. The treatment of terminally ill patients by paramedics may present an ethical problem: if paramedics honour patients’ wishes, they will violate juridical regulations. In future, a change concerning current regulations in the outpatient setting seems to be necessary as well.
