This article reviews the small amount of available literature regarding pre-hospital self-extrication, and the mechanics of the spine and spinal cord, in an attempt to show that alert and conscious patients are capable of managing their own cervical spine (c-spine) during self-extrication, in line with the recommendations made by the Faculty of Pre-hospital Care (Connor et al, 2013). This will generally involve less movement than assisted extrication, as well as decrease the time to definitive care (by avoiding a prolonged mechanical extrication), utilise fewer resources and avoid the destruction of an often serviceable vehicle. The situation is analogous to a patient with a lower limb injury who will still be able to mobilise, but do so in a way to protect their own injury, without worsening it or causing pain. It must be continuously emphasised that this is not an attempt to ‘clear’ the c-spine, simply a means of extrication that allows the patient to manage their own injury (or potential injury) to reduce unnecessary movement, prior to immobilisation. This is something advocated by the author's HEMS team, and many other advanced trauma teams in the pre-hospital environment.
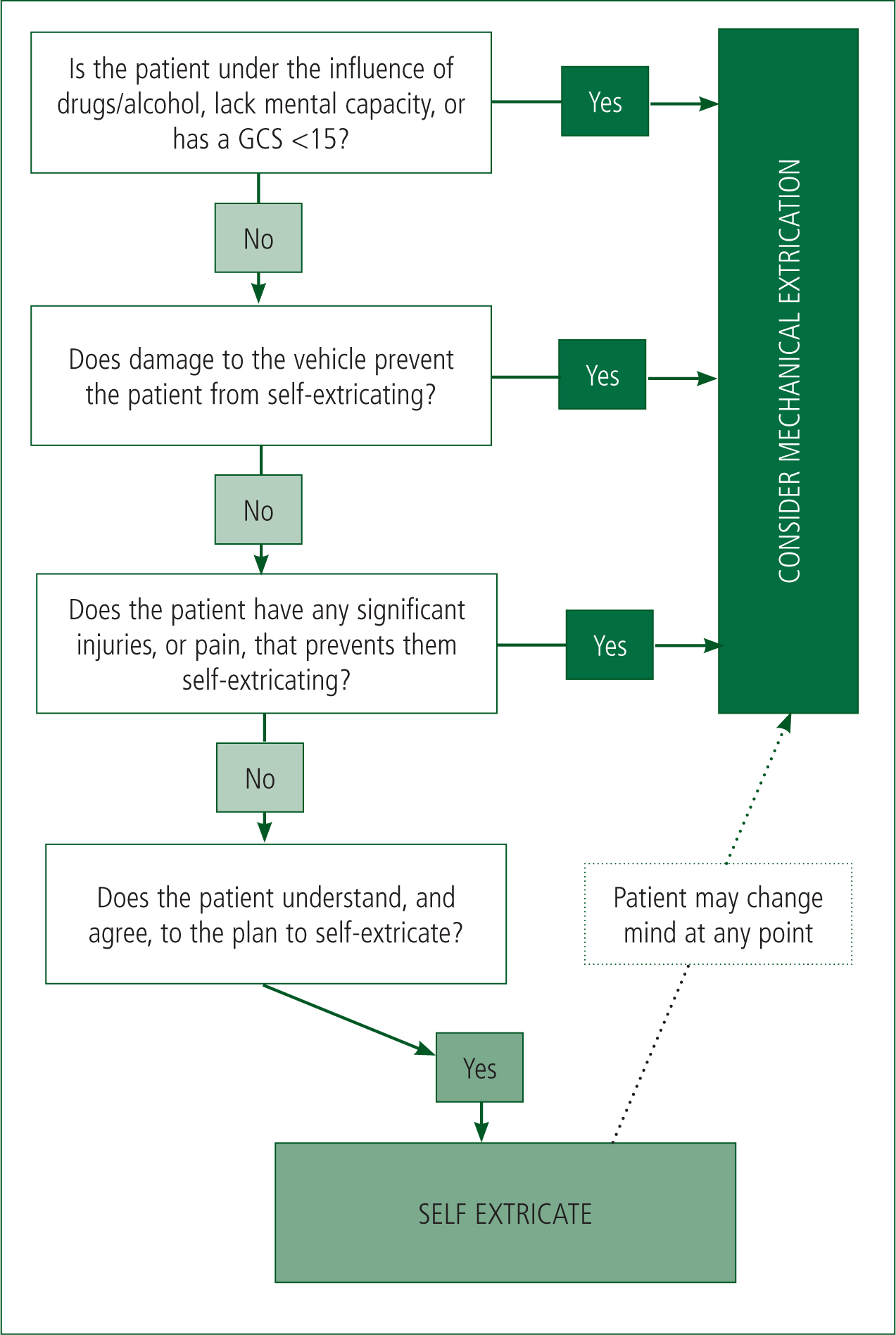
This article will not attempt to recommend when or how to immobilise and, while this is the subject of intense debate in the wider pre-hospital arena, it should be left to the clinician's local protocols to dictate. It is also recognised that mechanical extrication is necessary in a number of situations and this article does not aim to eliminate it. Non-alert patients will often require mechanical extrication, as will alert patients who are prohibited from self-extricating due to pain or vehicle damage. The ultimate aim is to create an algorithm to guide the pre-hospital clinician in extricating the systemically well, alert patient, and recommend further research in order to validate the tool.
Methods
This literature review incorporates two principal searches. Initially the review interrogated the Ovid Medline database, with search terms including ‘extrication’, ‘movement’, ‘pre-hospital’ and ‘cervical’. No limit was placed on age or language. Even with these fairly wide ranging criteria, only 44 articles were found. Examination of these articles found only four to be relevant to the subject in question, where relevant meant a direct focus on the movement of the cervical spine during extrication. The rest were primarily dismissed on the basis that they examined cervical immobilisation devices (generally a collar, or Kendrick extrication device), which is outside the scope of this review. Further to this literature search, additional literature was sourced from peer-reviewed material in order to support statistics or well-established facts.
Background
Despite a recent consensus statement (Connor et al, 2013), many pre-hospital clinicians live in fear of catastrophic spinal cord injury in their trauma patients. Almost all will have heard many anecdotes of the apparently well patient who, while walking around, becomes seriously ill following a brief turn of the neck. Subsequently, each working shift the decision of how to extricate a person involved in a road traffic collision (RTC) is faced by numerous pre-hospital clinicians and in an increasingly litigious society, precautions often far exceed what is necessary and/or sensible, and may even be detrimental. The result is countless examples of situations where alert, and generally uninjured patients, are being cut out of their cars (or occasionally, other people's cars who have provided refuge).
The clinician will often have faced the prospect of whether to immobilise prior to hospital conveyance and frequently, when this is deemed necessary, the patient will be extricated from the car using a variety of destructive methods such as the removal of the door, windscreen or roof by the Fire and Rescue Service (FRS) using hydraulic cutting procedures. This is often done not because the patient is unable to get out the car, but by the fact that the clinician has decided to immobilise and believes that any movement from now on risks exacerbating any unstable spinal injury and causing a catastrophic compromise to the spinal cord. In fact, while there is no doubt that trauma can cause unstable c-spine injury, the incidence in alert and stable patients is 1.7%, with only 0.1% continuing to develop significant neurological deficit (Benger and Blackham, 2009). The fact that some studies question the need for any pre-hospital immobilisation at all (Hauswald et al, 1998) reinforces the common sense argument that the clinically ‘well’ patient is unlikely to be deleteriously effected by stepping out of the car.
‘While there is no doubt that trauma can cause unstable c-spine injury, the incidence in alert and stable patients is 1.7%, with only 0.1% continuing to develop significant neurological deficit’
Spinal physiology
The spine is comprises a complex array of reinforcing parts, most of which ‘fail’ at a similar force. This allows for great structural integrity, with a minimum mass. It also means that injuries will generally be very minor, or very severe, with less room for injuries in between the two extremes. Very little energy is required to move an uninjured spinal column, thus an injured column will not be ‘easier’ to move, and in all likelihood will be a lot harder due to tissue oedema and a natural pain protection mechanism (Hauswald et al, 1998). This is anecdotally backed up, and in the literature, by emergency department physicians, many of whom have their own story of the self-presenting patient who has a severe c-spine injury, obtained many days earlier, that have been fully ambulant ever since with no large-scale deterioration (Cox and Barish, 1991; Jain et al, 2010; Weston and Gisondi, 2012; Momaya et al, 2014).
Injury patterns and kinetics are complex, but in road trauma involve the rapid deposition of large amounts of energy that dissipate through the crash sequence, often in an oscillating manner (e.g. as the head hits the airbag, then rebounds back, then forwards again). The force required to fracture the c-spine is in the order of 2 000–6 000 N—compare this with the force generated by ‘dangling’ an average head over the edge of a treatment table (40 N), and it is easy to see that the orders of magnitude difference are so great that further c-spine injury is almost impossible. It also demonstrates that a catastrophic injury, if it is to occur, will have occurred during the crash sequence (Hauswald, 2013). Further, in support of self-immobilisation, studies have shown that creating unnatural pivot points (e.g. a poorly fitting collar, or poor handling during mechanical extrication) will focus the force in to one area and contribute towards possible further injury (Lador et al, 2011). While these figures cannot be directly applied to a damaged c-spine, it provides a good frame of reference of the forces involved, and required, to cause injury.
It should be re-emphasised at this point that the self-extricating patient is not having their c-spine ‘cleared’ on scene. It is documented, for example, that as tissue oedema resolves a stable c-spine injury can become unstable over time and so the patient still needs clinical assessment in the emergency department with possible radiographic imaging.
Extrication difficulties
Many different techniques are adopted daily by pre-hospital clinicians in order to assist the immobilised patient from the vehicle. These often involve removal on an extrication board, through a mechanically removed roof or door, or a twist and slide through an open door. These methods all involve multiple resources, significant upheaval to the patient and vehicle, and a great deal of time. Anyone who has been ‘cut’ from a car, in training or otherwise, will know how much it exacerbates an already traumatic situation. In addition, this process can often take a significant amount of time, during which the patient is being delayed in their journey to definitive care, as well as often becoming cold (something widely accepted to contribute towards coagulopathy, and so is detrimental in the trauma patient), poorly analgesed and increasingly anxious. Recent studies also show the prolonged extrication patient to be at higher risk of venous thromboembolism (Rogers et al, 2011).
Nevertheless, it is still sensible practice to limit movement of a c-spine that needs to be immobilised. While we have seen little theoretical evidence for any movement worsening an injury, it will still help to reduce pain and anxiety if movement is limited during extrication. There is a disappointing number of studies that examine the extrication process, rather than the method of immobilisation. A pilot study of just a few participants showed the patient who self-extricated, albeit with a c-collar in situ, had far less movement in the c-spine than those who were mechanically extricated (Shafer and Naunheim, 2009). Their follow-up study, which recruited more people and evaluated movement in far more axes, supported this finding (Engsberg et al, 2013), and another recent, more focused, study has further supported the findings (Dixon et al, 2014). In the first two studies the unassisted patients who had no c-collar did have slightly more movement, but it must be remembered that these participants were known to be uninjured and, as Hauswald (2013) explains, the presence of any injury further stabilises the area, along with the auto-protective mechanism adopted by someone when in pain. All three studies show self-extrication is associated with less c-spine movement than traditional extrication methods. Furthermore, the patient will only move in planes that will not exacerbate an injury, rather than mechanical extrication where the patient has no control over which direction they are moved.
Furthermore, as we have briefly discussed, other extrication factors can be detrimental. The debate regarding the potential harm caused by c-collars rages on, and is not discussed here as their application in this instance will be clinician dependent. The importance of not extending scene times is not disputed nor is the emphasis on time to definitive care and the detriment of hypothermia in trauma. Average extrication times are not widely collected, but previous reports in the UK of 44 minutes appear accurate, and are unlikely to have reduced significantly (Wilmink et al, 1996). Clearly self-extrication will greatly reduce this figure.
The decision to self-extricate must be made in conjunction with the patient. Similar to the Joint Royal Colleges Ambulance Liaison Committee (Association of Ambulance Chief Executives, 2013) guidelines on immobilisation, they should be assessed as being alert and orientated (Glasgow Coma Scale (GCS) of 15), have full mental capacity and not be intoxicated by alcohol or drugs. In addition it must be judged that there are no other reasons for them not to self-extricate, such as the presence of severe injury to other body parts. However, with the emphasis on reducing time to definitive care, it may be prudent to allow a seriously injured patient to self-extricate, though this would be done on a case by case basis. The patient should have the plan explained to them and be happy to comply. Where the patient is mechanically trapped—for instance, by a door that will not open due to damage—mechanical extrication may to some degree be the only solution, though self-extrication can resume if the obstacle is removed and deemed safe. Where self-extrication is appropriate, full immobilisation measures can be prepared prior to extrication so the patient can be immobilised (in line with local protocol) as soon as possible once out of the vehicle. This is crucial to the process—allowing a patient to manage their own c-spine and self-extricate is not a declaration of absence of c-spine injury. Furthermore, the patient may at any point change their mind about the procedure, for example if it causes too much pain, and so plans should be in place to revert to a mechanical extrication if this occurs.

Discussion
In line with recommendations made by Conner et al (2013), self-extrication in alert patients that have sustained vehicular-related trauma is entirely appropriate in many circumstances and can reduce time, resource use and destruction of personal property, all of which can be of detriment to the patient. Catastrophic spinal injury is extremely rare, and even more so in the patient presenting as alert post-injury. Where an underlying injury is present, an injured c-spine is not easier to move than an uninjured one, and coupled with tissue oedema and the body's own protection mechanism, is likely to be more difficult to move. Further injury is very unlikely as the force required to create that injury during the accident process is several orders of magnitude greater than anything generated during normal movement. Crucially, a patient that self-extricates has been shown to move their c-spine less than those who are mechanically extricated. This is clearly an important point as it demonstrates that the supposed argument behind mechanical extrication (i.e. good immobilisation of the c-spine) may be invalid. Where the patient is alert and with mental capacity, and in the absence of a preventative circumstance (such as significant lower limb injury or mechanical entrapment), the patient can be invited to self-extricate, before employing spinal immobilisation in line with local protocol. It must be remembered that, like any form of consent, the patient may change their mind during the procedure and measures should be in place to account for this.
Example of algorithm use
A paramedic crew is called to moderate speed head on RTC and asked to attend the single male occupant driver of one of the cars. On examination the patient is alert and talking, and judged to have mental capacity by the crew. He is complaining of 4/10 pain around the C4-5 area as well as some pain across his chest, in keeping with a seatbelt injury. There is moderate damage to the front of the car, but the driver's compartment is grossly intact and the door opens easily. The airbag has deployed. The crew decide that this patient does require immobilisation for conveyance to hospital, but in keeping with the algorithm explain to him that they would like him to step out of the car prior to immobilisation, but that he should keep his head as still as he can. He agrees to this and understands he can change his mind at any time. Prior to self-extrication, the crew prepare the immobilisation equipment, assembling it on the road just a few yards from the car. In accordance with their local protocol it consists of a vacuum mattress on an ambulance trolley, head blocks and a cervical collar. The patient then steps out of the car and lies down on the mattress, at which point he is fully immobilised and conveyed to hospital following attention to his observations and analgesic needs.
Conclusions
The author has developed an algorithm (see Figure 2) that may assist the pre-hospital clinician in making this decision, and incorporates the principles discussed within this article. There is obvious scope, and need, for further focused research on the act of extrication and would be useful running alongside the current work being done on immobilisation methods. Larger scale randomised trials would be useful, especially to validate an algorithm such as the one suggested here, although due to the small proportion of negative outcome measures the population would need to be very large and would be logistically difficult.
Limitations
The author recognises that this is a narrative review, which has not undergone a full robust systematic process, and so will be subjective in parts. All of the studies into self-extrication have used non-injured patients, so the behaviour and movement of injured patients has yet to be studied, though it is likely to only further support the findings of existing studies.
Recommendations
The author is in the process of constructing a rigorous systematic review into the subject. Further, large scale, practical studies in to the biomechanics of self-extrication are required to further validate the findings of current literature. Information on the usefulness of the algorithm would be useful, whether this was feedback or via a larger scale validation process.

