‘The patient with burns presents a difficult challenge to most health care personnel. Apart from the serious nature of the injury, there is the patient's discomfort, the distress of the patient and their relatives, the loss of income and the compromise of their employment future and their uncertainty about the future’ (Emergency Management of Severe Burns UK Course, Pre-Reading—BBA/ANZBA).
Internationally burn injury is one of the major causes of death and disability. In high income countries major injuries have become less frequent but the total number of burn injuries per year remains oddly static despite all the preventative actions taken in many countries. In the UK it is estimated that approximately 130 000 burn injury cases are seen in emergency departments (ED) in England and Wales each year, but only 10% (11 600) of these require admission to a hospital and only 10% (1 200) of those constitute complex burn injuries (International Burn Injury Database).
Serious burn injuries are for life
Serious burn injuries are devastating events that leave patients with long-term physical and psychological challenges that are recognised by paramedics worldwide as one of the most horrific and challenging injuries known to the emergency medical and rescue services. Burn injuries may be extremely complex in their presentation, and any resulting complications may extend the need for expensive long-term management from months to years.
The final outcome for the burn injured patient will be influenced by the patient's age and the severity of the burn injury, which itself is dictated by the source (flame, hot liquids, chemicals, electricity etc.), the time in contact with the source, location of the burn injury on the patient's body (critical areas, whether circumferential), and medical and mental conditions. Additionally, the location of the patient at the time of injury, time to cooling, any suspected history of inhalation injury (carbon monoxide [CO], hydrogen cyanide [HCN]) and the effectiveness of the initial response and treatment by the responding emergency medical and rescue paramedics are all important.
All responding emergency medical and rescue personnel must consider the factors listed above which are subject to division into further subcategories (If heat is involved, is it wet or dry? If it is electricity is it domestic or industrial? Is the pathway external or internal? Skin condition? If it is a chemical is it acid or alkali and is it one of the specific and special case chemicals that require specific action?). Were correct irrigation/brush procedures performed or was an antidote employed? (If so, is it recognised and approved by the nationally recognised overseeing advisory body, is it in date, is it designed for that particular application).
Paramedics are the emergency department (ED) detectives on scene, they must use their eyes and ears to record as much information as possible (3 x history—scene, patient and pre-cooling) in the time available, as they become part of a very large burn care team when responding and treating severe burn injuries. They are the first on scene and must understand the need for a scene and patient history, pre-cooling history, a clear understanding of the various categories of burn injury and what to do and not do in each category, whilst at the same time assessing and estimating the burn injury. One of the important differentiators in complex burns is that they are not necessarily the ones affecting a large skin area. It may not be the area of skin but rather the mechanism of injury (electrical or chemical) or the circumstances (chronically ill) of the patient that make the clinical situation complicated and potentially risky. In other words, they must define the true mechanism of injury and understand the additional information that must be sought, recorded and handed on, as well as any specific action or inaction appropriate to that specific circumstance.
Many burn injuries require surgical intervention. The timing and extent of this is influenced by, and sometimes materially dictated by, the care provided by the pre-hospital paramedic. If there is not a clear clinical understanding of what this all means for the burn patient and the care pathway they are about to follow, due to a lack of training or inexperience, then the burn patient faces the prospect of a poorer outcome; possibly resulting in a more severely restricted lifestyle than might have been the case, which may in turn impact on their ability to work and earn a living for their future life.
All humans respond to a burn injury in the same way and this means you! It is worth noting that the responding emergency medical and rescue paramedics may be responding to a scene that is potentially very dangerous, and it may threaten their own survival as well as that of the patient. A concise knowledge of these potential concerns should be part of the initial paramedic training, recognising potential risks requires the knowledge necessary to unpick the often unique set of circumstances that may exist at the incident, e.g. although it is a basic requirement to provide oxygen support to a patient in shock, if the burn patient is still smouldering when you introduce supplemental oxygen (100% nrb) there may be an explosion on scene, possibly resulting in a fatal outcome for the patient and the responding paramedic crew. Many such adverse consequences that may follow a burn injury can be reduced by a clear understanding of the problem and effective prehospital management by the responding emergency medical and rescue practitioners.
Worldwide there are many references available that offer, what are perceived to be, the best treatment protocols for burn patients in their respective country/region. Many of these protocols are based on the ability/inability of each country/region to financially support the management pathway of burn injured patients. What is clinically best practice is open to debate but the complexity of burn care means it is rare for guidelines to be produced that will prove usable in all instances. It is always preferable for practitioners to understand the important variables at play in a given situation and act on the basis of that up-to-date knowledge and appreciation.
All burn injured patients are trauma patients
When a paramedic responds to severe burn injured patients there may be many distractions on scene. During assessment, the distracting nature of the sights and smells of burn injury plus the pain being suffered by the patient, coupled with the extreme reactions of bystanders and relatives can cause sufficient distraction such that important coexisting injuries can be missed and vitally important information to be overlooked by the paramedic. The application of a correct trauma response remains vital, with modifications for the burn injury that intersect with the routine trauma assessment, so as to accommodate the specific requirements of the injuries being considered.
Burn injured patients at the extremes of age require extra consideration. The potential for over or under fluid resuscitation is both real and may have far more rapid adverse consequences. This can arise from poor burn area (TBSA) assessment and/or a failure to appreciate the impact of other injuries.
The narrowness of the paediatric airway is well known but the effect of oedema around the pharynx following over-enthusiastic fluid resuscitation is not often appreciated, nor the potential for such oedema to particularly affect those with a high body mass index (BMI) at any age. In the elderly their ability to cope with significant fluid fluxes is understood, but with a burn, with the massive fluid shifts that occur, this sensitivity appears to affect even patients from their mid 50s onwards.
Burn injuries are by their very nature disturbing to assess and treat. This is not only because they affect the largest organ in the human body, skin, which at 16% of most adult's bodyweight proportionally constitutes a massive traumatic injury when a substantial proportion of it is injured. The skin is also in so many ways a communicator of our general well being, as well as acting as the patient's body armour. The age of the patient relates to the structure of the skin (integument) at the time of injury, the younger the patient the thinner the skin and the older the patient (>60 years) the thinner the skin, but for a completely different reason. Skin thickness also varies around the body as do the structures in the skin that promote healing, thus the potential for healing changes and the need for greater attention during the pre-hospital stage.
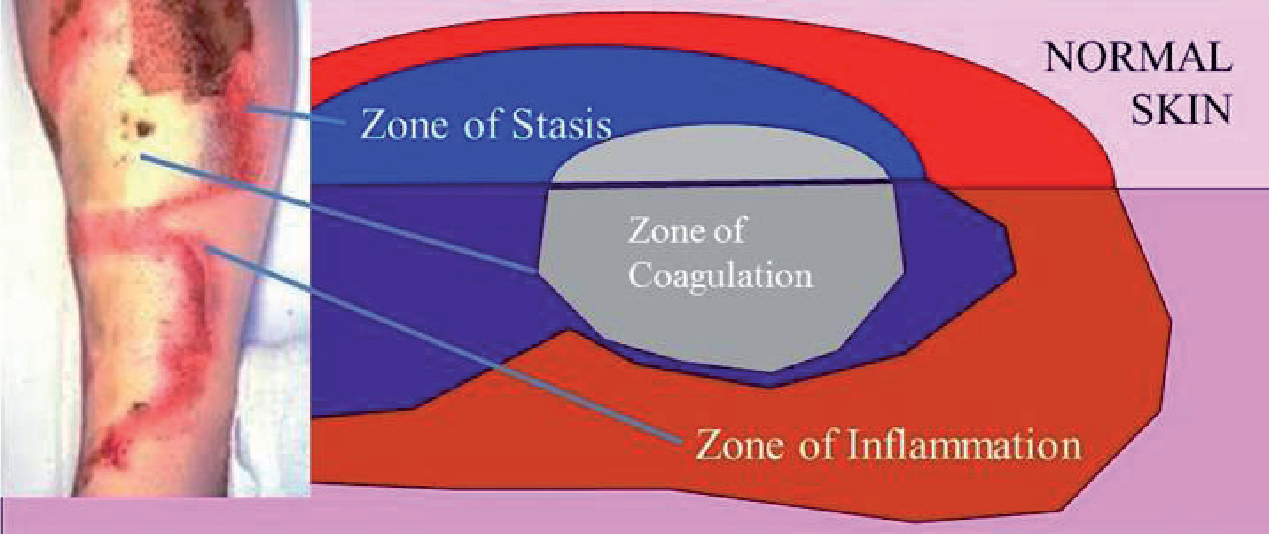
Although the clinical descriptions of burn depth vary around the world, they all acknowledge the Jackson Burn Wound Model (Figure 1), which describes a zone of coagulation, zone of stasis and the zone of hyperaemia (inflammation) in cutaneous burn injury. The aim is to maintain the viability of the zone of stasis, which requires a balance of approaches to cooling, fluid and wound management. Any imbalance can result in extension of the zone of coagulation with greater skin death and an increased need for grafting and thus scarring.
Total Body Surface Area (TBSA) of burn estimation in the pre-hospital setting is measured by the ‘Wallace Rule of Nines’, where the adult body is divided into areas that represent multiples of 9%. With the palmer measure (extended patient's palm and fingers ∼1% of their skin) used as an assist for random spot burns, serial halving is now not recommended in the pre-hospital setting (Joint Royal Colleges Ambulance Liaison Committee [JRCALC], 2013).
The area, depth (Jackson's burn zones) and location damaged by burn injury is important information for the receiving emergency department, as it indicates the severity of the injury, and the potential for systemic compromise. A burn injury may disrupt all systems homeostasis, routinely compromising the thermoregulatory and circulatory systems, allow microbial invasion from wound and gut, and instigate massive fluid loss (hypovolaemia) from the wound into the body's ‘third space’.
Depending on area burned it may cause the release of inflammatory mediators that overwhelm the local systems of control, creating a systemic reaction. The potential for cardiac and respiratory depression and shock is ever present; especially as the size of the injury grows and if pre-injury fitness of the individual is low. The systemic effects of a burn injury are a greater threat to life than the local effects.
Knowledgeable and skilled initial assessment and management is vital, not only to the survival of the individual but also the minimising of continuing injury that is present in the majority of thermal injuries. An appreciation of the amount of time following the event that first aid can be not only helpful but can totally change the necessary treatment and recovery for that individual is often not appreciated. In different circumstances appropriate first aid even after significant delay can still be effective. This is particularly so with chemical and electrical injuries, as well as the majority of thermal injuries, as long as central hypothermia or excessive wound contamination is avoided.
The location of burn injuries on the body will affect the on-going treatment the patient will undergo. There are critical areas of the body that if burnt will require specialised management; i.e. the hand, feet and parts of the face, ears and perineum.
The human hand has two aspects: the dorsal and palmer surface, both supported by a complex structure of bones connective tissue and muscles. The palmer surface is a working surface with no hair, the (glabellous) skin is thick with underlying dorsai interossei, thenar and hypothenar muscle bundles to provide resistance to abrasion and injury, and strength of flexion and grip. The dorsal surface (back of the hand) is not a working surface, contains hair on its surface and is thinner, but it has the duty of protecting the vascular structures, tendons and protective sheaths which allow the hand to function as a complete unit. Severe burn injury to either aspect of the hand may have a very poor functional outcome, compromising future functionality and ability to earn a living and self-manage.
Inhalation injury patients may on initial presentation/interview appear normal, but can deteriorate very rapidly, requiring immediate airway supportive intervention. Confusion and/or altered level of consciousness (LOC) at a fire or smoke scene are prime indicators of inhalation injury. There are three levels of inhalation injury: upper airway burns (supraglottic site), lung injury (by products of combustion inhaled into the lower airways) and systemic toxicity (absorption of inhaled products of combustion into the system). Swollen lips are a late sign and must not be ignored, but remain only an indication that inhalation may have occurred.
At a confined space fire scene ∼80% of patients die from inhalation injury. Here once again age is a major influencing factor in survival. Paramedics responding to a fire scene with patients reported must consider the potential for exposure to the ‘toxic twins’ carbon monoxide (CO) and hydrogen cyanide (HCN). Haemoglobin binds to carbon monoxide 240 times more easily than oxygen, generating carboxyhaemoglobin (COHb) which is then transferred throughout the blood stream no longer carrying oxygen.
The presence of carbon monoxide on scene is indicated by many factors. CO is a narcotic gas and may cause the patient to become unconscious or to unwittingly mask pain that otherwise would indicate associated injuries to the responding paramedic. There is no smell or taste to carbon monoxide. If the paramedic on scene is exposed to high concentrations of CO over a short period, i.e. 25 to 30 seconds, their ability to effectively treat the patient may be challenged, potentially resulting in a compromised outcome for the patient.
The effect of hydrogen cyanide (HCN) depends on whether exposure is a high or low dose. If a low dose, the symptoms of exposure are similar to those of carbon monoxide, prompting a possible misdiagnosis. Hydrogen cyanide is 24 times more lethal than carbon monoxide as it blocks the ability of cells in the body to absorb and use oxygen.
Very low dose exposure to hydrogen cyanide over a period of time may result in on-going cellular destruction. High dose exposure is rapidly fatal.
Pulse oximetry is not accurate in the presence of poisoning with either of the above. Specialised monitoring is required to establish the presence of carbon monoxide or hydrogen cyanide. If the fire scene is enclosed then inhalation injury must be considered. Recommended oxygen therapy: 100% oxygen with a non-rebreather mask (BBA and ANZBA, 2006).
Children are not small adults
From infant to maturity, as children progress through their growing cycle to achieve adulthood, their anatomy and physiology gradually change. As with adults, a primary and secondary trauma survey will be used to evaluate the burn injured child. Some 60% of burn injuries to children are caused by hot liquids. The density of the hot liquid will influence the pre-hospital treatment, in-hospital length of stay and on-going burn wound management. The density of a hot liquid for a scald injury must be considered. A higher temperature will be required to heat a thick liquid, resulting in greater tissue damage; a thinner liquid (water) may do less damage as it cools more quickly as it runs down the body surface, but may cover a greater area.
Outside of the normal complexities of a child trauma patient, the onset of shock may be rapid. Infants and children with a severe burn injury may suffer third space fluid shifts, considerable evaporative water loss and enter a compensatory phase prior to rapid decompensation. Older children who have a shiver mechanism may tire very quickly as their muscle mass is still quite small and underdeveloped, whilst a lack of shiver mechanism in infants under 1 year of age may increase the risk of developing severe hypothermia.
The maintenance of the respiratory system for an infant or child is challenging even for the most experienced paramedic. Depending upon age of the infant/child they may be an obligate nasal breather. Their tongues are larger, the larynx is more cephalad and their airways are smaller than that of an adult. Any form of blockage may compromise effective respiration.
The source of the burn injury will influence the potential outcome for the patient. It is vital to stop the burning process as soon as possible. A partial thickness burn will be generated from exposure to a temperature as low as 45 °C, if the exposure to that heat is for long enough. A full thickness burn requires only 69–70 °C for less than a second, and human bone carbonises at 650 °C. The average house fire burns at 750 °C. Flame is particularly destructive to human tissue and may rapidly progress to a full thickness burn (zone of coagulation).
Electrical injury will arise from a manufactured (AC/DC) source, such as domestic (single phase) or industrial (three phase), or from a natural source, e.g. lightning, which can produce temperatures in excess of 25 000 °C. Unless there is a clear understanding by the responding paramedic of the electrical pathway, potential internal and external burn injury, cardiac and respiratory compromise, and musculoskeletal damage (possibly requiring an urgent fasciotomy), the patient may not benefit from the extensive non-burn skills provided.
Chemical injury is an anomaly in that it is the one scenario where the offending medium must be removed from the site of insult prior to further management of the patient. Acid will do considerable coagulative damage, but alkali is far more destructive as it permeates into deep tissue, resulting in liquefactive necrosis. Once all the chemical has been removed from the site (flush/brush) cover with wet dressings (JRCALC, 2013). It is important to keep in mind that the responding paramedics may themselves become contaminated and compromised, with the potential for a fatal outcome while attending the patient.
Radiation burns. The increased use of radioactive materials in industry and medicine has raised the awareness for the potential for this material. It is very important to establish whether potential exposure exists, and if so, withdraw from the scene and call in the local Hazard Area Response Team (HART) who are specialists within the emergency services to deal with this situation. Specialised training is required for these contaminated patients.
Sunburn is often overlooked as a potential for serious burn injury. Once again age is an important factor, as the very young have an under-developed integument and may very readily suffer severe sunburn. If this is left untreated the injury can develop into a complex partial thickness burn over the next few hours and the unappreciated fluid loss threatens circulatory decompensation requiring advanced clinical attention.
Circumferential burn injuries (JRCALC, 2013) may compromise distal perfusion to a limb or digit and is a major concern for the receiving emergency department. Urgent surgical release (in the ED) of tissue tension by escharotomy may be required to ensure perfusion of the distal site. Circumferential burns of the chest or back are indicated by burn injury from axilla to axilla.
Cryogenic burns are caused from exposure to gases that have been liquefied at very low temperatures (-150 °C) and stored under extreme pressure, e.g. liquid nitrogen, LPG, LNG, refrigeration gases etc.
The resultant burn will present as desiccated tissue and can extend to deep muscle and bone. The management requires a clear understanding of the re-warming process. A variance of only 3 °C over the recommended re-warming temperature (40–42 °C) will only exacerbate the burn injury further. Attendance at an ED is required for these patients.
Boiling liquid expanding vapour explosion (BLEVE) is caused by the rupturing of specialised containment cylinders and transport vehicles used for the transport of liquefied flammable gases. Due to sudden impact, collision or derailment, the contained gas within leaks out to the atmosphere under extreme pressure and eventually ignites, generating a major explosion with high speed projectiles injuring and burning all those people within its damage radius.
Explosive events are the most complex event that any paramedic will attend in their lifetime. Understanding the kinematics of an explosion should be in the knowledge base of every paramedic. On response there is one question that must always be asked: ‘are there more explosives on scene waiting to kill me?’ if there is any doubt, do not enter the scene.
Once scene safety has been established, the paramedic mind goes into full treatment mode with the following considerations: what stage(s) involves your patients? Did they suffer one of the following: primary, secondary, tertiary or quaternary injuries or were they subjected to more than one stage? The injuries sustained in each category are very specific and must be suspected until triage and advanced clinical examination indicates otherwise. Due to the high pressure and heat produced as a result of an explosion, many severe burn injuries usually present. Remember the patient is a trauma patient and will need to be treated accordingly.
Hypothermia is a major concern with burn patients. Internationally the majority of burn injury presentations to the emergency department (ED) by ambulance or self-presentation are usually under 10–15% TBSA (Figure 2). The pre-hospital treatment will involve primary and secondary survey, pain relief, cooling, fluid resuscitation (if required) and associated management for shock etc. as required.

Adult patients who suffer burns in excess of 15–20% may have thermoregulatory compromise due to extensive damage to the integumentary structure. As a result they are no longer able to maintain core temperature and begin to cool very quickly resulting in hypothermia with all the complications this creates. Children and the elderly will, for obvious reasons, become compromised more quickly and require urgent corrective attention.
Current research into pre-hospital burn injury treatment has clearly indicated that efficient and effective cooling is very beneficial to the burn injured patient. Providing pain relief, arresting the progression of ongoing tissue necrosis and possibly assisting in the maintenance of the viability of the zone of stasis (depending on how early the cooling started), resulting in a better outcome for the patient.
Irrigation with copious amounts of water over a period of 15 to 20 minutes can be effective for up to 3 hours after the burn injury (JRCALC, 2013). Cooling the burn injury only and not the patient will be supportive to maintenance of core temperature. It is important not to over cool the patient by aggressive irrigation with cool running water (ice should never be used). The treatment plan is to keep it small and shallow (KISS [SBLS]). Cool only the burn, not the patient. In the absence of available running water, gel-based dressings may be used.
‘The principles of first aid are to stop the burning process and to cool the burn wound. Stopping the burning process reduces tissue damage. Cooling the surface of the burn wound reduces the production of inflammatory mediators and promotes the maintenance of viability in the zone of stasis. It therefore helps to prevent progression of damage that occurs in an untreated burn in the first 24 hours after injury’ (Emergency Management of Severe Burns UK Course Pre-Reading—BBA/ANZBA).
First aid education for the management of burns advocates cool running water over burnt skin to limit soft tissue damage. However, the water may itself constitute a risk; when obtaining the history of a burn injury, enquiries as to the source of water used should be sought as this will assist in predicting the likely pathogens and thus appropriate empiric antibiotics, pending culture results (Ribeiro et al, 2010).
The water source should be recorded. Is it static, brackish or running, domestic, industrial or wilderness? As these may constitute a severe wound contamination risk.
Clingfilm/glad wrap should not be used on a burn injury that remains hot. It may constrict necessary oedema and compromise the potential for distal circulation and viable maintenance of the zone of stasis. Clingfilm/glad wrap should never be used on or around the head and face.
History forms and records are very important for burn patients presenting to the ED. There remains a high risk that information can be lost or adulterated between the initial scene and the point of definitive care. Information loss and errors of communication can only increase risks for the patient with the potential for significant harm being done or allowed to happen.
Not only is it necessary to record the extended scene and patient history, it is also required that the pre-cooling history is recorded. This will support the responding paramedic on presentation of the burn patient to the ED. If the patient is hypothermic the chances are that the parents, friends or guardians of the patient employed aggressive cooling prior to the arrival of the paramedics in the belief that they were doing good.
Shock with cardiovascular compromise is the big factor with all trauma patients. Patients with serious burns are a major challenge in this regard. Burn patients may present with multiple reasons for developing shock. A burn patient with >20% TBSA may suffer a loss of intravascular volume to the interstitial space, resulting in burn shock (develops over a period of 6–10 hours). This is a combination of distributive, hypovolaemic and cardiogenic shock. Systemic shock may follow and electrical injuries will present with neurological deficit. The aim is to prevent rather than treat all forms of shock.
Conclusions
Inevitably burn injury carries with it a higher risk of death than many other forms of injury. The rate of such loss of life has reduced in recent decades but remains a constant feature of burn care. This is not only from the inevitable consequences of burn injury but also from the fact that there is a high complication rate, especially from infection. Among burn patients the potential for misadventure exists at every stage of the care pathway but is highest in the first 48 hours post injury.
Burn injury remains the most traumatic of survivable injuries. It has a profound effect on every body system when of sufficient severity, but even the most minor injury may change the individual's appearance, with inevitable social and psychological consequences. Functional losses with restricted scarring and contractures over joints have work and lifestyle consequences which can be career limiting with all of the financial consequences that follow.
As such, anything that can prevent burn injury in the first place or prevent the injury developing into something worse than it need be has to be the primary concern of EMS personnel caring for the victim at the beginning of their care pathway. This applies from the scene of injury all the way to final discharge from the burn care service, which for many patients is decades after the burn injury.
Burn injured patients never forget—the quality of your first response is vital to their future outcome.
