The rapid identification of patients with life-threatening conditions is the primary function of any emergency medical service (EMS) dispatch system. The most time critical condition is cardiac arrest, and the relationship between a delay in commencing resuscitation and subsequent survival from out of hospital cardiac arrest (OHCA) is well documented (Perkins at al, 2012). Accurate identification of patients with life threatening conditions during the call triage process can facilitate a range of interventions shown to benefit survival rates. In addition to facilitating the provision of the fastest possible ambulance response, benefits include telephone instructions on cardiopulmonary resuscitation (CPR) and the promotion of community defibrillator use (O'Keeffe et al, 2011).
Peri-arrest is the recognised period occurring either just before, or just after, a full cardiac arrest. In a period of peri-arrest the patient's condition is very unstable and care must be taken to prevent progression or regression into a full cardiac arrest. Whilst appropriate ambulance dispatch to patients already in cardiac arrest is important, the clinical benefits of early recognition of patients in peri-arrest could be considered equally important. O'Keeffe et al (2011) conclude that this is at least as beneficial as a rapid response to patients who are already in cardiac arrest.
To address this challenge, and with the support of the NHS Pathways user group, South Western Ambulance Service NHS Foundation Trust (SWAST) introduced an additional ‘Nature of Call’ (NOC) pre-triage system in 2012. The aim of NOC is to use a broad open question immediately prior to the commencement of the NHS Pathways triage process. Call takers chose from one of 60 NOC categories; developed by SWAST based on Override Protocol Priorities (OVPs), to allow early identification of the likely category of call. This indicates to dispatchers those calls needing immediate allocation and calls where they could wait for further information. After the NOC category has been selected, call-takers initiate the full NHS Pathways triage process. If the NOC produces a delayed response disposition, but if NHS Pathways subsequently find evidence indicating higher acuity, NOC will be overridden. The dispatch priority assigned to each NOC category continues to be refined on a regular basis, in response to evidence of cardiac arrest frequency.
In 2013, the National Director of Operations Group (NDOG) and the National Ambulance Medical Services Directors (NASMeD) established a working group to remove general inconsistencies in Red 1 coding between ambulance trusts in England. They addressed inconsistencies between NHS Pathways and Advanced Medical Priority Dispatch (AMPDS) coding outcomes; maintained a record of what individual trusts are coding as Red 1, and designed a control process to govern any future trust-level local additions to Red 1 codes.
In addition to the existing Red 1 definition, a new definition of Red 1 was agreed by this working group and trialled in November 2013 as the highest priority dispatch code. The definitions are detailed in Table 1.
| Previous Red 1 Definition | New Red 1 Definition |
|---|---|
| Not breathing and not conscious |
|
This new definition was predicated on the assumption that providing the fastest response to those patients who are at greatest risk of progressing to cardiac arrest would reduce the number of cardiac arrests that occur, and improve overall patient outcomes. Widening the Red 1 definition was also expected to capture more patients in a peri-arrest and life-threatening condition.
Aim
The aim of the evaluation was to assess whether the new Red 1 definition had an impact on the patients that receive a Red 1 response.
The condition of the patient on arrival of ambulance personnel was analysed, and compared before and after the introduction of the New Red 1 definition, and between the Red 1 subgroups (i.e. the previous Red 1 definition and the new Red 1 definition).
Method
The evaluation was completed in the East and West divisions of SWAST, where NHS Pathways is in use. All attended incidents that received a Red 1 response between 12/11/12 and 31/12/12, and between 01/11/13 and 31/12/13 were included.
Where available, clinical records for each incident were individually reviewed. Auditors collected data reported by the attending ambulance personnel. Data were recorded as to whether patients were deceased on arrival (DOA) (this is where resuscitation is determined to be futile by a clinician) had a valid ‘do not attempt resuscitation’ (DNAR) order (a legal order advising clinicians not to attempt resuscitation), were resuscitated by SWAST staff, or were not in cardiac arrest (non-arrest).
Patients who were not in arrest on arrival and did not arrest during the pre-hospital phase of care were further reviewed to establish the severity of their presenting condition. The National Early Warning Score (NEWs) (Royal College of Physicians (RCP), 2012) was retrospectively applied to each patient using the details recorded on the Patient Clinical Record (PCR). The system uses value ranges of key clinical observations to assess acute illness, and to indicate the level of response required (RCP, 2012). Patients who were aged under 16 years or pregnant were excluded according to national guidance.
Results and discussion
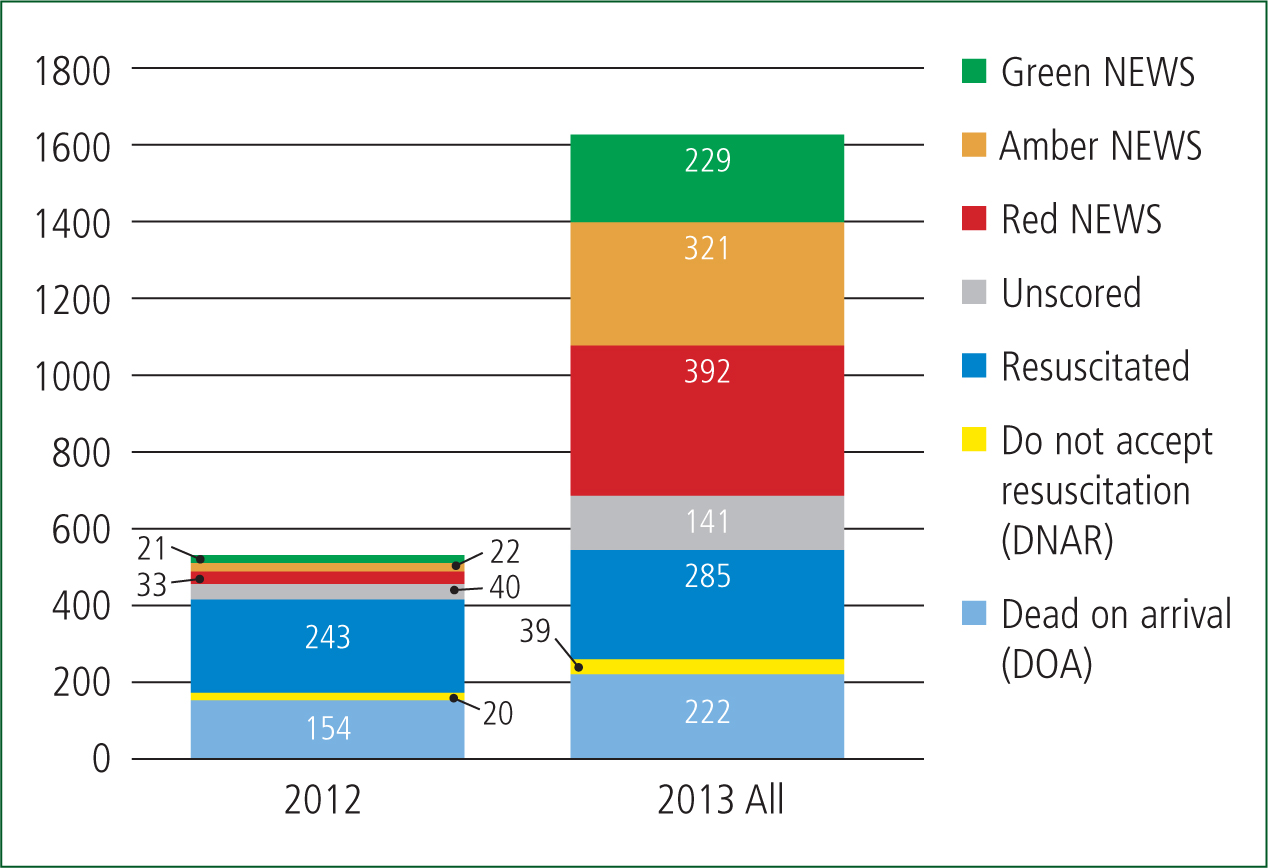
There were n=543 Red 1 incidents in the first reporting period (12/11/12 to 31/12/12), compared to n=1629 Red 1 incidents in the second reporting period (01/11/13 to 31/12/13). The breakdown is detailed in Table 2; for the second reporting period patients were also separated into those identified by the previous Red 1 definition and the additional patients identified by the new Red 1 definition.
| Sample | 2012 | 2013 | 2013 |
|---|---|---|---|
| R1 Definition | Previous | Previous | New |
| Red1 | 543 | 898 | 731 |
The 2012 sample began on 12/11/12, as this was the starting date of the NOC trial. Therefore, this sample does not include the first 105 incidents that received a Red 1 response occurring between 01/11/12 and 11/11/12. This equates to 16.2% of Red 1 patients for the 2012 sample data.
Clearly, more patients received a Red 1 response in 2013 than 2012, even accounting for the 105 shortfall in Red 1 incidents in the 2012 sample data. This would be expected given the expanded definition.
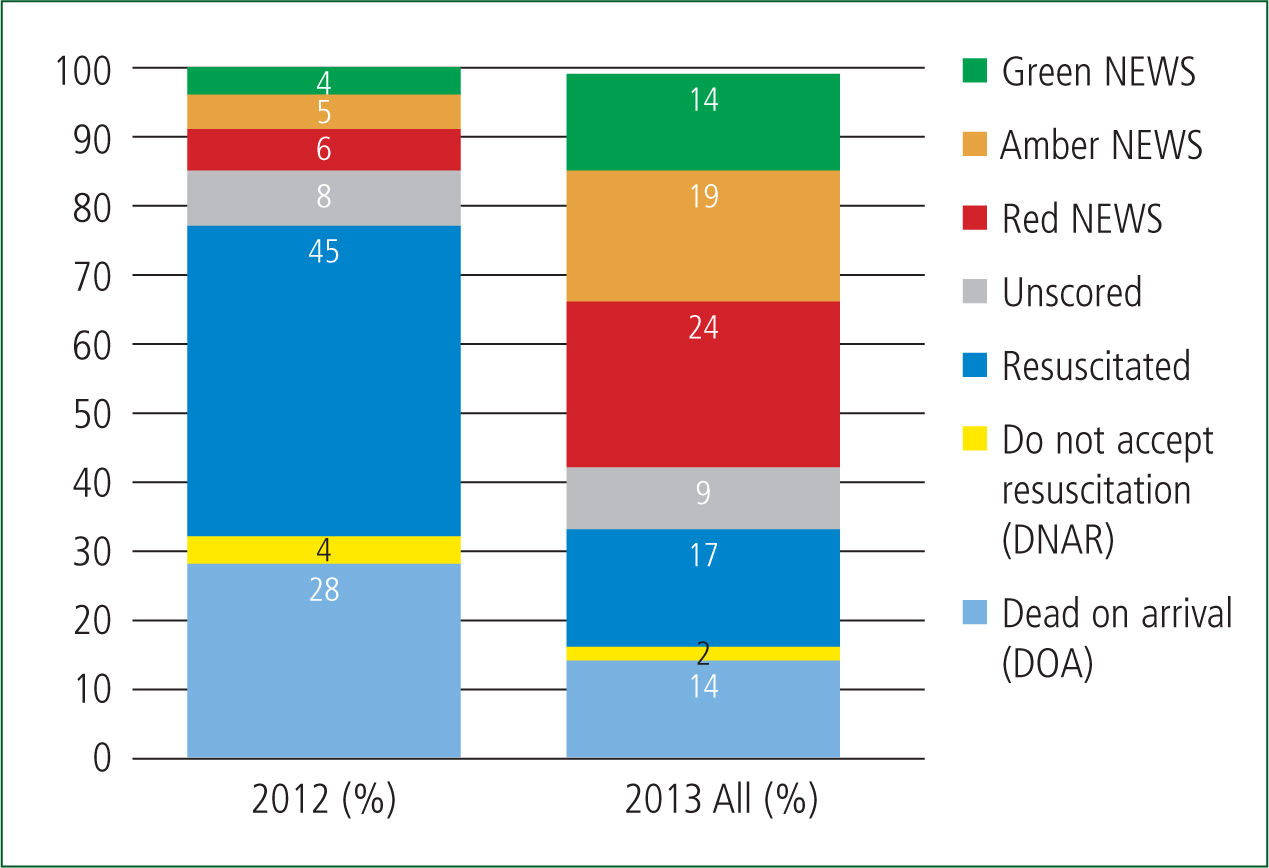
Comparing the 2012 sample after adjustment to include an additional 16.2% of patients (to account for the shortfall of 11 days in the 2012 reporting period) with the new Red 1 definition identified an additional 353 patients who had a red NEWS score. Patients with a red score under the NEWS system are considered to be critically unwell, with the RCP recommending that they receive an immediate assessment by a team with critical care competencies. For the purposes of this paper, the red NEWS category is therefore taken as patients with the most life-threatening presentations, requiring a Red 1 response.
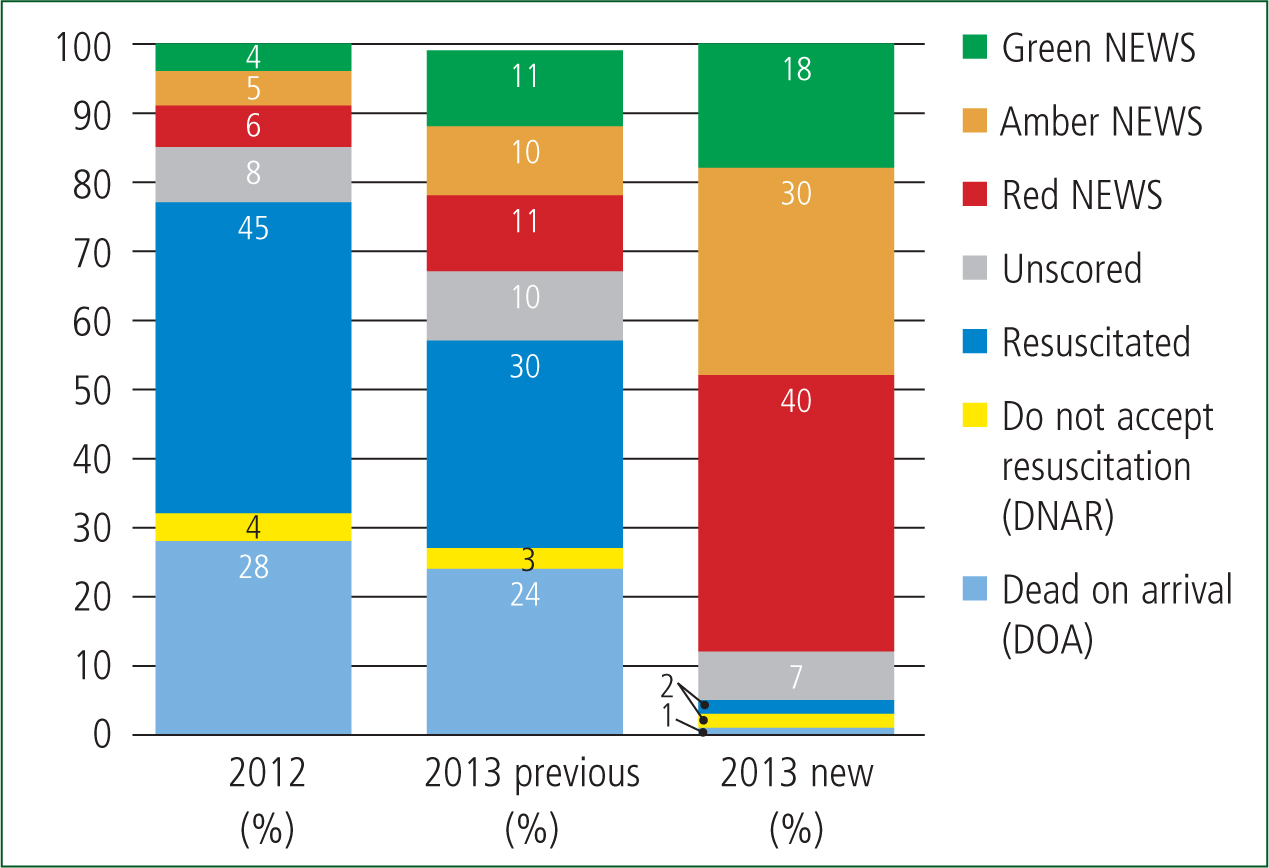
Analysing in terms of proportion provides further support to these findings. Figure 3 breaks down the 2013 results into those identified by the previous Red 1 definition and those identified by the new Red 1 definition.
When the cases identified by the new Red 1 definition only were analysed further, the majority (95%) of patients did not experience a cardiac arrest. However, the new definition was significantly better at identifying critically unwell patients with a red NEWs score (40%).
While the sensitivity for identifying critically unwell patients and those in cardiac arrest was significantly increased, as expected, the new Red 1 definition had poorer specificity. The proportion of urgent but not life-threatening patients indicated by an amber NEWS score was 30% within the new Red 1 definition, compared to 10% in the previous Red 1 definition. The identification of unwell patients indicated by a green NEWS score was 18% (new definition) and 11% (previous definition) respectively. Further work is needed to establish the severity of patients within the green NEWS score category. As NEWS is based on physiological parameters, a limitation of this approach is that some time-critical conditions, such as myocardial infarction, which have a high risk of progressing to cardiac arrest, may not cause significant abnormalities in physiological observations and present with a green NEWS score.
The 2012 Red 1 group and the 2013 Red 1 patients identified by the previous criteria were expected to be similar because they used the same definition. Similar proportions of patients were found to be deceased on arrival or with a valid DNAR in each group. However, the proportion of patients receiving resuscitation reduced in 2013 and was, in effect, replaced by patients who did not arrest.
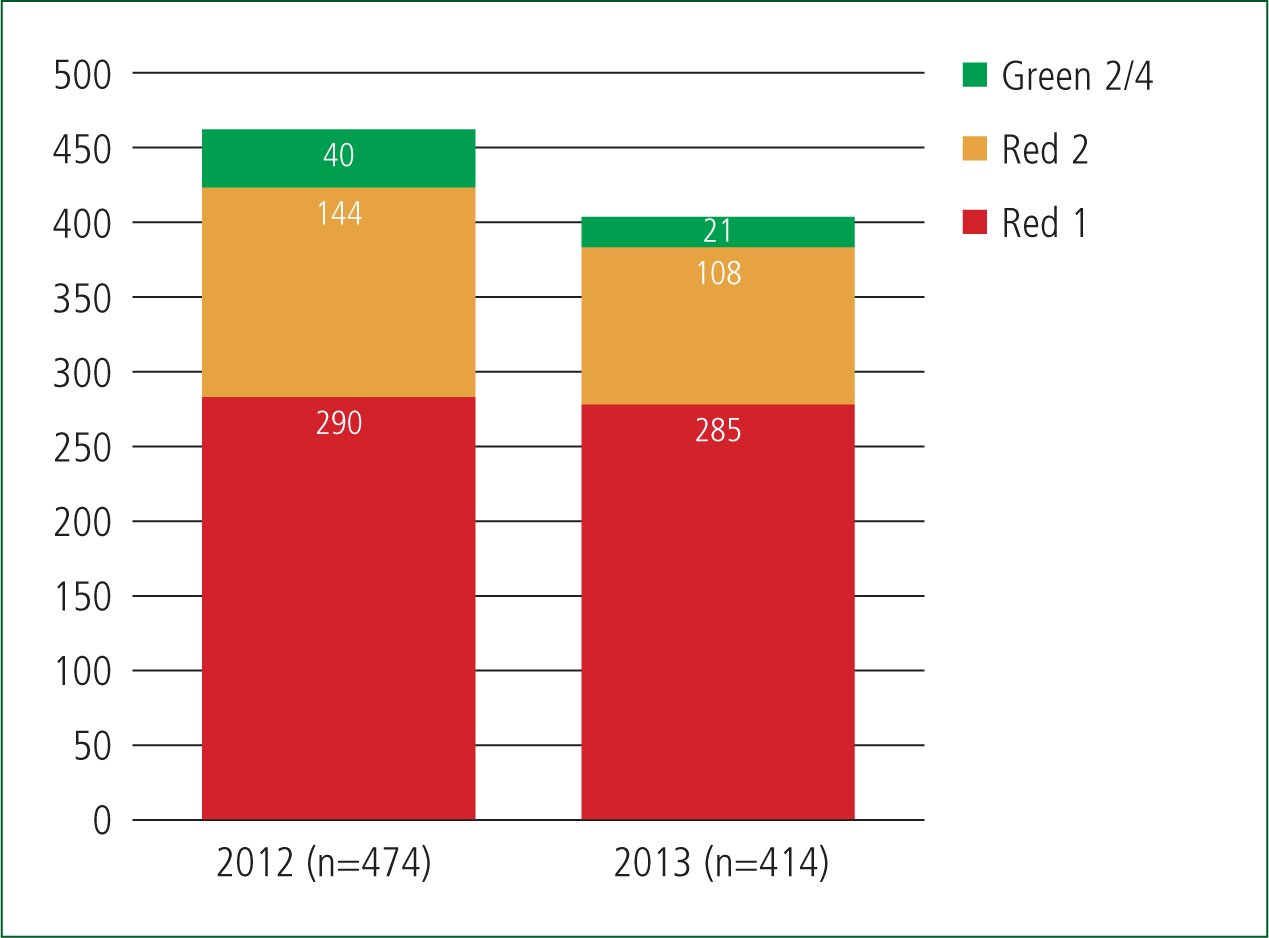
Further analysis was conducted to establish the impact of the revised Red 1 definition on the total number of resuscitation attempts. Due to the potential for cardiac arrests to be identified in other categories of call, the analysis reviewed Red 1, Red 2 and Green 2 calls. As the overall 2012 sample omitted the first 11 days of the month, the results within the dataset were adjusted accordingly. The distribution of dispatch codes for all patients receiving resuscitation during the two sample periods is presented in Figure 4. This analysis demonstrates that the total number of resuscitation attempts decreased by 11.7%.
This is a small-scale evaluation; however, the results are encouraging. Data analysed suggest that identifying and providing an early response to an additional 353 patients who were assessed to be critically ill may have led to a reduction in the number of patients who subsequently experienced a cardiac arrest.
The cases that could not be NEWS scored are detailed in Table 3. The unscored sub-group presented in Figures 1–3 is detailed further in Table 3.
| Reason | 2012 (n) | 2013 (n) | 2013 (n) |
|---|---|---|---|
| R1 Definition | Previous | Previous | Split New |
| Under 16 years | 13 | 42 | 30 |
| Record unavailable | 27 | 44 | 20 |
| Patient refused observations | 0 | 2 | 0 |
| No patient contact | 0 | 0 | 1 |
| Ambulance stood down | 0 | 1 | 1 |
| Total | 40 | 89 | 52 |
A large proportion were children who were unsuitable for the application of NEWS.
Conclusion
Although this is a small study, there appeared to be a reduction in the number of patients who required resuscitation under the new Red 1 definition. This supports the hypothesis that more life-threatened patients are captured by the new definition, and the more rapid response may have diminished their likelihood of experiencing a cardiac arrest.
Overall, a larger number of patients were included in the new Red 1 definition in 2013 than in the previous 2012 version. Whilst the operational impact of this increase is outside of the scope of this paper, it is important that it is viewed in the context of the total number of incidents to which the ambulance service responds. Red 1 cases represented 0.8% of the total number of incidents completed during the previous definition sample period and 2.0% during the new definition period; this remains a very small proportion of ambulance incidents.
Of note, under the new definition a greater number (43%, n=957) of Red 1 patients did not arrest, and more were within the red NEWS score category (353 additional patients, equating to 22% of all Red 1 patients).
This leads to the conclusion that the new Red 1 definition may be more sensitive than the previous definition for the identification of patients in cardiac arrest, and those with the highest risk of experiencing a cardiac arrest. The decrease in the proportion of patients receiving resuscitation categorised as Red 2 or Green 2 when using the new Red 1 definition is a further indication of the positive impact of the new definition on patient care.
This increase in sensitivity comes at the cost of an anticipated decrease in specificity, with proportionally more urgent but not life-threatening (amber NEWS) and unwell (green NEWS) patients being identified. It is widely accepted that any move to increase sensitivity will have the opposite impact on specificity, with patients being over-triaged. Further reviewing the green NEWS sub-sets may enable triage changes to be identified that could improve specificity, without adversely affecting the current sensitivity.

