The benefits of simulation across disciplines in healthcare education have been recognised and its use is now commonplace (NHS England, 2024). Simulation-based education involves guided, structured activities and experiences to reflect realistic situations, thereby enhancing the knowledge, decision-making, critical thinking, skills and attitudes of learners and preparing them for clinical practice (Dalwood et al, 2020; Wheeler and Dippenaar; 2020, Diamond and Bilton, 2021).
While healthcare regulators such as the Health and Care Professions Council (2021) and the Nursing and Midwifery Council (2019) recognise the role of simulation within practice-based learning, they also recognise that it is not an end in itself and must be integrated into overall approaches to education to ensure meaningful and effective learning experiences and outcomes that are in keeping with standards for education.
However, as highlighted by Alinier and Oriot (2022), simulation as an educational approach not only applies to undergraduate healthcare students but also extends into postgraduate education, enabling continuing professional development and recertification or revalidation requirements to be met. Such use of simulation allows experiential learning within the high-risk industry of healthcare (Alinier and Oriot, 2022), particularly for events that are infrequently encountered (Murray et al, 2019), within environments posing low risk to both patients and participants (Imbriaco et al, 2021).
Simulation fidelity, sometimes referred to as authenticity, concerns to what extent the simulated experience reflects or approaches reality (Association for Simulated Practice in Healthcare, 2016) and reproduces reactions, interactions and responses expected in the real world (Lioce et al, 2020). Lioce et al (2020) further defined high-fidelity simulation as that which provides experiences that are extremely realistic, involve the learner in a high level of interaction and may include humans or manikins. In low-fidelity simulation, which may include task trainers (training device or specialised model designed to help learner practice a specific skill or task) or case studies, learner participation is not reliant on external control or programming by a facilitator or operator.
However, as Tun et al (2015) discussed, while fidelity has long been considered intrinsic to simulation and plays a crucial role in its educational effectiveness, reality does not necessarily have to be faithfully replicated; rather, clues and stimuli have to be such that the participant can make responses to them which are appropriate and accurate.
This literature review will examine the evidence base to determine if simulation fidelity influences the learning of students or other participants, in particular those working in the prehospital healthcare environment.
Methods
This narrative literature review was undertaken during February and March 2023. Searches of selected databases were undertaken (Table 1).
| Database | Key words | Limiters | Total results |
|---|---|---|---|
| MEDLINE | “simulation training” OR “simulation education” OR “simulation learning” |
2013–present |
53 |
| CINAHL Ultimate | “simulation training” OR “simulation education” OR “simulation learning” |
2013–present |
28 |
| Scopus | “simulation training” OR “simulation education” OR “simulation learning” |
2013–present |
8 |
| ScienceDirect | “simulation training” OR “simulation education” OR “simulation learning” |
2013–present |
6 |
Ethical approval was not required as this was a narrative literature review. Publications were initially sought from within the past 5 years as suggested by Parahoo (2014), with this then being expanded to 10 years to seek a balance between the most recent literature and a sufficient body of evidence in keeping with recommendations by Cronin et al (2008) and Hewitt-Taylor (2017).
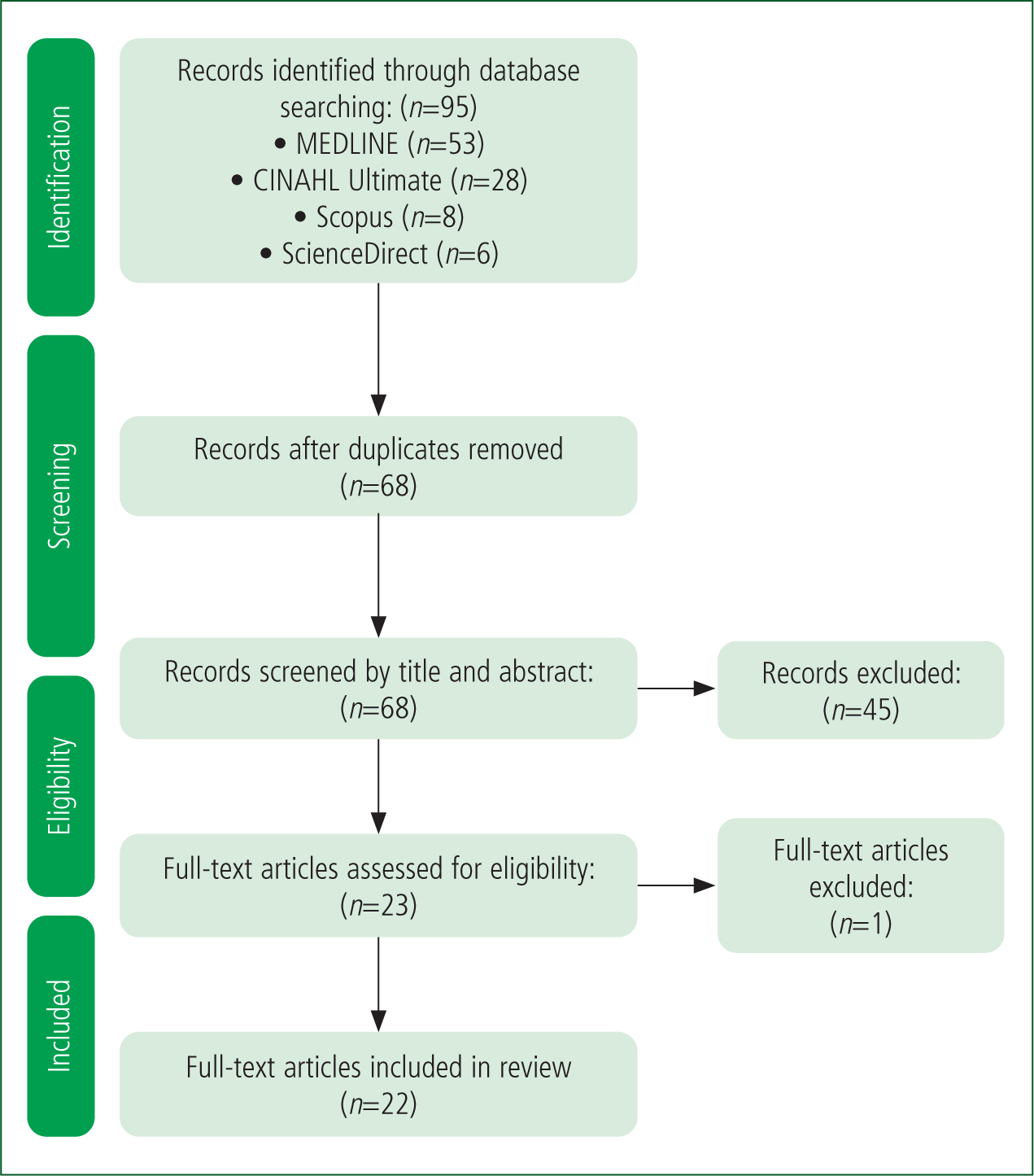
Results from database searches were screened by title and abstract then by review of full-text articles to ensure the most relevant literature was included.
To ensure transparency of results from database searches, as recommended by Aveyard (2018), an amended PRISMA flow chart (Figure 1) was completed. The PRISMA flow chart (Moher et al, 2009) records the identification of the literature, screening, eligibility and final articles included in the review. In total, 22 articles were included, which form the basis of this review.
Critical review and discussion
As part of the critical evaluation of the literature, three themes were identified using an approach similar to that described by Aveyard (2018).
First was the role of the model of simulation, which includes addressing the fidelity of the simulation. Second was the role of the simulation facilitator in creating a safe environment, free of risk for the participants and where fidelity of the simulation played a part in suspending disbelief. Third was the need for simulation to be underpinned by sound educational theory, thereby ensuring the simulation and level of fidelity met the needs of participants and learning outcomes. Table 2 outlines the themes and relevance of studies to each.
| Theme | |||
|---|---|---|---|
| Author (year) | Simulation model | Role of the facilitator | Educational theory |
| Tun et al (2015) | ✓ | ✓ | |
| Roh et al (2016) | ✓ | ||
| Hernandez et al (2019) | ✓ | ✓ | |
| Howland et al (2019) | ✓ | ||
| Murray et al (2019) | ✓ | ||
| Dalwood et al (2020) | ✓ | ||
| Kim and Lee (2020) | ✓ | ✓ | ✓ |
| Lerner et al (2020) | ✓ | ||
| McKelvin and McKelvin (2020) | ✓ | ✓ | ✓ |
| Mills et al (2020) | ✓ | ||
| Peterson et al (2020) | ✓ | ✓ | |
| Wiggins et al (2020) | ✓ | ✓ | |
| Zhang et al (2020) | ✓ | ✓ | |
| Wheeler and Dippenaar (2020) | ✓ | ✓ | ✓ |
| Diamond and Bilton (2021) | ✓ | ✓ | |
| Hunter et al (2021) | ✓ | ✓ | |
| Imbriaco et al (2021) | ✓ | ✓ | |
| Sandy et al (2021) | ✓ | ✓ | ✓ |
| Alinier and Oriot (2022) | ✓ | ✓ | ✓ |
| Lammers et al (2022) | ✓ | ✓ | |
| Larraga-Garcia et al (2022) | ✓ | ✓ | |
| Avery et al (2023) | ✓ | ||
Simulation model
The delivery of simulation can be broadly described in stages: briefing and familiarisation of participants; delivery of and participation in the simulation; and debriefing and reflection (Tun et al, 2015; Kim and Lee, 2020; Lerner et al, 2020; McKelvin and McKelvin, 2020; Wheeler and Dippenaar, 2020; Wiggins et al, 2020; Lammers et al, 2022).
In undertaking careful, precise preparation of a simulation, key decisions must be made about the level of fidelity and modality to be used, based on the intended learning outcomes, the perceived level of participants and the capacity of the chosen modality to engage participants (McKelvin and McKelvin, 2020).
Alinier and Oriot (2022) identified that various frameworks or models have been proposed that describe how fidelity in simulation is used in the context of healthcare education. However, Tun et al (2015) asserted that, despite proposed models for fidelity of simulation, there is a lack of evidence-based, generalisable theories to guide the fidelity requirements of education. In addition, Diamond and Bilton (2021) stated that no comprehensive methods or even best practice guidelines for setting up and running effective simulations for paramedicine educators exist.
Tun et al (2015) outlined a multidimensional framework or model of simulation fidelity that identifies key dimensions of the patient, healthcare facilities and clinical scenario, but also seeks to address limitations that prevent the suspension of disbelief required of participants. Alinier and Oriot (2022), who contributed to the previous work by Tun et al. (2015), progressed this model to consider four key elements, namely the ‘environmental, patient, semantical, and phenomenal dimensions’ (Alinier and Oriot 2022), each of which can have its own level of fidelity. However, Wheeler and Dippenaar (2020) identified that providing the patient dimension of such a model in a high-fidelity simulation of the prehospital environment is difficult, with a lack of equipment such as manikins. In this context, delivering simulation in the prehospital environment must consider the fidelity of each dimension outlined by both Tun et al (2015) and Alinier and Oriot (2022) to maximise fidelity in dimensions that is achievable.
Additionally, situational awareness of participants, as discussed by Hunter et al (2021), and difficulties in taking in information beyond their ‘circle of focus’ (Alinier and Oriot 2022) means that potentially only essential aspects of physical fidelity, functional fidelity, environmental stressors and realistic environments need to be recreated (Tun et al, 2015; McKelvin and McKelvin, 2020; Wheeler and Dippenaar, 2020; Alinier and Oriot, 2022; Lammers et al, 2022).
Role of facilitator
The terms educator, tutor, instructor or co-ordinator are used interchangeably with facilitator throughout the literature (Kim and Lee, 2020; McKelvin and McKelvin, 2020; Imbriaco et al, 2021; Sandy et al, 2021; Alinier and Oriot, 2022). For this review, the term facilitator will be used to describe all or any of these roles within simulation.
In simulation, the facilitator role has been identified as pivotal (Wheeler and Dippenaar, 2020). Tun et al (2015) pointed to the key role of facilitators in orientating participants to simulations, enabling students to navigate the experiential learning process, and in supporting debriefing and reflection. Alinier and Oriot (2022) referred to facilitators needing to orchestrate the simulation, with successful facilitation being itself an art.
However, facilitation of simulation extends beyond orchestration of the parts. As Hunter et al (2021), Imbriaco et al (2021) and Alinier and Oriot (2022) noted, healthcare in general is a high-risk industry with paramedics and those working in the prehospital arena experiencing environments that are unpredictable and complex and where staff safety may be at risk. Therefore, while by its very nature, simulation does not involve real patients so removes the risk to patients (Alinier and Oriot 2022), facilitators have a role in ensuring a low-risk environment is created for participants that creates psychological safety and promotes learning (Tun et al, 2015; Hunter et al, 2021; Imbriaco et al, 2021; Sandy et al, 2021). However, while creating a safe learning environment, care must be taken by facilitators to ensure the fidelity of the simulation promotes engagement and buy-in to the scenario so participants can suspend disbelief and achieve the learning outcomes (Tun et al, 2015; Wheeler and Dippenaar, 2020; Sandy et al, 2021; Alinier and Oriot, 2022).
Murray et al (2019) stated that education in healthcare is not structured to provide realistic experiences in high-risk but infrequently encountered events such as disasters within communities. Simulation therefore provides opportunities for exposure to and improvement in the management of events that rarely occur but may have significant consequences when they do (Howland et al, 2019; Murray et al, 2019; Kim and Lee, 2020; Mills et al, 2020; Wheeler and Dippenaar, 2020; Diamond and Bilton, 2021; Lammers et al, 2022).
Consequently, when facilitating simulation of such rare events, levels of fidelity must be carefully considered so participants do not become ovewhelmed (Lammers et al, 2022). As Wiggins et al (2020) said, the potential for cognitive overload should be considered by facilitators in overall instructional design, and consideration given to creating opportunities for scaffolding through increasing levels of skill mastery and attributes as simulations develop in both complexity and fidelity.
Debriefing and reflection are key elements of simulation in which facilitators play crucial enabling roles (Kim and Lee, 2020; McKelvin and McKelvin, 2020; Peterson et al, 2020; Wiggins et al, 2020; Imbriaco et al, 2021). Simulation provides opportunities to provide prompt feedback and reflection (Avery et al, 2023), the benefits of which have been explored by Race (2014).
In a study that compared debriefing led by an instructor (facilitator) with that led by peers, Roh et al (2016) concluded that performance and satisfaction were higher with instructor-led debriefing; they also found the interaction with facilitators and timing of the debriefing were more important than the type of debriefing used. Furthermore, Avery et al (2023) found that a move away from summative assessment-based training to a model of simulation followed by debriefing that was structured and led by a facilitator had positive responses both from participants and faculty.
Such use of structured debriefing was also highlighted by Wiggins et al (2020), who used the Debriefing Assessment for Simulation in Healthcare (DASH) tool to gain debrief information that assisted in supporting the case for further regular training. As Bolton and Delderfield (2018) highlighted, reflective practice allows for searching questions that have not been asked previously to be framed appropriately and brought into the open, enabling both future and current professionals to learn from experiences such as simulation.
Educational theory
With the rise in use and development of simulation-based training within clinical education, a key principle is that a sound educational strategy must surround the simulation model to ensure its effectiveness (Zhang et al, 2020).
Murray et al (2019) maintained that the complexity of simulation scenarios means that to maximise learning, an understanding not only of experiential and constructivist theories but also of theories of reflective learning is required. A common assertion within the literature reviewed is that simulation allows for the concept of building upon existing knowledge and experience, or the creation of a scaffolding of knowledge and experience (McKelvin and McKelvin 2020; Wiggins et al, 2020; Alinier and Oriot 2022). This concept of scaffolding is also discussed by Gopee (2018) when considering both constructivism and Ansubel et al's (1978) assimilation theory in the broader context of cognitive learning theory and experiential learning.
Therefore, when considering the fidelity of simulation, as McKelvin and McKelvin (2020) discussed, high-fidelity simulation can enhance individualised learning by providing opportunities to identify and rectify errors in a safe environment. However, clarity is required when developing simulation session objectives so as to select correct simulation methods, such as high- or low-fidelity, to achieve the objectives (Larraga-Garcia et al, 2022). For a given simulation, there may be no single approach that is correct and a combination of approaches may be used, resulting in mixed-reality simulation (Peterson et al, 2020).
Similarly, simulation provides opportunities to focus on particular skills or tasks in isolation until mastery is achieved before they are incorporated into more complex simulations where skills can be consolidated (Wheeler and Dippenaar, 2020). Simulation therefore addresses key principles of andragogy, with adult learners enabled to improve their thinking and performance through applying previously acquired knowledge and experience (Alinier and Oriot, 2022).
The ability of peers to provide immediate feedback was identified by Avery et al (2023) as vital to increasing depth of knowledge.
As discussed by Gopee (2018), experiential learning, which can be achieved through simulation, is key to reflective learning and a central component of cognitive learning theory.
Simulation and reflection therefore provide opportunities to bridge theory-practice gaps (Sandy et al, 2021). With sound instructional design, simulation-based education provides opportunities for sessions to be designed with debriefing, feedback and reflection as core concepts (Wheeler and Dippenaar, 2020), thereby optimising learning.
Additionally, using reflection before simulation to identify learning needs and for students to set their own learning objectives can inform the instructional design and choice of simulation topic as well as enhance both individual and team performance (Peterson et al, 2020).
Discussion
Simulation-based education enables both students and experienced practitioners (including those undertaking postgraduate education) to undertake activities and have experiences that enhance their knowledge, decision-making, critical thinking, skills and attitudes and better prepare them for practice (Dalwood et al, 2020; Wheeler and Dippenaar, 2020; Diamond and Bilton, 2021; Alinier and Oriot, 2022).
Opportunities for experiential learning within the low-risk environment of simulation are crucial, particularly in relation to events that occur rarely but which have significant consequences (Murray et al 2019; Diamond and Bilton, 2021; Imbriaco et al, 2021; Alinier and Oriot, 2022).
The educational effectiveness of simulation is, crucially, influenced not just by the overall level of realism or fidelity used but also by the choice of model of fidelity as well as using levels of fidelity appropriate to scenarios and each element of the model (Tun et al, 2015; Alinier and Oriot, 2022). There are particular challenges with providing high-fidelity simulation for the prehospital environment (Wheeler and Dippenaar, 2020), meaning that choices on fidelity levels should be focused on the areas where those taking part will be concentrating and making use of most of their sensory capacity (Tun et al, 2015; Alinier and Oriot, 2022).
Simulation facilitators play a pivotal role (Wheeler and Dippenaar, 2020) in what Alinier and Oriot (2022) refer to as orchestrating the simulation. Their role involves preparing students to participate in simulation, guiding them through experiential learning processes and supporting the crucial steps of debrief, feedback and reflection (Tun et al, 2015). The importance of the facilitator role is emphasised in creating low-risk environments where risks are minimised and psychological safety promoted so learning is nurtured (Tun et al, 2015; Hunter et al, 2021; Imbriaco et al, 2021; Sandy et al, 2021); this is particularly important during simulations of rare events with significant consequences to prevent cognitive overload and not overwhelm participants (Wiggins et al, 2020; Lammers et al, 2022).
Debriefing and reflection are important in simulation and facilitators have a key role in enabling reflection to happen (Kim and Lee, 2020; McKelvin and McKelvin, 2020; Peterson et al, 2020; Wiggins et al, 2020; Imbriaco et al, 2021). A role of the facilitator is to ensure debriefing, feedback and reflection on simulation are undertaken and in a timely manner (Roh et al, 2016; Kim and Lee, 2020, McKelvin and McKelvin, 2020; Peterson et al, 2020; Wiggins et al, 2020; Imbriaco et al, 2021).
Sound instructional design of simulation, achieved through choice of simulation modality and level of fidelity, can optimise learning and enhance both individual and team performance through embedding reflection at its core and bridging theory-practice gaps (Peterson et al, 2020; Wheeler and Dippenaar, 2020; Sandy et al, 2021).
Simulation must be based on a sound educational strategy (Zhang et al, 2020). Successful simulation uses the concept of scaffolding and building on existing knowledge and experience (McKelvin and McKelvin, 2020; Wiggins et al, 2020; Alinier and Oriot, 2022) within a broader context of cognitive learning theory, experiential learning and constructivism (Gopee, 2018). The opportunities that simulation presents to increase in complexity and fidelity as skills are mastered and attributes are developed (Wiggins et al, 2020) may be broadly compared to learning outcomes increasing through the levels of the Structure of the Observed Learning Outcome model (Biggs and Tang, 2011).
Limitations
During the literature search, it was noted that there is limited research on simulation fidelity in the prehospital environment. Search results may have been restricted by use of only peer-reviewed studies in the English language. A search of alternative databases or grey literature may have led to further relevant studies being included.
The literature search was undertaken by a single researcher, which has the potential to introduce bias. As the study was a narrative review, a critical appraisal of included studies was not undertaken.
Conclusion
Evidence from this review demonstrates the benefits of simulation for both students and registered paramedics. Simulation provides particular benefits in training for rarely occurring events that have significant consequences.
However, literature specific to the fidelity of simulation in the prehospital environment remains sparse and would benefit from further studies being undertaken.
Simulation should have sound instructional design, achieved through choice of simulation modality and level of fidelity. This can optimise learning and enhance individual and team performance, and reflection should be embedded at its core.
While the delivery of high-fidelity simulation for a prehospital setting may be difficult to achieve, the use of simulation in this environment, with levels of fidelity appropriate to the scenario and that recognise the sensory capacity of participants, can be educationally effective.
In addition, effectiveness is influenced by the choice of simulation model, having a dedicated facilitator and being based on a sound educational strategy. This combination allows learning outcomes to be met and the gap between theory and practice to be bridged more effectively.


