A 72-year-old man has collapsed with signs of a stroke. He lives at home with his wife and dog. He is reasonably independent with good mobility. However, several years ago, he was diagnosed with Alzheimer's disease and his cognitive function has steadily declined since. He has been treated for hypertension for the last decade or more.
This morning, his wife heard a thump from upstairs and she found him slumped across the bed. He was groaning and was incoherent. He had an obvious facial droop on the left side. He had also been incontinent of urine.
His wife dialled 999. When the paramedics arrived, he was identified as FAST-positive with a likely diagnosis of stroke.
His vital signs were:
Cardiac monitoring was commenced and the electrocardiogram (ECG) in Figure 1 was taken.

What does the ECG show?
Interpretation of the ECG rhythm
This is an example of a atrial fibrillation (AF) with an uncontrolled ventricular rate.
AF is the commonest sustained abnormal heart rhythm disorder (arrhythmia) (National Institute for Health and Care Excellence (NICE), 2021). Approximately 2% of the adult population is affected (NICE, 2021). It is typically detected as an irregular pulse or an irregular rhythm on an ECG. However, most patients with an irregular pulse will not have AF, with ectopic beats being a more common cause (NICE, 2021).
Patients with AF are around five times more likely to have a stroke, with one in every five strokes in the UK being a result of known AF. In AF, clots may propagate in the left atrial appendage and pass into the cerebral circulation where they embolise (Lamassa et al, 2001). A patient's risk of stroke can be identified using the CHA2DS2-VASc scoring system (Lip et al, 2010) (Figure 2).
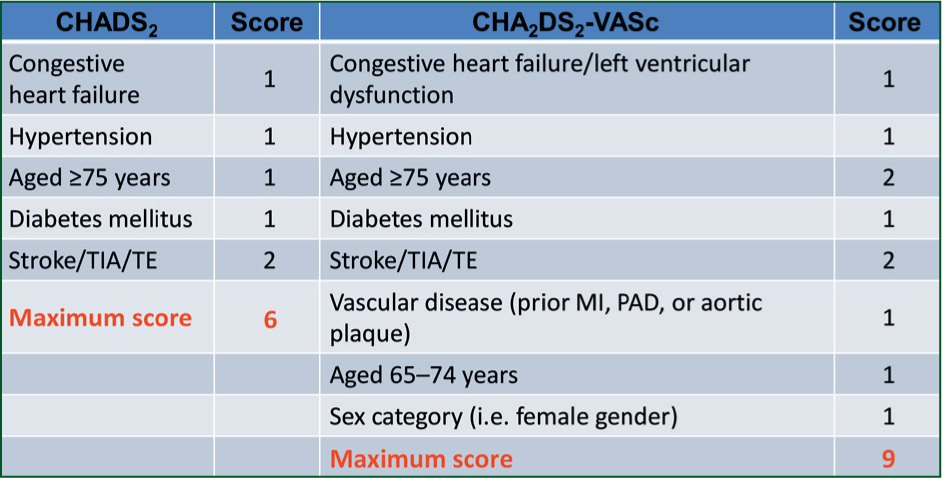
Oral anticoagulation is considered when CHA2DS2-VASc indicates a significant risk of stroke.

