Traumatic cardiac arrests have generally poor outcomes. A retrospective database search of 909 traumatic arrests treated by a physician led, established, inner city helicopter emergency medical service (HEMS) service showed a 7.5 % survival rate for this patient group (Lockey et al. 2006). This could be considered a ‘best case’ survival rate where patients received early, high level care and the majority of reversible causes were identified and if feasible treated.
The main correctable causes are hypoxia, hypovolaemia, cardiac tamponade, hypothermia and tension pneumothorax (Kloeck, 1995). The pathophysiology of these causes make closed chest compressions at best minimally effective if performed prior to their reversal (Vanden Hoek et al, 2010). Other patients have medical causes of cardiac arrest in traumatic settings, this should be suspected in a patient whose clinical condition does not correlate with the injury they have sustained, and treated as such (Hopson et al, 2003).
Using established techniques, paramedics are able treat hypoxia with airway management and ventilation with 100 % oxygen.
Pre-hospital re-warming techniques are designed to prevent worsening of hypothermia in those patients in cardiac arrest, and it is therefore important to identify hypothermic patients, establish these techniques and rapidly convey the patient to hospital, where definitive re-warming can be achieved.
Hypovolaemia can be treated with control of external haemorrhage, judicious fluid resuscitation and rapid transport to hospital. Non-blood product resuscitation has a poor success rate and pre-hospital hypovolaemic cardiac arrest is almost universally fatal in the UK population (Lockey et al. 2006). It is worth noting however that a recent observational study of traumatic cardiorespiratory arrests in Afghanistan demonstrated an 8 % survival to discharge rate (n=4). Of these four survivors three had arrested due to exsanguination (Tarmey et al, 2011); suggesting that successful resuscitation can be achieved in these patients by arresting blood loss and aggressive pre-hospital blood product resuscitation. Unfortunately due to logistical reasons this is difficult to achieve in most of the UK.Cardiac tamponade caused by a haemopericardium is ineffectively treated by needle pericardiocentesis. For a chance of successful resuscitation a thoracotomy is required within 10 minutes of loss of output to decompress the pericardium. However, this is currently a skill only offered by senior physicians either in the pre-hospital environment or in the emergency department (Asensio et al, 1998a; Asensio et al, 1998b; Coats et al, 2001).
This paper reviews the current guidelines for the management of tension pneumothorax by paramedics during cardiac arrest. It examines whether it is likely to be effective and compares it to other methods of management.
Tension pneumothorax
Tension pneumothorax is a build up of air between the lung and the pleura lining the chest wall. It occurs when a defect in the lung, chest wall or airways operates as a one-way valve, allowing air into this potential space during inspiration; as it is not released during expiration this trapped air increases in volume. This results in pressure being placed on the lung tissues resulting in compression, raised intrathoractic pressure and eventually mediastinal shift, a reduction in venous return to the heart and consequent circulatory collapse.
The condition tends to progress slowly in spontaneously ventilating patients, but progresses rapidly when patients are ventilated due to the greater pressures involved (Leigh-Smith and Harris, 2005).
Current recommendations
The Joint Royal Colleges Ambulance Liaison Committee ( JRCALC) guidelines currently recommend the decompression of suspected tension pneumothoraces during cardiac arrest using needle thoracocentesis. It is advised in patients with clinical evidence of tension pneumothorax and those in traumatic cardiac arrest with evidence of thoracic trauma, bilateral decompression is suggested unless certain of which side to decompress (Walter et al, 2006).
Is needle thoracocentesis effective in cardiac arrest?
There is mounting evidence that needle decompression of a tension pneumothorax is unreliable, though accurate success rates are unknown. Many papers suggest that insufficient catheter length might be at fault (Sanchez et al, 2001; McLean et al, 2011; Inaba et al, 2011; Inaba et al, 2012) however other potential reasons for failure to decompress are shown in Table 1.
In the context of cardiac arrest, return of spontaneous circulation (ROSC) following needle decompression would strongly suggest a decompressedd tension pneumothoras. Where there is no improvement in a patient's condition the continued presence of tension pneumothorax cannot be ruled out (Rojas et al. 1983). This may result in a difficult dilemma occurring as to whether to reattempt the procedure or move to hospital without further decompression attempts. A report on three patients with pulseless electrical activity (PEA) arrests secondary to respiratory distress would suggest that this might not be an uncommon problem in patients with cardiac arrest secondary to tension pneumothorax; needle decompression failed in all three patients, but all achieved ROSC on placement of chest drains (Castle et al. 2005). Had tension pneumothorax been ruled out on the basis of failed needle decompression it is highly unlikely ROSC would have been achieved.
While needle decompression has a role in temporising symptoms of tension pneumothorax in spontaneously breathing patients, as was concluded by Simons (2011) in a review of JRCALC guidance, it must intuitively fail to decompress a tension pneumothorax in a ventilated patient, as with every breath delivered air enters the space between the lung and chest wall under positive pressure rapidly re-expanding the penumothorax. Typically minute volumes in such patients are 6 l/min (based on tidal volumes of 600 ml and a respiratory rate of ten); even if a patent 14G cannula was perfectly sited and draining freely it could not be expected to adequately deal with flow rates of this magnitude.
A porcine model of PEA arrest due to isolated tension pneumothorax seems to confirm this; it showed a 36 % treatment success rate with needle decompression, compared to 100 % with tube thoracostomy; despite needle decompression being performed under laboratory conditions, with ultrasound identifying the thinnest area of chest wall (Martin et al. 2012).
Finger thoracostomy
Finger thoracostomy was a procedure first described by Deakin et al (1995), physicians of London HEMS. The technique is in essence the initial stages of a tube thoracostomy (chest drain) without the insertion of a tube, and is shown in Figures 1–4. The procedure creates an open pneumothorax, allowing the lung to rapidly re-expand, in a patient who is being ventilated with positive pressure.




It is therefore suited to intubated cardiac arrest patients, as these are likely to be ventilated with positive pressure. It offers advantages in the pre-hospital environment over tube thoracostomy, in this patient group, as it allows the lung to re-inflate in the same way, but is quicker, easier to perform and requires less training (Deakin et al. 1995).
It is also a rapid diagnostic test for the presence of a tension pneumothorax. Should a finger sweep identify lung tissue, it is unlikely that a significant pneumothorax is present.
Finger thoracostomy is a relatively simple procedure to perform with the correct training, and it has been suggested it could be performed unsupervised by experienced paramedics where needle decompression has failed (Deakin et al. 1995). Many critical care paramedics now have it within their skill set.
Post-procedure management
When the author initially presented the concept of paramedic led finger thoracostomy, concern was raised over the management of patients who had ROSC and returned to spontaneous, negative pressure, ventilation. The concern is that negative intrathoracic pressures can suck air into the pleural cavity, causing on open pneumothorax (Deakin et al. 1995). In a physician-led critical care service sedative and paralytic agents (general anesthesia) can be given to a patient to continue positive pressure ventilation. However when this is not available a patient will be left with bilateral open pneumothoraces. It should be noted that ROSC with return to spontaneous ventilation is an extremely positive outcome for a patient in traumatic arrest and a fear of its occurrence should not stop the procedure being performed. In this eventuality it is proposed that the surgical wounds should be treated as open pneumothoraces; and covered with one-way chest seals (Asherman, Bolin or Russel) (American College of Surgeons Committee on Trauma, 2008). Should the patient continue to be ventilated, no covering is needed. (Deakin et al. 1995)
Should a patient deteriorate a sterile gloved finger can be inserted into the thoracostomy sites and finger sweeps made, to ensure the tension has not re-accumulated.
Complications
Tube thoracostomy carries with it risks of several complications, for instance; infection, leading to empyema and massive haemothoraces secondary to iatrogenic injury. (Aylwin et al 2008) It would be reasonable to assume that simple thoracostomy, as a similar, though less invasive, procedure, would carry similar risks, however in a series of 55 patients of an Italian HEMS service undergoing finger thoracostomy no serious complications were documented and no recurrence of tension pneumothorax occurred. (Massarutti et al, 2006)
When should the chest be decompressed?
While current guidelines empower paramedics to perform bilateral needle decompression during traumatic cardiac arrest, there is evidence to suggest it is performed less frequently in paramedic led traumatic arrests compared to those a doctor attends (Mistry et al. 2009). This is unsurprising considering the lack of exposure of UK paramedics to tension pneumothorax, the relative difficulty in making the clinical diagnosis (despite the impression given on resuscitation courses (American College of Surgeons Committee on Trauma, 2008) and the concern over procedural complications.
A traumatic cardiac arrest is stressful for those who attend them infrequently and thus every effort should be made to adopt an effective protocol relying on minimal decision making, to rapidly treat and rule out possible reversible causes (Coats et al. 1995).
As the potential complications of finger thoracostomy are minimal; particularly when weighed against the poor outcomes of a patient in cardiac arrest with a missed tension pneumothorax; it could be reasoned that all patients in traumatic cardiac arrest should have bilateral decompressions in this manner, unless an experienced clinician on scene can assure themselves that no chest trauma is likely (a tiny minority of patients).
Conclusions
It would seem that there is evidence to doubt the effectiveness of needle decompression in the management of tension pneumothorax, particularly in the context of traumatic cardiac arrest.
As tension pneumothorax is an important reversible cause in traumatic cardiac arrest care in this patient group would seem to be improved if paramedics, who in most UK cases will be the lead clinicians on scene, were equipped with a reliable method of rapidly treating it or excluding it as a diagnosis.
Finger thoracostomy safely fulfils this role and thus the author proposes that paramedics should be trained in a rapid and simple technique to perform a finger thoracostomy.
Additionally, JRCALC should consider recommending that bilateral thoracostomies be performed in all traumatic arrests, unless a senior clinician on scene can be absolutely sure no chest trauma has occurred.
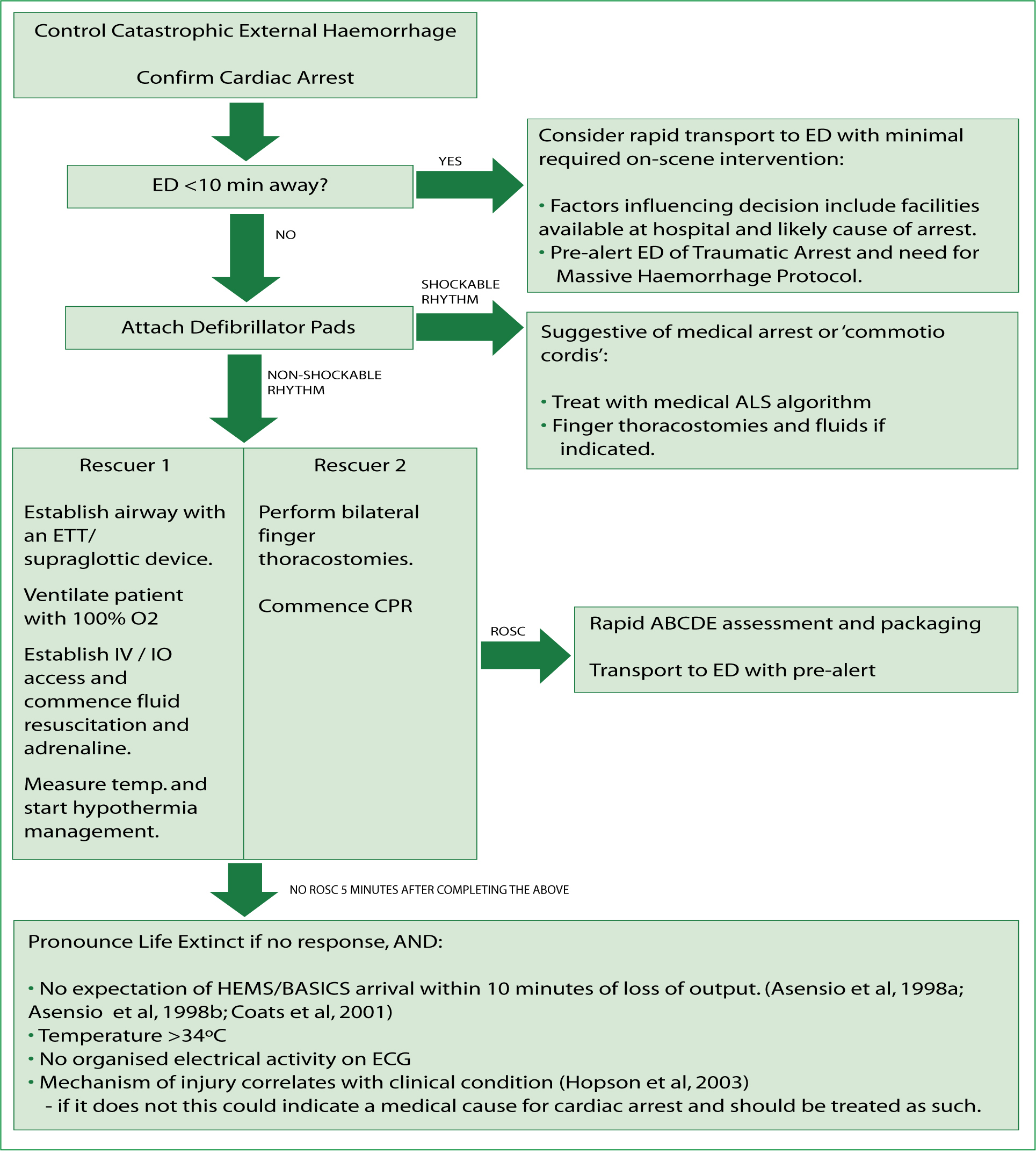
A further recommendation is the introduction of a new protocol for treating traumatic cardiac arrest that focuses on the rapid treatment of reversible causes; rather than chest compressions, early defibrillation and drug treatment as in a medical arrest, a possible algorithm is proposed in Figure 5.