There are almost 16 000 traumatic deaths worldwide every day (Krug et al. 2000), and it is estimated that up to 40% of trauma deaths are the result of haemorrhage (Kauvar et al. 2006). Tranexamic acid (TXA) is a proven life-saving treatment for trauma patients in the pre-hospital environment, and has been shown by the CRASH-2 study to reduce the risk of death by bleeding if administered within 3 hours, acting by inhibition of fibrinolysis (Shakur et al. 2010). Greatest significance was shown when TXA was administered within 1 hour of injury.
CRASH-2 further found that there was no increase in vascular occlusive events as a result of TXA, and reported an incidence of pulmonary embolism (PE) and deep-vein thrombosis (DVT) post TXA to be 0.7% and 0.4% respectively. There has since been little follow-up regarding the incidence of venous thromboembolism (VTE) post TXA use in the pre-hospital trauma environment.
Based on the CRASH-2 findings, TXA is now available to UK pre-hospital care teams treating major trauma patients. TXA has been available to Great North Air Ambulance Service (GNAAS) clinicians since 2011, where it is indicated for trauma patients with signs or injuries that could suggest potentially significant haemorrhage. This is consistent with the JRCALC indication of ‘time critical injury where significant internal/external haemorrhage is suspected’ (UK Ambulance Services 2013). A dose of 15 mg/kg is used in children and adults, with a maximum dose of 1 g. A subsequent infusion should then be given in hospital as per the CRASH-2 protocol.
GNAAS treats an average of 900 patients per year, and a significant number of these have suffered major trauma. The evaluation described in this research spotlight focuses upon the use of TXA by GNAAS and considers individual patient outcomes in hospital, including the need for blood products and VTE rate.
Methods
A service evaluation was performed with analysis of patient outcome by the review of patient report forms (PRFs). Patients who received pre-hospital TXA were identified and further analysis of their outcomes was performed at the two receiving local major trauma centres.
Data collection
GNAAS operates two aircrafts, as well as a response car out of hours; all patient encounters are documented on a paper PRF. All forms were analysed during a 12-month period from April 2015 to March 2016 (n=846). Patients were identified at hospital using the picture archiving and communication system (PACS). Specific imaging of the pulmonary vasculature or limbs was reviewed to assess for the presence of PE or DVT, and this was confirmed based on a radiologist report. Transfusion data are collected routinely as part of the GNAAS ‘Blood on Board’ policy, and were available for review. Trauma Audit and Research Network (TARN) information is also routinely collected, and injury severity scores (ISS) were available for review.
Results
Based on the retrospective analysis of PRFs, 106 patients received pre-hospital TXA (age range: 3–82 years; median: 39 years), which accounts for 12.5% of GNAAS patients during this time period. The type of trauma sustained is shown in Table 1. Of these patients, 93 (88%) had a cardiac output upon arrival at hospital; 32 (30%) received a pre-hospital transfusion of packed red cells in addition to TXA.
| Trauma type | n=106 | % |
|---|---|---|
| Road traffic collision (RTC) | 77 | 73 |
| Penetrating | 12 | 11 |
| Falls | 12 | 11 |
| Crush | 4 | 4 |
| Sporting | 1 | 1 |
The time of the incident or injury was recorded for 74 patients and, of these, every patient received TXA within 3 hours—only 25 (34%) patients received TXA within 1 hour of injury.
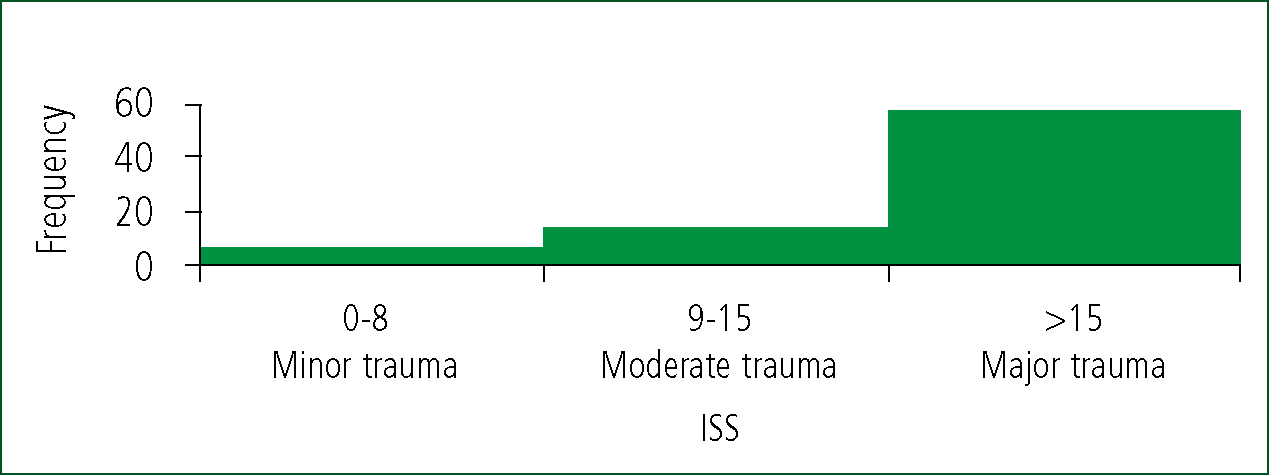
Retrospective ISS were available for 79 patients (range: 0–75; median: 26). There were 58 (73%) patients who had an ISS ≥15, which traditionally defines major trauma (Palmer 2007). ISS are shown in Figure 1.
PACS data were available for 95 patients; of these, seven (7.4%) were diagnosed with VTE; six (6.3%) with PE; and one (1.1%) with DVT. One of the patients with a PE was diagnosed 4 months after injury, but all others were within 1 month. Accounting for this, this evaluation shows a 6.3% incidence of VTE within 1 month. No patients died as a result of VTE.
In-hospital transfusion data were available for 99 patients. Of these, 45 (45%) had an in-hospital transfusion; and of these, 17 (38%) required more than four units of packed red cells.
Discussion
TXA has a proven survival benefit when given within 3 hours of injury, and the greatest benefit is seen when given within 1 hour. If it is delayed to more than 3 hours after injury, it is suggested that there is an increased risk of death (Roberts et al. 2011). Within this evaluation, no patients received TXA beyond 3 hours after injury. It is possible that there were factors which prevented administration within 1 hour, but this was not assessed within this evaluation. Despite the subjective indication for TXA, the majority of patients were retrospectively classified as major trauma by their ISS. This suggests that GNAAS were administering TXA in alignment with CRASH-2 (Shakur et al. 2010) in order to offer the known survival benefit.
VTE incidence post trauma has been quoted as ranging from 0.36% to 58% (Geerts et al. 1994; Knudson et al. 2004). While this range may be attributable to individual investigation sensitivity, the GNAAS-reported VTE incidence rate of 6.3% seems to fall towards the lower end of this range, and the lack of associated mortality is reassuring. While this is higher than the rate reported in CRASH-2, the authors of CRASH-2 do state that their frequency of VTE is likely to be under-reported (Shakur et al. 2010).
A third of patients who received TXA also required a pre-hospital transfusion of packed red cells. This reflects the more restrictive indication for pre-hospital transfusion compared with TXA. A slightly higher number of patients received an in-hospital transfusion (43%), which may be as a result of those patients with a more insidious presentation, or may be reactive to blood measurements within the hospital. This is less than the CRASH-2 transfusion rate of 50.4% in those patients who had received TXA (Shakur et al. 2010).
Limitations
There are inherent limitations of a retrospective PRF evaluation, including form availability and reliance on the accuracy of recorded information. In addition, follow-up data were not available for all patients, which may have altered the results presented here. Therefore, conclusions from the data collected should be treated with caution.
Only six children (age <18 years) received TXA within the study, and they were included as part of the overall analysis. Therefore, no specific conclusions should be made with regards to children on the basis of this evaluation alone.
Furthermore, owing to the subjective indication for TXA, it was not possible to assess whether there were patients who did not receive TXA when it should have been given.
Conclusions
Bleeding trauma patients can be offered a survival benefit with early administration of TXA. Within this cohort, TXA was administered promptly and appropriately, although not all within 1 hour. A VTE incidence of 6.3% seems in line with current literature regarding trauma patients. With zero mortality from VTE in this evaluation, this should be considered positively against the survival benefit of TXA.
GNAAS are now also able to offer thawed plasma to bleeding trauma patients, and this may further improve survival by reducing traumatic coagulopathy (Gonzalez et al. 2007). TXA is available to pre-hospital clinicians across the UK, where the author believes its use should be encouraged. A national review of TXA use may expand on the findings of this evaluation, and assess barriers to administration within 1 hour of injury. Further study, which evaluates whether there are major trauma patients who are not receiving TXA, may be appropriate in order identify a larger population who may benefit.

