In the UK approximately 60,000 people suffer a prehospital cardiac arrest each year, and in approximately 50% of cases resuscitation is commenced by the ambulance staff (Berdowski et al, 2010). Survival statistics for patients that receive resuscitation attempts remain critically low, ranging from 2 to 12%; this also reflects upon the variable success of resuscitation attempts across the many regions (Perkins and Cooke, 2012). The incidence of coronary artery disease is high in out of hospital cardiac arrest patients and incidences still remain high when the clinician's selection bias for primary percutaneous coronary intervention (PPCI) treatment is removed. In a case review of 72 consecutive patients who survived to hospital admission, coronary angiography findings showed that 63.9% of patients had coronary artery disease and 37.5% had findings consistent with an acute myocardial infarction (MI) (Anyfantakis et al, 2009). The variable survival rates shown by Perkins and Cooke (2012) cannot be explained solely by patient characteristics, implying that differences in hospital based care are at least partly responsible for this (Rea et al, 2010). The procedure currently used to treat myocardial infarction in the UK is Primary Percutaneous Coronary Intervention (PPCI), also known as angioplasty, and this service is accessed by UK ambulance staff via regional specialised centres located within 28 cardiac networks (McLenachan et al, 2012).
Current practice in the UK is moving towards a ‘direct to PPCI’ approach and is often dictated by local hospital policy. For example, in 2011 London Ambulance Service became the first UK ambulance service to initiate a direct to cath lab approach for resuscitated patients with ST-elevation on the ECG (Fothergill et al 2014). Outside London, in the South Central Ambulance Service area, for patients with return of spontaneous circulation (ROSC) and ST-segment elevation on the ECG the optimal care pathway requires direct transfer to a hospital that can provide immediate primary percutaneous coronary intervention (PPCI) at all times and local protocols should be followed to activate the PPCI pathway (Sherwood, 2016). A unified approach is recommended by the Resusciation Council Prehospital Guidelines (Deakin et al 2016; Neumar, 2008) which states that for post cardiac arrest, patients with ST-segment elevation on the ECG the optimal care pathway requires direct transfer to a hospital that can provide immediate primary percutaneous coronary intervention (PPCI) at all times. However it is common for coronary occlusion to present with no ST elevation, no LBBB, or a completely normal ROSC ECG, this less straightforward scenario requires individualised multidisciplinary input (Noc et al 2014; Roffi et al 2015). Conscious patients should undergo immediate angiography, whereas comatose patients should first be evaluated for non-cardiac conditions (Noc et al, 2014). However, some ambulance services are urging their clinicians to discuss these patients who have non-diagnostic ECGs with the cath lab, particularly when there is a history of preceeding chest pain (Sherwood, 2016). Decision making is not straightforward as the ROSC ECG is unreliable at predicting vessel occlusion, coronary occlusion may have been transient and coronary disease may cause arrest without occlusion, particularly in three vessel disease and left mainstem disease. There may also be indirect benefits of angiography which may help to guide management if the patient's coronary anatomy is known (MacCarthey, 2015).
Paramedic practice is always advancing and there are other treatments available other than transporting direct to a PPCI catheter laboratory. Numerous case studies published in the literature have shown critical care paramedics and physicians administering thrombolytic medications depending on the circumstances and patient characteristics. Case reports of out of hospital thrombolysis during cardiac arrest have led to hospital discharge and good neurological outcome in these published UK and Norweigian cases (Hitt and Pateman, 2015; Soreide, 2013). However, as case studies it is possible that these papers have been subjected to positive publication bias and although they clearly demonstrate thrombolysis as a feasible and effective treatment in these cases, it is known how many patients did not survive despite receiving the same care.
Patients suffering a cardiac arrest secondary to a myocardial infarction are high-risk patients and although they have a higher mortality rate, they also have the most to gain from aggressive specialist efforts at regionalised centres (Dalby and Whitbread, 2013). Unfortunately, it is difficult to determine a precipitating diagnosis for cardiac arrest in the emergency setting as there is often no medical history available, the patient is usually unconscious, and acute symptoms prior to cardiac arrest are reported in just 20 to 27% of patients with a confirmed MI (Anyfantakis et al 2009; Strote et al, 2012). Also, ST-segment deviation on the post arrest electrocardiogram (ECG) may be the consequence of transient repolarisation abnormalities after defibrillation, electrolyte abnormalities, or related to other causes (Anyfantakis et al, 2009) and figures between 57% (Reynolds et al, 2009) and 79% (Zannuttini et al, 2012) have been recorded in populations that have suffered an MI without ST-changes being present.
The aim and objective of this review is to make an evidence based judgement to determine if bypassing the local hospital to reach a specialist PPCI centre is beneficial to survival outcomes when the patient has been resuscitated from cardiac arrest. This is particularly relevant when it is difficult to assess the post-cardiac arrest patient for a myocardial infarction. Using the PICO template (Table 1), the following research question was developed as the basis for a literature search in order to scrutinise the best evidence based practice for these patients:
| Population | Pre-hospital cardiac arrest patients |
| Intervention | Transport to a PPCI centre |
| Comparison | [Standard treatment] |
| Outcome | Improved survival |
“Which resuscitated patients benefit from PPCI after an out of hospital cardiac arrest?”
Methods
In order to gather and critically review the known evidence to answer the research question it is important to obtain precise and relevant research material, therefore, the PICO template of database literature searching (Figure 1) was utilised to write the research question. This has been shown to increase the value of search results when compared to standard field searching in evidence based medicine (Aveyard, 2014; Schardt et al, 2007). An initial literature search was carried out of the healthcare database Medline which was chosen because of its vast size and relevance to the topic. Of note, the database holds articles on the all fields of medicine, nursing and allied health, but contains reference to journal articles only (Aveyard, 2014; NICE 2015).
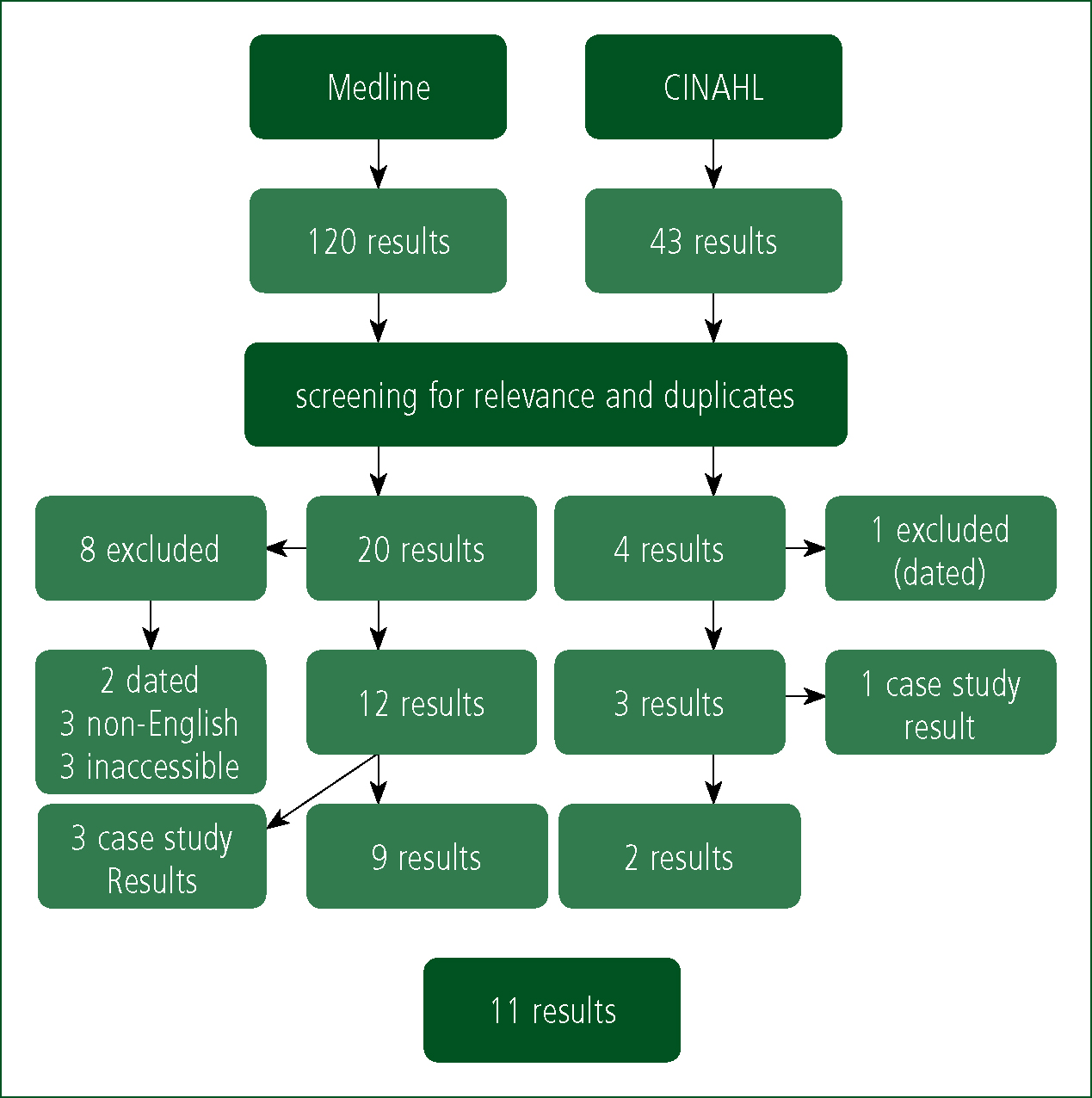
A second search was carried out using the same search criteria of the Cumulative Index to Nursing and Allied Health Literature (CINAHL) with the intention of finding further articles published under the more specific database of nursing and allied health literature, alongside any other literature outside of journal publications that are held by CINAHL (NICE, 2015). The searches were conducted using the three stage search strategy displayed in Figure 2. The Boolean operator ‘AND’ was used to link the search stages, with ‘OR’ being used to link terminology within each stage. The search strategy was designed to identify research associated with the following three keywords:
After the search results were recorded, the search of both Medline and CINAHL was repeated, but a number of amendments to the strategy were made. The term ‘paramedic*’ was truncated in the ‘out of hospital environment search stage, and the terms ‘cardiopulmonary resuscitation’ and ‘CPR’ were added to the ‘cardiac arrest’ search stage and were linked by the Boolean operator ‘OR’. However, these late additions did not find any further relevant or irrelevant results at all from either the Medline or from the CINAHL database. Searching the Cochrane Database of Systematic Reviews failed to find any papers of relevance to the research question. Therefore, for the purposes of this literature review and the results that it contains, the actual search strategy that yielded this paper's search results should be regarded as the original search shown in Table 2.
| paramedic OR ambulance OR pre-hospital OR prehospital OR out-of-hospital OR emergency medical service |
| AND |
| cardiac arrest OR resuscitation |
| AND |
| PPCI OR angioplasty OR cath lab OR catheterisation laboratory OR Primary Percutaneous Coronary Intervention OR heart attack centre |
Results
Searching Medline yielded an initial 120 results and an additional 43 results were gathered from CINAHL. Then, duplicate articles were removed and all results were screened for precise relevance to the question which left 20 and 4 results respectively (Figure 1). Full texts were accessed and read for articles where the relevance to the subject was initially questionable. To access the most contemporary knowledge, articles retrieved from both Medline and CINAHL published before 2005 were excluded and this led to the removal of just three dated results. As PPCI is a relatively new concept and as recently as 2009-2010 it became the dominant reperfusion management for myocardial infarction (McLenachan, 2012); it is believed that this can account for the contemporaneous search results. A further three results were excluded as they were not written in English, and three results were excluded because they were inaccessible. From both databases this left 15 results, of which four were case study reports. Overall, 11 results that are contemporary and relevant were found (Table 3), which will allow a thorough and accurate discussion of the research question in the next section.
Discussion
How does PPCI influence patient survival?
A vital aspect to proposing any new research question is to understand whether the intervention will benefit the patient or not, otherwise the proposal cannot be justifiable (RCEM, 2010). Two retrospective reviews conducted by Garot et al (2007) and Fothergill et al (2014) show a dramatic increase in survival to hospital discharge with the authors stating 55% and 66% survival respectively when patients have undergone PPCI to treat cardiac arrest due to MI. At the outset these statistics appear to be outstanding, but these are also highly selective. The percentages shown are taken from a population already having successful ROSC in the presence of a confirmed MI. Additionally, the official registry from which Garot et al (2007) acquired their statistics could not provide a specific number of out of hospital cardiac arrest patients for the duration of the study period. Instead a range of patients was provided (2500-3100) that received resuscitation from which 103 of 186 patients with confirmed MI survived to discharge. Using the median average (2800) from the range given, Garot et al (2007) has a survival to discharge that equates to 3.68%. Unfortunately there is no mention of pathology reports within the paper, so it is unknown how many patients did not survive that were later proven to have an MI. Garot et al (2007) is the oldest paper that will appear within this literature review with a population recruited between 1995 and 2005 and as such, its low survival rates may be subjected to distant resuscitation policies that have now been updated many times over. For instance, the ERC guidelines alone have been updated in 1998, 2000, 2005 and 2010 since the first recruitment for this study in 1995 (ERC, 2015).
Fothergill et al (2014) quotes a 66% survival to discharge rate for a cohort of 206 patients with MI and cardiac arrest transported to PPCI. This is particularly useful data when the authors compare this to a 12-32% survival rate for patients that were transported to the closest hospital by the same London Ambulance Service, researched one year previously (Fothergill et al, 2013). As the authors have cited another study published by themselves to show a leap in survival this could be susceptible to bias, however, there is a strong counter argument that they have accessed the most contemporary figures available which are not subject to population differences, differing ambulance service protocols, or other environmental confounding factors. Koeth et al (2012) is a complex multi-arm study comparing outcomes from out of hospital/hospital thrombolytic therapy versus PPCI versus no reperfusion therapy for 190 patients with cardiac arrest and MI. Although results are limited by a small population size of just 69 patients in the PPCI (54/69) vs no reperfusion therapy (15/69) arm, survival to discharge was 69.2% with PPCI, and 33.3% with no reperfusion therapy. This third retrospective review replicates the findings of Fothergill et al (2014).
Between 2003 and 2008, Dumas et al (2010) collected data from 714 patients that were referred to a tertiary centre specialising in cardiac arrest, where the treatment offered includes PPCI, therapeutic hypothermia and intensive care unit admission 24 hours a day, 7 days a week. Provided patients did not have an obvious extra-cardiac cause for their arrest, they were admitted directly to the catheterisation laboratory for a coronary angiogram with a view to proceeding to PPCI if coronary occlusion was detected. Dumas et al (2010) states a survival to discharge rate of 39% for all patients, but notably this increased from 31% for no or failed PPCI to 51% for successful PPCI. However, the authors acknowledge that their sample population is likely to be highly selective due to a very high incidence of patients that presented with ventricular fibrillation/tachycardia (VF/VT) as an initial rhythm. Although, 39% were excluded due to extra-cardiac causes and patients presented with non-VF/VT rhythms in 71% of cases. The Parisian out of hospital care system described in the paper includes a physician presence at every cardiac arrest with strong cessation of resuscitation guidelines which may also have contributed to the low non-VF/VT statistics described. Nonetheless, Dumas et al (2010) displays a significant decrease in mortality (odds ratio 2.06) for all patients when PPCI is successful.
Dumas et al (2012) retrospectively assesses the impact of PPCI when combined with therapeutic hypothermia on long term survival following out of hospital cardiac arrest. In a population of 5958 patients with 1001 surviving to discharge, 791 discharged patients had a cardiac aetiology, of which 384 received PPCI. The study used both PPCI and therapeutic hypothermia groups which were then analysed for trends with or without each intervention. The data in Table 4 shows a 5 year increase in survival from 49.2% to 76.5% when comparing ‘nil research interventions’ versus PPCI; notably PPCI was (4.4%) greater than therapeutic hypothermia alone. Another study also reflects this finding (Grasner et al, 2011) with PPCI improving survival, but whilst therapeutic hypothermia also showed improved survival odds, it did not reach statistical significance. Again, Dumas et al (2012) used a selective population with a high percentage of VF as the initial rhythm and there was also a high incidence of cardiac aetiology preceding arrest (79.1%). Several studies within this search are subject to a degree of selection bias as randomisation cannot occur retrospectively (Strote et al, 2012; Nanjayya and Nayyar, 2012; Zannuttini et al, 2012) and so the decision to refer for PPCI was taken by the cardiologist. However, this remains useful data as Zannuttini et al (2012) shows that in patients referred for PPCI, a coronary occlusion was detected in 52% of patients and in those that received delayed PPCI an occlusion was detected in 33% of patients. As such, in this study clinical judgement can detect the need for emergency PPCI with a sensitivity of 0.43. Of course, this should be interpreted with caution as decision making may be influenced by other factors such as prioritising other treatments over PPCI.
| Intervention | 1 year survival % | 5 year survival % |
|---|---|---|
| PPCI & TH | 100 | 88.6 |
| PPCI | 90.6 | 76.5 |
| TH | 81.1 | 72.1 |
| nil research intervention | 71.8 | 49.2 |
The presenting cardiac arrest rhythm
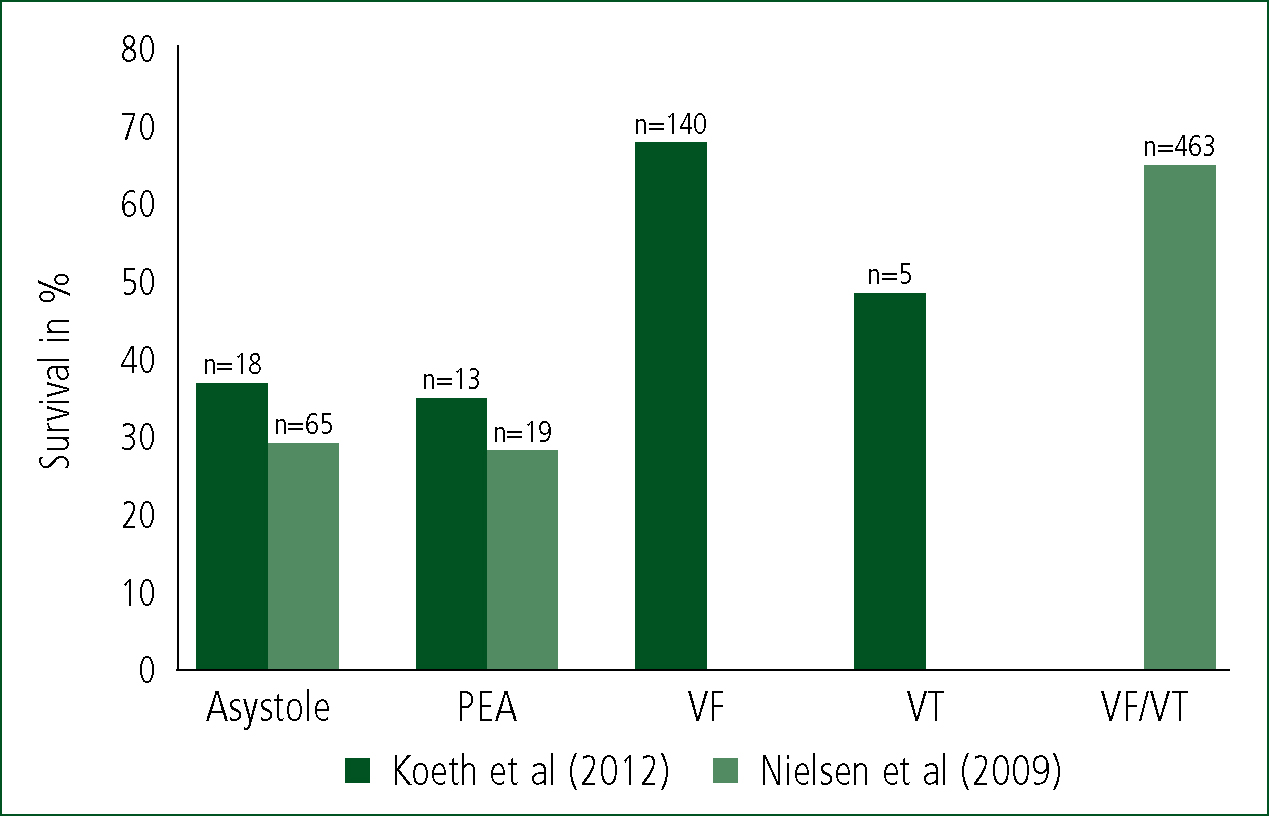
As Noc et al (2014) and Roffi et al (2015) have aforementioned, the ROSC ECG of a patient with coronary occlusion can include no ST elevation, no LBBB, or a completely normal ROSC ECG. Although defibrillation and electrolyte abnormalities can cause ST elevation (Anyfantakis et al, 2009), patients that have a clear STEMI on their ROSC ECG should have PPCI performed as soon as possible, a practice that the UK Resuscitation Council advocates (Deakin et al 2015). It is the patient with a no ST elevation, no LBBB, or a normal ECG that will present the clinician with a dilemma as to the best way forward. This decision can be affected by patient characteristics and the availability of interventions, but other factors such as ECG activity shown during the cardiac arrest also predict survival and a cardiac cause for the arrest. The findings of Nielsen et al (2009) above concur with several other studies, where patients with initial cardiac arrest rhythms of VF/VT have shown increased chances of survival. The authors of one Scandinavian study prospectively researched the outcomes and adverse events during therapeutic hypothermia after cardiac arrest (Nielsen et al, 2009). From a total of 986 patients, 70% (n=686) had a VF/VT arrest, 49% (n=479) of all patients underwent angiography and 303 received PPCI. 61% of all survivors came from the VF/VT population. However, although the VF/VT group have demonstrated good rates of survival, there can also be a degree of optimism for patients presenting with asystole (n=217).
Although the asystole group is statistically less powered than the VF/VT group, 30% survived to discharge, with 22% having a favourable neurological outcome. This is a positive step forward as patients from the asystole group (25% survived) have now been shown to have a prognosis similar to patients in pulseless electrical activity (27%), however this is a weak powered study with only 19 (PEA) and 65 (asystole) patients in their respective arms. Historically, asystole has been known to predict the worst outcomes in the absence of these trial interventions (Perkins and Cooke, 2012). It must be remembered that as Nielsen et al (2009) aims to assess therapeutic hypothermia as an intervention, this may also partly explain these high asystole survival rates and therefore the results should not be attributed to PPCI alone. Koeth et al (2012) also has findings that agree with Nielsen et al (2009), however, this is also significantly underpowered in the PEA and asystole groups although survival rates are similar between studies (Figure 2). This appears to be a common problem in cardiac arrest research as so few patients achieve ROSC when they present with asystole (Perkins and Cooke, 2012). A further limitation is how Nielsen et al (2009) have combined the VF/VT groups in their study but this does not appear to detract from the pattern seen in the data regarding prognosis, particularly when the VT group in Koeth et al (2012) only consists of 5 patients.
On the outset, the ECG appears to act as a prognostic indicator, although it clearly does not hold sufficient specificity or sensitivity to justify applying or withholding the intervention solely based on the initial ECG. There is a significant proportion of patients with PEA and asystole that have suffered an MI which although have shown a reduced survival rate, efforts are by no means futile. Grasner et al (2011) present the patient population arranged by ECG rhythm and cardiac versus non-cardiac cause of arrest. The findings (Figure 3) demonstrate several key points. Firstly, in cardiac patients there is an almost equal selection of both VF (n=226) and non-VF rhythms (n=240) whilst in non-cardiac patients VF is rare. However, the high prevalence of cardiac causes compared to non-cardiac causes has led to the non-cardiac group to be lesser powered in this study, although there is a clear rationale to suggest that VF is a strong predictor of cardiac cause.
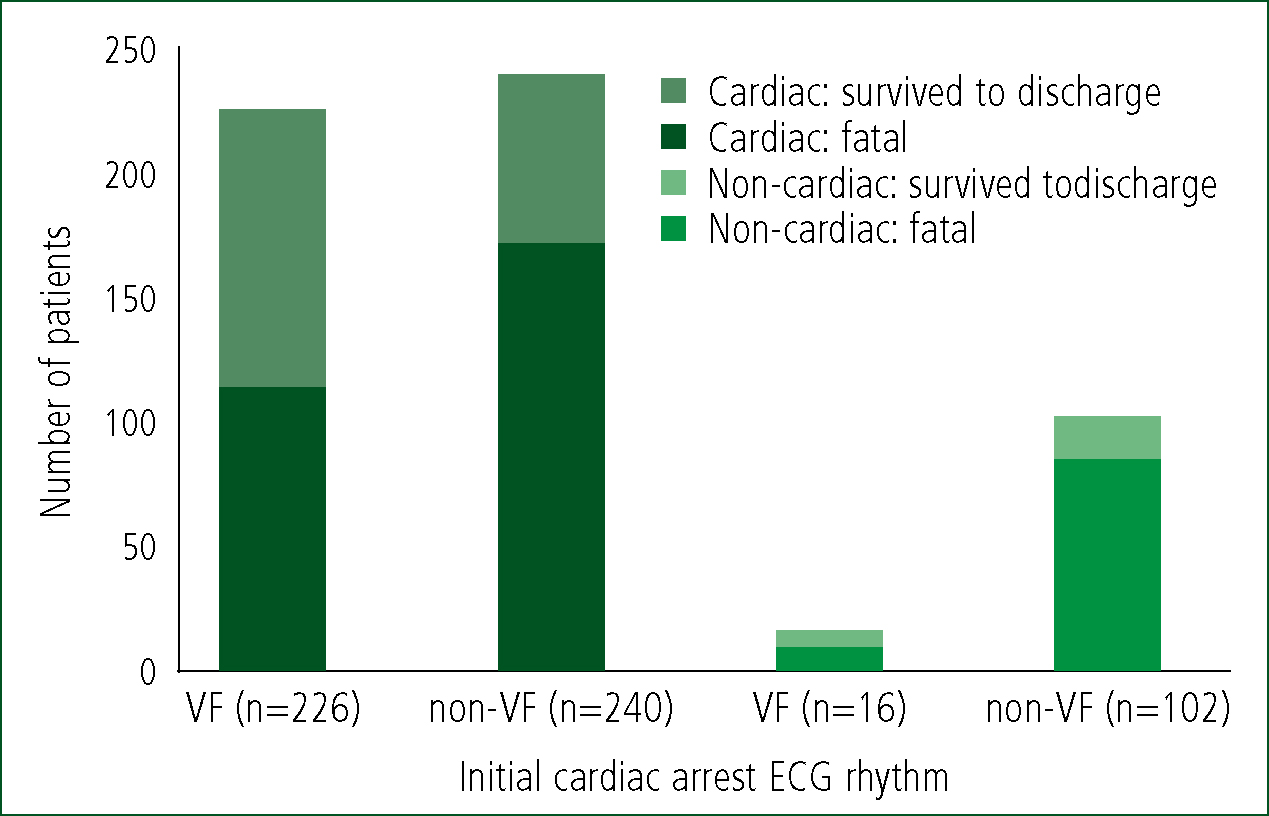
Secondly, non-VF rhythms from any cause of cardiac arrest leads to a poorer chance of survival than VF from any cause. VF, by either cause, has a survival rate of approximately 50% although the non-cardiac VF group is significantly underpowered to accurately determine this. Frustratingly, the rhythm VT has been unaccounted for in Grasner et al (2011), although this omission would be unlikely to alter the findings meaningfully as another study (Koeth et al, 2012) has shown that VT is a very rare event in cardiac arrest, occurring in just 2.8% of patients with MI. The authors have also chosen to present the initial rhythm data of PEA and asystole as a non-VF rhythm group, which prevents further data analysis of rhythm.
Implementing PPCI for arrested patients
The success of implementing a new intervention is affected by barriers which may prevent or impede successful change (NICE, 2007). This will be the final theme identified from this literature search. One barrier identified is the safety of the critically ill patient during extended transport times to reach a regional PPCI capable hospital. This scenario is similar to the implementation of the UK National Major Trauma Network. Although specifics are obviously different, the proposal is essentially the same dilemma. That is, whether patients should be transported to a place where they have more to gain, but weighted against a risk of mortality in transit and an extended distance and time to hospital.
The Trauma Audit and Research Network (2013) reported a 20% increase in survival from major traumatic injuries since regionalisation, proving the benefit of specialist centres over the more minor detriment caused by prolonged transportation. Some authors have stated that patient outcomes are likely to be positive and comparable between trauma and cardiac arrest (Kajino et al, 2010). However, following the literature search performed here, there is an absence of any research that has examined the direct impact of transporting a patient an extended distance to reach definitive care; although constructing such a trial would be unlikely to progress beyond an ethics committee. Therefore, other relevant evidence must be considered to assess whether extending the transport time to reach a PPCI centre can be justified.
It would appear that whilst MI and cardiac arrest are both immediately life threatening conditions requiring emergency treatment, the speed at which coronary reperfusion is delivered is not as emergent as one might think, with patients still benefitting from PPCI at 6 hours post cardiac arrest. One retrospective control study (Strote et al, 2012) assessed how survival would be affected by a delay in receiving the intervention. Survival was greater in the acute (<6-hours, 72%) versus the delayed (>6 hours, 49%) study arm. However, in the absence of a ‘no PPCI’ patient group it is unknown from this study alone exactly how much benefit was derived from PPCI performed >6 hours post cardiac arrest compared to no PPCI. The use of this paper's +/- 6 hours controlling factor makes Strote et al (2012) one of the highest quality studies identified within the database searches undertaken here according to the Centre for Evidence-based Medicine (2009) hierarchy of evidence (Table 5). As a retrospective study using control, the decision to treat a patient with acute or delayed PPCI was left to the physicians treating the patient at that time, which triggered a degree of selection bias. This can be seen in the characteristics of the acute patients as they were on average 3 years younger, more often male, smokers, and had more cardiac conditions previously diagnosed. As PPCI centres in the UK are strategically located within 2 hours of each other and with 86% of call to balloon times being less than 2.5 hours (British Cardiovascular Intervention Society, 2012), this is firmly within the proposed 6 hour treatment window suggested by Strote et al (2012). It could therefore be suggested that extending transportation time, may be in the patient's interests if they are then able to access PPCI.
|
Level 1.Systematic reviews (SR) of randomised controlled trials (RCTs) and RCTs
|
|
Level 2. SRs of cohort studies and cohort studies
|
|
Level 3. SRs of case-control studies and case-control studies
|
|
Level 4. Case series
|
|
Level 5. Expert opinion and studies including in-hospital arrested populations
|
Another potential barrier to the intervention is whether successful PPCI will be a useful procedure when carried out on post-cardiac arrest patients that are in a comatose neurological state. Nanjayya and Nayyar (2012) write that such a strategy may not be useful when prognosis is determined by the level of neurological injury suffered at the time of cardiac arrest. However, their study may be prone to selection bias as the decision to refer patients for immediate PPCI was made by the cardiologist on-call, which created non-randomised intervention and control groups.
| Author and Date | Study setting | Patient group | Study type | Results | Limitations |
|---|---|---|---|---|---|
| Dumas et al (2010) | France | 435 patients with ROSC who received PPCI when no obvious extra-cardiac cause was identified | Prospective registry case series | 96% of patients with ST elevation had >1 coronary lesion. 58% of patients with non-diagnostic ECG had >1 coronary lesion. Overall survival was 40% | Selective population, high rates of VF |
| Dumas et al (2012) | Seattle, USA and Paris, France | 5958 out of hospital cardiac arrests. 1001 patients survived to discharge, 384 received PPCI | Retrospective case series | Survival at 5 years 78.7% for patients receiving PPCI. 54.4% for patients not receiving PPCI | Selection bias, high rates of VF. No information on follow up period quality of life. |
| Fothergill et al (2014) | London, England | 206 adults with ST elevation on ROSC ECG conveyed to PPCI capable hospital | Retrospective descriptive review | 66% survived to discharge, 97% alive at 1 year | Unknown how many patients had PPCI after being transported - due to data collection. Unknown neurology at discharge |
| Garot et al (2007) | 4 hospitals in Paris, 1 in Normandy, France | Total of 186 arrested patients: 154 out of hospital, 32 in hospital | Retrospective observational case series | 54% survival at 6 months | Dated with population recruitment occurring between 1995 and 2005. Selection bias. Included in hospital cardiac arrests |
| Grasner et al (2011) | Germany | 2973 arrested patients, 1302 had ROSC. 26% received PPCI and 74% did not. | Prospective registry case series | Survival at 24 hours 89% for patients receiving PPCI. 61% for patients not receiving PPCI | Data drawn from a register which is thought to not represent the entirety of the picture across Germany. Highly selective cohort bias |
| Koeth et al (2012) | Germany | 79 arrested patients with STEMI who arrived at hospital with ROSC. 54 received PPCI, 15 received no reperfusion therapy, 10 received thrombolysis | Retrospective observational case series | Survival rates for each treatment group are: PPCI 69%, no reperfusion therapy 33%, in hospital thrombolysis 70% | Data drawn from a myocardial infarction registry therefore smaller population numbers. Out of hospital thrombolysis was not an independent predictor of survival |
| Nanjayyar & Nayyar (2012) | New South Wales, Australia | 70 arrested patients. 35 received PPCI. 35 did not. All were admitted alive to intensive care | Retrospective observational case series | Survival to discharge 40% for patients receiving PPCI. 31% for patients not receiving PPCI | Small population study. Decision to proceed to PPCI was taken by the cardiologist and was not randomised |
| Nielsen et al (2009) | Lund, Sweeden | 986 patients survived to intensive care following out of hospital cardiac arrest. 49% received angiography and 30% received PPCI | Prospective observational case series | Survival 63% for patients receiving angiography. 66% for patients receiving PPCI | Data drawn from a Therapeutic Hypothermia Network (cardiac arrest) Registry with less cardiology detail than would be found in a cardiology paper |
| Strote et al (2012) | Seattle, USA | 240 patients with ROSC from VF/VT cardiac arrest. 61 received PPCI acutely < 6 hours, 179 were deferred to >6 hours. | Retrospective systematic review case series | Survival 72% for <6 hours and 49% >6 hours | Reliant on medical chart review. Has attempted to minimise biases based on statistical adjustment. Selective population, VF/VT (initial rhythm) only |
| Wolfrum et al (2008) | Schleswig-Holstein, Germany | 33 patients with ROSC after VF arrest and STEMI. All received PPCI | Retrospective observational case series | Overall survival at 6 months was 30%. Survival was 25% when receiving therapeutic hypothermia, 35% in the control group | This is primarily a very small study of therapeutic hypothermia, 16 patients received cooling and 17 did not |
| Zannuttini et al (2012) | Udine, Italy | 93 patients with ROSC following out of hospital cardiac arrest. 66 received PPCI | Retrospective case series | Survival 54% for patients receiving acute PPCI. 47% for delayed or no PPCI. | Rates of successful PPCI were low compared to other studies at 52% |
Nanjayya and Nayyar (2012) conclude that PPCI for comatose survivors of cardiac arrest is associated with a longer stay in intensive care and hospital, more interventions and potentially more use of resources, whilst 38 out of 40 deaths were due to poor neurological recovery. The authors acknowledge a trend in results towards increased survival, but this may be biased as the patients with a lower severity of illness at admission were predominantly patients with an MI rather than with other pathologies. It must be noted that other studies contradict these findings (Zannuttini et al, 2012) by showing benefits to comatose patients. This may be due to the timing of PPCI because whilst the call to PPCI times are a median of 2.5 hours in Nanjayya and Nayyar (2012), Zannuttini et al (2012) does not state a specific time period, but instead states that PPCI is performed as an emergency which could indicate that the timing may be more urgent here.
Wolfrum et al (2008) shows potential value in combining PPCI with therapeutic hypothermia to overcome poor neurological recovery. It is a small study of 33 comatose patients from a VF cardiac arrest and an MI who received PPCI, from which 16 also received therapeutic hypothermia. Patients that received therapeutic hypothermia had a lower mortality (25%) at 6 months than those that did not (35%). The study uses a cohort selection of only VF arrested patients who have a more optimistic survival rate than other rhythms (Figure 3) and this is also seen in Grasner et al (2011). The key finding of Wolfrum et al (2008) is that PPCI can be combined with therapeutic hypothermia safely, albeit there were increased bleeding complications with significantly more patients receiving blood transfusions when combining both interventions. No bleeding was life threatening and bleeding sites were mainly located at the arterial puncture site or involved nasal bleeding after nasogastric tube insertion.
Conclusions
The research demonstrates significantly increased survival rates when PPCI is available for patients with an ST elevation MI complicated by cardiac arrest. Studies consistently agree with this in their findings as does guidance from the UK Resuscitation Council and the International Liason Committee on Resuscitation (Deakin et al, 2015; Neumar, 2008). In patients with non-diagostic ECGs and ROSC, the evidence is less clear but the decision to proceed to PPCI should be largely based on risk factors and predictors of acute coronary syndrome identified during cardiac arrest. There is a high incidence of IHD in adult cardiac arrest patients.
When a cardiac arrest is assessed as non-cardiac by senior medical staff, this is frequently not the case and culprit occlusions are then found during angiography. Predictors of cardiac aetiology include an initial rhythm of VF due to its rarity in patients with non-cardiac causes. Asystolic and PEA arrest rhythms must not be used to predict a cause as these rhythms occur almost as equally as VF following an MI. VT is very rare in all causes of cardiac arrest.
Considering how the ECG rhythm may predict survival, two studies reported good rates of survival for VF, with results showing almost equal odds between PEA and asystole. However, studies comparing survival rates between patients grouped by initial ECG rhythm are often underpowered in the asystole group due to few patients with this rhythm achieving ROSC. When asystolic patients do have ROSC they have considerably higher chances of survival than of their counterpart asystolic patients who had arrested from a non-cardiac etiologies.
At present, work on developing an evidence based clinical decision rule to guide the decision to transport a patient directly to PPCI following cardiac arrest would be restricted by the lack of a high quality RCT answering the question until now. Patterson et al (2017) have recently conducted a pilot study demonstrating the ability to conduct a large scale RCT, namely the ‘ARREST trial’, to study this treatment as a randomised intervention. Mortality rates were representative of VF arrested patients and comparable to previous statistics in the same London Ambulance Service (Fothergill et al, 2013).
The risks of extending the journey time to reach a specialised centre appear to be outweighed by the considerable benefits of accessing PPCI facilities in patients with STEMI, or a non-diagnostic ECG in conjunction with specific predictors and risk factors. PPCI should be considered an emergency intervention for all arrested patients and should be delivered with even greater haste in comatose survivors of cardiac arrest.
