In recent years, the increased demand for ambulance services has drawn attention to the phenomenon of frequent callers who, although making up a small subset of service users, account for a disproportionately high volume of calls (Scott et al, 2014a; 2023; Aslam et al, 2022).
Frequent callers often request ambulance services for non-emergency reasons, resulting in increased costs, reduced availability of ambulances for other people and, therefore, a lower quality of care for those needing emergency care (Snooks et al, 2019). The consequences of frequent callers highlight the importance of effective strategies that can be introduced to reduce such calls.
The definition of frequent callers to ambulance services has previously varied across the evidence base (Smith and McNally, 2014; Edwards et al, 2015). Variability in definitions can significantly impact research findings and real-world applications (Middleton et al, 2014; Scott et al, 2023). Therefore, the Frequent Caller National Network (FreCaNN), established in 2013, defined a frequent caller as one who generates five or more calls in 1 month or 12 calls in a 3-month period (FreCaNN, 2022). Although this definition has been criticised for limiting the definition to those who call themselves and omitting other calls (Harring et al, 2024), the FreCaNN definition aims to provide consistency to help healthcare services share best practice and inform local and national policy on the standardised management of frequent ambulance callers.
Ambulance service frequent callers are a substantial problem for healthcare systems such as the NHS, as they reportedly strain resources and may negatively impact the quality of care for other people (Snooks et al, 2019). Because of this, such callers can experience stigmatisation and a lack of understanding of their circumstances from health professionals (Stangl et al, 2019; Snowdon, 2022; Evans et al, 2024). Frequent callers often have interconnected complex physical, mental and social needs that bring them into contact with ambulance services (Snowdon, 2022).
Various strategies have been developed and implemented to reduce the impact of frequent callers, such as case management (Snooks et al, 2019), mass distribution letters (McDonnell et al, 2022), levelled intervention management systems (Smith and McNally, 2014) and outreach teams in the United States (Tangherlini et al, 2016).
Analysing the strategies employed to manage this population and evaluating their effectiveness could inform and instigate policy and practice updates. Snooks et al's (2019) review of UK ambulance trusts highlighted that established reduction strategies are limited, thus highlighting a gap in the evidence base.
Aim
This literature review aimed to analyse primary research articles that explore strategies to reduce frequent ambulance callers and evaluate their effectiveness in terms of reducing call volume to help alleviate the pressures on ambulance services and improve caller outcomes.
By providing an overview of the current knowledge base and identifying the most effective interventions, this review will contribute to a better understanding of the most promising approaches for managing this complex issue and offer recommendations for future research and practice.
Research design and methods
Search strategy
An integrative review was undertaken, using a systematic method and thorough search strategy including studies with diverse methodologies to enable a comprehensive overview of the literature and understanding of the topic area (Noble and Smith, 2018).
The search was completed in September 2024. Databases searched included MEDLINE with full text, Academic Search Complete, AMED (Allied and Complementary Medicine Database), APA PsycArticles, APA PsycInfo and CINAHL Ultimate. They were chosen as they are the most relevant comprehensive health-focused databases and provide access to a wide range of articles related to nursing, paramedicine, allied health, biomedicine and healthcare (Alving et al, 2018). Google Scholar and connected papers were additionally used to conduct snowballing.
Alternative search terms were used to ensure robustness of the search strategy (Table 1). Boolean operators were used in a systematic manner to develop a search strategy that began with a broad scope and gradually became more targeted. The search incorporated the use of OR to connect terms or phrases, ensuring that at least one of them would be present in the search results. To search for multiple terms or phrases simultaneously, AND was used as a connector. The asterisk (*) served as a wildcard symbol, allowing for a range of variations of the search term or phrase. Lastly, quotation marks (“”) were used to search for an exact phrase instead of individual words within it.
| Population 1 | AND |
AND |
AND |
|---|---|---|---|
| Frequent callers |
Ambulance services |
Strategies |
Reduce the volume |
| “frequent caller*” |
“ambulance service*” |
“strategy*” |
“effectiveness” |
Various terms to describe ‘frequent caller’ were included to ensure that all relevant research was captured, as different terms are used. ‘Frequent attenders’ or ‘frequent users’ were included to ensure that no appropriate articles were missed; however, these terms are used to identify those who may frequently attend emergency departments but may not have contact with ambulance services – the focus of this review.
Peer-reviewed primary research was included, defined as research reviewed by peers through journals' academic peer-review processes (Willis, 2024). This is a limiter on the EBSCO database.
Primary studies conducted in the UK were chosen as healthcare services differ across the globe (Elston et al, 2022). The 2014–2024 time range was chosen to ensure that evidence was current; in addition, FreCaNN was established in 2013.
Full review was undertaken of any key papers included in relevant reviews and any primary studies meeting the search strategy were reviewed for inclusion (Alruwaili et al, 2024).
Other reviews have focused on frequent attenders to emergency departments (Kumar and Klein, 2013; Soril et al, 2015; Hudon et al, 2016; Moe et al, 2017; Memedovich et al, 2024), not specifically focused on ambulance callers.
There is a planned Cochrane review of case management or planning for frequent attenders at emergency departments, rather than callers to ambulance services; it will exclude any non-randomised trials or studies without a comparison control group (Budhwani et al, 2022).
Therefore, there is a gap in the evidence base and a need for the present review. This review considers all interventions and all methodologies focused on all ambulance callers rather than specific groups such as people with mental health issues (Stergiopoulos et al, 2016; 2017; Gabet et al, 2023) or homelessness (Smith and Moyer, 2021).
Results
Database search outcome
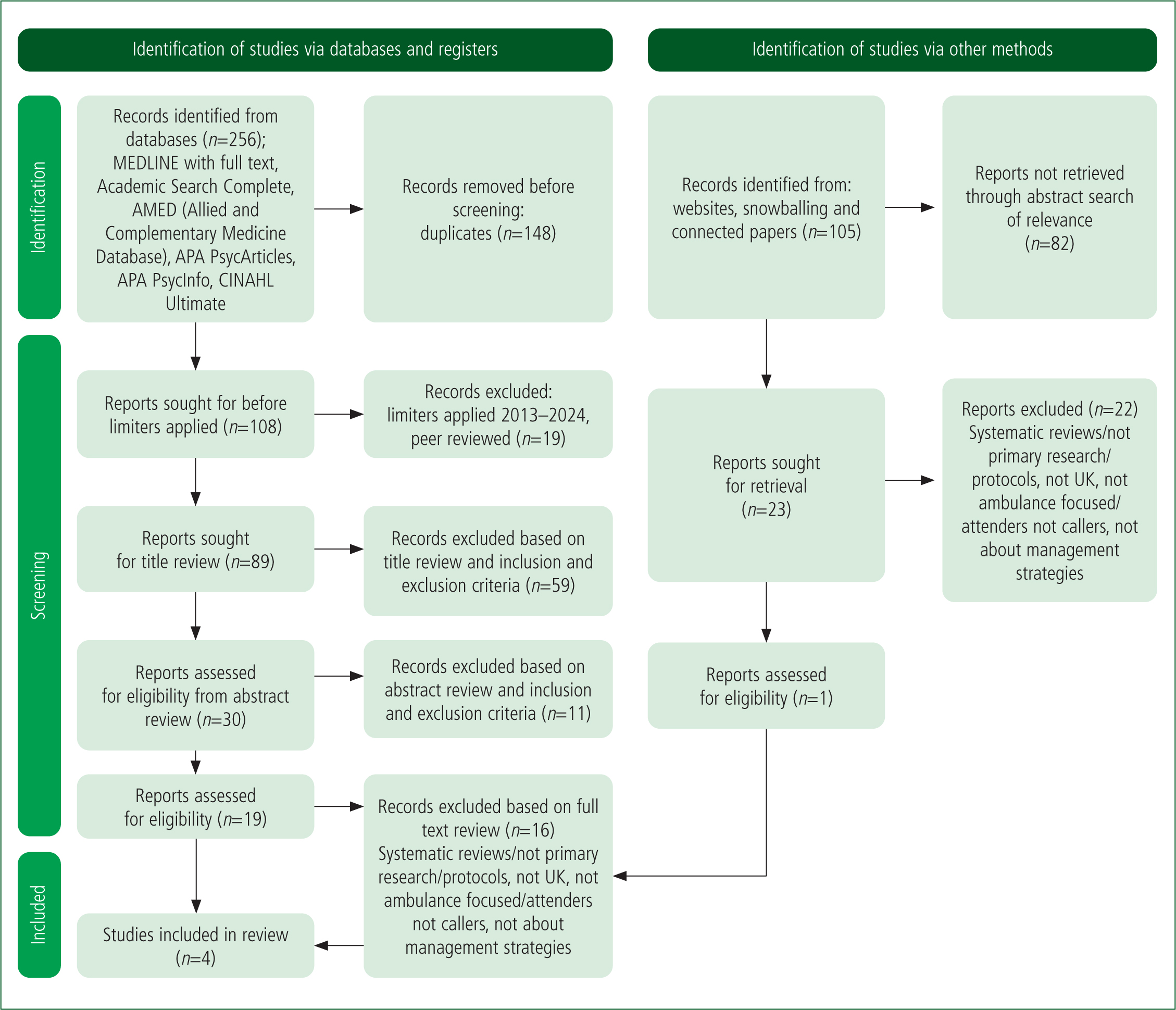
Upon completing the database search using the key terms (Table 1) and following the removal of duplicates, 256 pieces of evidence were identified for screening. Through further reduction from reviewing titles and abstracts and relevance to the research question using inclusion and exclusion criteria outlined in Table 2, three articles were identified from the database search. Snowballing was used to search for related literature and 105 items were identified, of which was one included (Snooks et al, 2019). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) approach was completed (Page et al, 2021) (Figure 1). The four papers identified for review were Smith and McNally (2014), Edwards et al (2015), McDonnell et al (2022) and Snooks et al (2019).
| Inclusion | Exclusion |
|---|---|
| 2014–2024 | Not children (age 0–18 years) |
| UK | Countries other than UK |
| Full text | Focus on emergency services other than ambulance services, including frequent attenders at emergency departments who may have had no contact with ambulance services |
| Written in English | Not frequent callers |
| Adults aged ≥18 | Not focused on strategies |
| Focused on ambulance services | Not peer reviewed |
| Focused on frequent callers | Focus only on one patient group e.g. mental health, homelessness, chronic illness |
| Focused on management strategies | |
| Peer-reviewed primary research |
Critical appraisal
To appraise the four articles found through the search strategy, the relevant Critical Appraisal Skills Programmes (CASP) tools were used. The CASP qualitative checklist (2024a) was used for Snooks et al (2019). There is no CASP tool specifically for service evaluation. However, as this study is based on an open national survey, this was the most appropriate tool.
The other three articles were cohort studies without a comparator, so the CASP cohort study tool (2024b) was used for these. The studies reviewed are outlined in (Table 3).
| Authors and year | Aim/objective | Methodology | Sample size | Key findings implications/recommendations | Strengths | Limitations |
|---|---|---|---|---|---|---|
| Smith and McNally (2014) | To evaluate the early results of a frequent caller management system | Pilot prospective cohort study without a comparator | 624 callers |
|
|
Limited generalisability |
| Edwards et al (2015) | To profile frequent callers and evaluate the impact of case management on their use of ambulance services | Retrospective cohort study without a comparator | 110 callers |
|
|
Limited generalisability |
| Snooks et al (2019) | To investigate the strategies employed by ambulance services in the UK to address the needs of frequent callers | Service evaluation using a national survey | 13 ambulance services |
|
|
Response rate |
| McDonnell et al (2022) | To assess the effectiveness of mass distribution letters as early interventions for potential frequent callers | Cohort study without a comparator | 96 callers |
|
|
Review of single intervention strategy |
Discussion
Three main themes emerged concerning frequent users of ambulance services and strategies to reduce calls as follows:
Identifying frequent callers and understanding their needs
It is important to identify frequent ambulance callers and understand the reasons behind their high use in order to implement effective strategies. By profiling these individuals, ambulance services can better recognise their unique needs, use resources effectively and develop tailored interventions (Kwame and Petrucka, 2021).
FreCaNN (2022) in the UK provides a definition of what constitutes a frequent caller as someone who makes five calls in 1 month and 12 in 3 months. This definition was used in Smith and McNally's (2014) frequent-caller management system and, as identified by Snooks et al's (2019) review of UK ambulance service frequent-caller strategies; most UK ambulance services use this nationally agreed definition.
However, before FreCaNN was established, ambulance services – such as the London Ambulance Service in Edwards et al's (2015) retrospective study completed before 2012 – defined a frequent caller as an individual who called the ambulance service 10 times per month for 3 months and/or where the quantity of calls was considered to have a significant impact on resources.
McDonnell et al (2022) initially identified potential frequent callers as those calling three times in a month, two times fewer than the FreCaNN; as the focus was on potential frequent callers, they were then monitored over 10 weeks.
A clear, consistent definition supports robust analysis of large amounts of data across various demographics to ensure reliable reporting and subsequent management of frequent callers (Smith and McNally, 2014), in addition to assessing the effectiveness of intervention strategies (Snooks et al, 2019). The implementation of FreCaNN's (2022) defining criteria should benefit future identification and the process of assessing caller needs to help reduce call volumes.
The papers reviewed here outlined methods to identify frequent callers. Most relied on analysing call data and caller demographics to identify frequent callers. Smith and McNally (2014) used an automated computerised report and McDonnell et al (2022) also used a computer system. As by Snooks et al (2019) found, most UK ambulance services have electronic systems that flag potential frequent callers and subsequent calls are then identified. Edwards et al (2015) identified frequent callers through practitioner referrals and call data as reviewed by a specialist team.
Smith and McNally (2014) emphasised the importance of data-driven systems for identifying frequent callers and addressing their needs through personalised, targeted interventions and support, which are essential for addressing the unique needs of frequent callers (Scott et al, 2014b; 2023). A study by Elston et al (2022) that explored frequent attenders at emergency departments used a predictive artificial intelligence (AI) algorithm to identify frequent attenders – a further option for future research around frequent callers.
Having a definition of frequent callers can ensure reliable reporting and management. There are different methods for identifying frequent callers, through computer systems, practitioner referral or specialist review. Nevertheless, however frequent callers were defined and subsequently identified, all included articles emphasise the importance of robust implementation of interventions to manage pressures on ambulance services and improve caller care.
Implementing interventions for frequent callers
Various interventions and strategies are intended to reduce the number of calls from frequent ambulance callers. Snooks et al (2019) explored the policies and management systems implemented by UK ambulance services; Smith and McNally (2014), Edwards et al (2015) and McDonnell et al (2022) focused on the interventions themselves. These interventions include case management (Edwards et al, 2015), mass-distribution letters (McDonnell et al, 2022) and frequent-caller management systems (Smith and McNally, 2014). Targeted interventions need to be implemented to manage the demand for emergency services and improve caller outcomes.
Edwards et al's (2015) study offers valuable insight into the potential benefits of case management for frequent callers, emphasising the importance of caller profiling and a multidisciplinary approach. It contributes to the development of targeted interventions aimed at reducing demand for emergency care and improving caller outcomes. Aslam et al's (2022) protocol outlines a planned large study to evaluate case management for frequent ambulance callers in the UK to add to the evidence for this approach. Case management has been found to be effective for frequent attenders in emergency departments (Hudon et al, 2017; Grazioli et al, 2019; Elston et al, 2022), hence the planned Cochrane review (Budhwani et al, 2022).
McDonnell et al (2022) reviewed mass-distribution letters as an effective strategy to reduce frequent callers. However, frequent callers have a broad spectrum of reasons for calling, ranging from comorbidities, loneliness (Moseley et al, 2024), mental health (Gabet et al, 2023), and mobility problems (Agarwal et al, 2019; Aslam et al, 2022; Scott et al, 2023). This highlights the need for person-centred approaches to manage frequent callers effectively, rather than adopting a standardised approach for all frequent callers. There has been some effectiveness of person-centred approaches like assertive outreach for alcohol-related emergency department attendance (Blackwood et al, 2020; Mak et al, 2022). Case management and care plan interventions for frequent attenders with mental health problems have also been successful (Gabet et al, 2023).
The outcome of McDonnell et al's (2022) mass-distribution letter appears to have reduced call volume, which may be owing to various factors, but there may be unintended consequences that put some callers at risk. After receiving the letter, some might hesitate to call an ambulance in an emergency for fear of being labelled as a frequent caller, potentially leading to negative health outcomes (Skogevall et al, 2022). The mass-distribution letter does, however, inform frequent callers of available and appropriate services that they can access instead, educating them on what they should be using instead of ambulance services.
There is also a risk that callers who receive letters may feel stigmatised or singled out, which could have negative psychological effects (Stangl et al, 2019; Snowdon, 2022). However, the mass-distribution method used by McDonnell et al (2022) may minimise the risk of stigmatisation as callers may be less likely to feel personally targeted if they are aware of the criteria for people receiving the letter.
While the mass-distribution letter approach may be cost-effective, it is not as tailored to individual needs as case management or caller management systems. Edwards et al (2015) highlight the importance of tailoring interventions to the specific needs of individual callers to better address their diverse needs and improve caller outcomes. However, this is more expensive and time consuming than McDonnell et al's (2022) approach.
Smith and McNally (2014) found that implementation of a frequent-caller management system can lead to improved caller outcomes, reduced call volume and better resource use. This aligns with Edwards et al's (2015) study, which had a broader theme of implementing targeted interventions for frequent callers, emphasising the need for personalised, data-driven strategies to understand and address the diverse needs of this caller demographic effectively.
Smith and McNally (2014) describe a staged approach to the management of frequent callers, beginning with low-level interventions, such as a letter like McDonnell et al (2022) or phone call, and escalating to multidisciplinary meetings if these are not effective. This approach is tailored towards the needs of the caller, not the service.
Snooks et al (2019) evaluated strategies using a survey identifying policies or pathways used by UK ambulance services to manage frequent callers. They found multiple strategies and interventions aimed at managing and reducing the rates of calls from frequent callers to ambulance services. These strategies mainly involved some form of case-management approaches as in Edwards et al's (2015) study, in addition to multidisciplinary approaches and home-visit assessments. The key emphasis in all of these strategies was the provision of interventions to manage the demand for ambulance services and improve caller outcomes.
Snooks et al (2019) stressed the need for any frequent-caller interventions to have a person-centred approach to manage complex needs more effectively. The effectiveness of interventions is dependent on the caller's context and individual needs; further research to refine and develop these strategies is needed.
Evaluating the effectiveness of interventions
It is essential to evaluate the effectiveness of interventions implemented on reducing ambulance services use by frequent callers. While some studies report positive results, such as decreased call frequency (Edwards et al, 2015) and improved caller experience (Smith and McNally, 2014), there is an emphasis on the need for further research and assessment of interventions' effectiveness in a broader context (Snooks et al, 2019; McDonnell et al, 2022).
Interventions in the studies by McDonnell (2022), Edwards et al (2015) and Smith and McNally (2014) all resulted in a reduction in call volume, consistent with other studies noting a reduction in frequent attenders to emergency departments following similar interventions (Elston et al, 2022; Hudon et al, 2022; Sillero-Rejon et al, 2023). Smith and McNally (2014) identified short-term improvements in safeguarding, productivity, caller experience and outcomes as significant indicators of success, although they do not state how this was evaluated beyond the reduction in call volume. McDonnell et al (2022) relied on a single intervention without considering other approaches or a control group, which limits the ability to assess the full effect of the mass-distribution letter on call volumes accurately.
Snooks et al (2019) found that, out of 13 UK ambulance services, seven did not audit or evaluate frequent call data at that time, three did not respond or said the survey was not applicable and the other three services reviewed only individual cases or pilot schemes. This demonstrates a paucity of evaluation of data from UK ambulance services. This finding is supported by Zayed et al's (2020) study based on a service review of ambulance service management of callers who have self-harmed, which also showed a lack of follow-up and evaluation of data from UK ambulance services.
Snooks et al (2019) support implementing tailored approaches to meet person-centred needs, in addition to further research to determine the efficacy of the identified interventions in reducing the impact on ambulance services.
To ensure best practices are shared and resources are used more effectively, it is essential that ambulance services collaborate and share information (Skogevall et al, 2024).
Edwards et al (2015) identify that evaluating and auditing ambulance service data regarding frequent callers are important for several reasons, including to help understand caller characteristics and needs and enable data analysis. Ambulance services can then identify patterns and trends to develop interventions and strategies to address frequent callers' needs and close gaps in care. Some frequent callers may contact ambulance services if they are not receiving adequate medical care elsewhere rather than for vexatious reasons; they need compassion and empathy from practitioners (Snowdon, 2022).
Multi-component interventions or a combination of interventions tailored to individual needs may be more effective in addressing the issue of frequent callers; longer post-study observation periods are needed to assess the length of time for which such interventions are effective. Evaluation of practices can provide crucial insights and learning that can help in the implementation of more effective interventions (Clarke et al, 2019; Snooks et al, 2019). Understanding these practices can shed light on the challenges faced and areas that require improvement (Schultes, 2023). The goal would be to meet the needs of frequent callers more effectively while ensuring ambulance services can operate efficiently and support all callers who require emergency care.
Limitations of the research area
There appears to be some promising evidence to support strategies to reduce the impact of frequent callers to ambulance services. However, there is limited research exploring interventions for frequent ambulance callers specifically, and a lack of control groups, limiting analysis and preventing firm conclusions of efficacy.
In addition to this, the impact of frequent callers and their needs are complex, hence the need for further research to enhance service provision and care of this caller group.
Implications for practice
There are potential issues with implementing identification systems and strategies, such as resource availability and cost. Multidisciplinary cooperation and sharing information to benefit both services and callers is essential.
Although the strategies reviewed on reducing frequent ambulance callers show promising results, further research is required to evaluate their long-term effectiveness and sustainability before they can be included in guidance or policy.
A staggered approach combining various strategies may be effective, initially with mass-generated letters to educate frequent callers on appropriate use of services, progressing to more costly and time-consuming personalised approaches and interventions such as phone calls and case-management and caller-management systems.
Conclusions
This literature review adds to the evidence base demonstrating that frequent callers pose a unique challenge to ambulance services and there is a strong need for investment in interventions to help meet their needs and reduce impact on services.
Clear definitions and identification systems are essential for ambulance services, in addition to information-sharing across services and exploring multi-component strategies.
Evidence on existing strategies has been explored to gain a deeper understanding of frequent ambulance caller needs to support the transformation of management approaches. Strategies such as case management, mass-distribution letters and frequent-caller management systems all show promising results for addressing and reducing the impact of frequent callers, in addition to ensuring person-centred care.

