Good-quality chest compressions have been the cornerstone of cardiac arrest management since the 1960s and are one of the few interventions proven to improve survival from out-of-hospital cardiac arrest (Feneley et al, 1988; Stiell et al, 2014a). Defining the ‘quality’ of chest compressions, however, can be challenging, although international guidelines and the UK Resuscitation Council emphasise quality in respect particularly to chest compression rate, depth and recoil (Olasveengen et al, 2021; Soar et al, 2021).
Chest compressions should be performed at a rate of 100–120 per minute to maintain coronary perfusion pressure (CPP). Rates that are too slow will allow CPP to fall, reducing perfusion, and rates that are too high will cause reduced cardiac filling and subsequent falls in CPP. This recommended rate is based upon two studies with a combined population of 13 469 patients who achieved higher rates of survival at this compression rate (Idris et al, 2015). Very high chest compression rates were associated with decreased chest compression depth and suboptimal cardiopulmonary resuscitation (CPR) (Stiell et al, 2014a).
Chest compression depth is of clear significance and several studies have demonstrated improved outcomes with depths of 45–55 mm (Hostler et al, 2011; Stiell et al, 2012a; 2014b; Vadeboncoeur et al, 2014) and a compression depth of 50–60 mm is now advocated by the European Resuscitation Council (2021). Even when performed optimally, this is likely to result in a cardiac output of no greater than 25–40% of pre-arrest values. It has been suggested in a small-scale animal study that a reduction in compression depth of 30% can significantly reduce CPP and subsequent successful resuscitation (Ristagno et al, 2006). However, no large-scale study has been undertaken to validate these results.
Adequate compression depth allows for optimal ventricular compression moving blood into the pulmonary and systemic circulation. In addition, ventricular filling is significant in optimal CPR and full chest recoil must also be facilitated. If the rescuer is leaning on the anterior chest wall, they may be failing to allow for sufficient chest wall recoil between each compression. It is thought such practice allows fatigued rescuers to inadvertently ‘rest’ between each compression. This practice impedes venous return and ventricular filling but evidence suggests that the practice is commonplace during CPR (Niles et al, 2011; Fried et al, 2011).
Leaning should be avoided as facilitating complete chest wall recoil after every chest compression improves venous return and may help make CPR more effective (Zuercher et al, 2010; Aufderheide, et al, 2005; Yannopoulos et al, 2005).
Aim
The aim of this study was to determine if chest compressions performed from a lateral position are more effective than chest compressions performed from an over-the-head position in a cohort of UK student paramedics. Quality was determined by assessing various metrics including chest compression rate, depth and recoil.
Methods
Seventy-five student paramedics from the University of Wolverhampton were recruited using a convenience and purposeful sampling methodology and inclusion criteria were limited to any individual enrolled in a BSc paramedic science programme who had participated in initial undergraduate education relating to basic life support (BLS). All individuals were deemed competent in both over-the-head and lateral CPR. Demographic data are given in Table 1.
| Sex | |
|---|---|
| Male | 20 |
| Female | 55 |
| Age* | 22.6 (4.39) |
| BMI* | 26.74 (6.5) |
| Study level (all undergraduate) | |
| Level 4 (year 1) | 52 |
| Level 5 (year 2) | 18 |
| Level 6 (year 3) | 5 |
| Date of last training | |
| <6 months | 53 |
| 6–12 months | 17 |
| 12–24 months | 5 |
*Mean and standard deviation
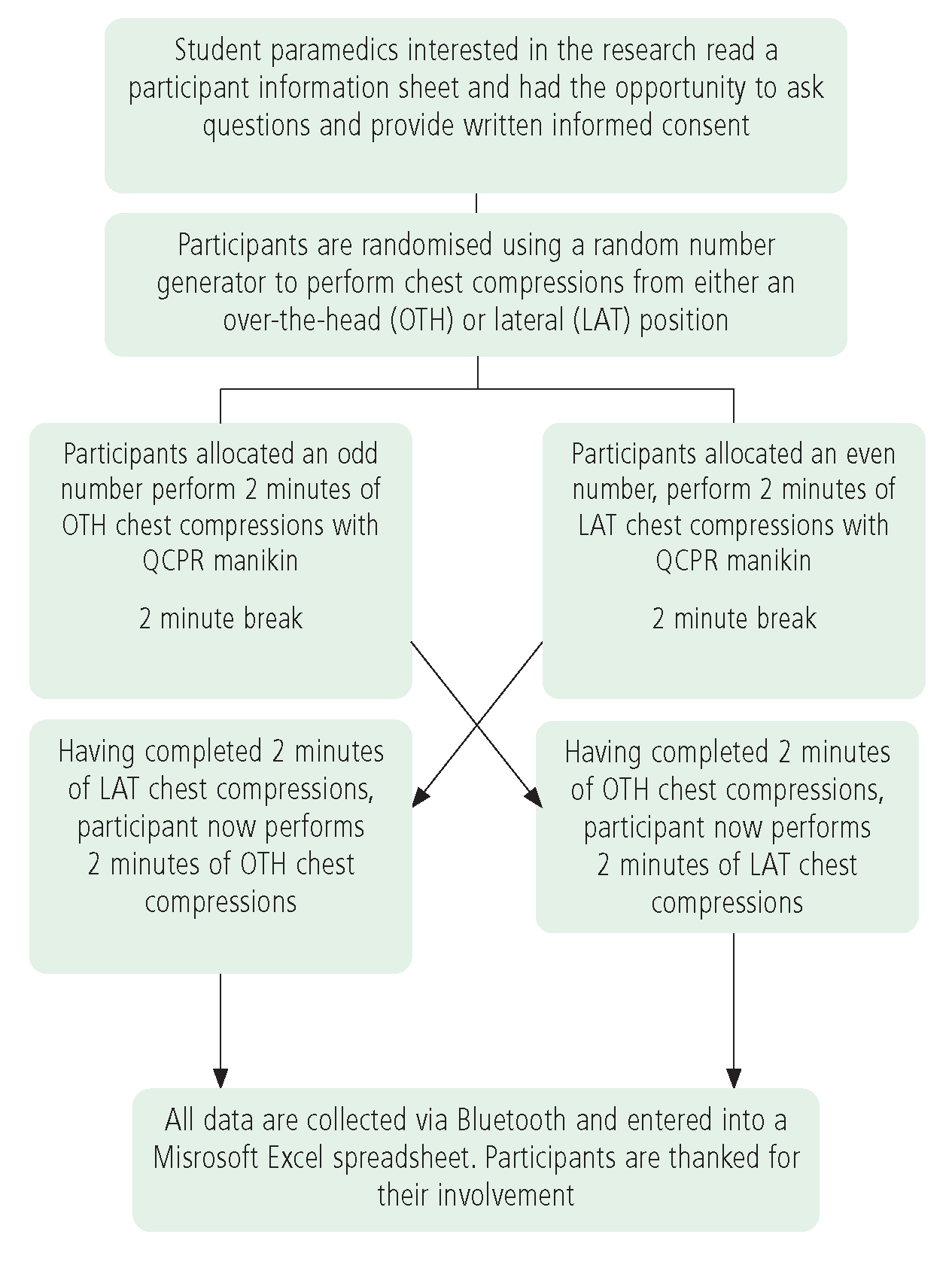
A random number generator was used to randomise students to one of the two arms of this crossover study. Odd numbers would perform over-the-head (OTH) chest compressions initially and even numbers would perform lateral (LAT) chest compressions initially. This simple method of randomisation was chosen to ensure that bias could be eliminated as far as reasonably possible. Participants were asked to perform continuous chest compressions and were not expected to ventilate the manikin. Following 2 minutes of continuous chest compressions, participants were then asked to stop and rest for 2 minutes before undertaking a further 2 minutes of chest compressions from the alternative position (Figure 1).
Chest compressions were performed on a Laerdal adult QCPR manikin that was linked remotely via bluetooth to an instructor's device which recorded various metrics (visible to the researcher only) including:
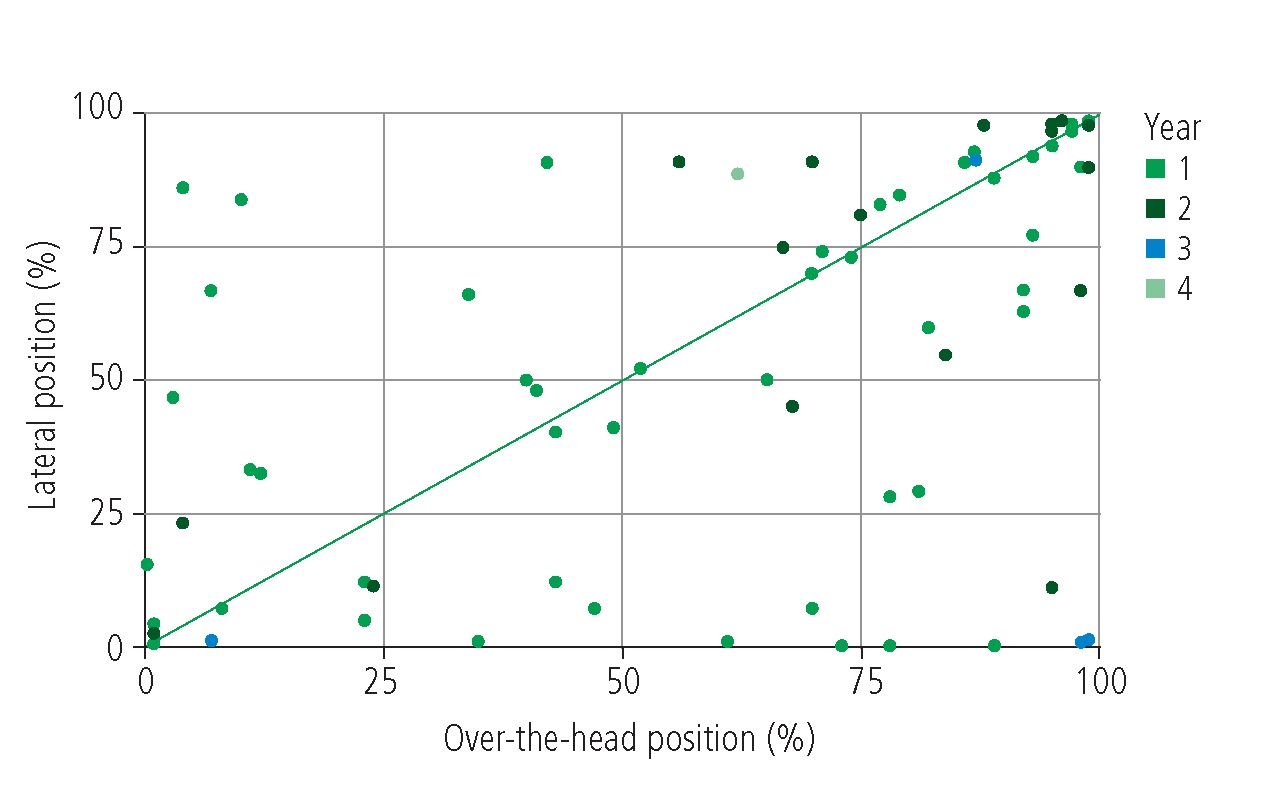
The primary outcome measure was the proportion of effective chest compressions performed in 2 minutes (Figure 2). The secondary outcome measures used to determine effective chest compressions are listed in Table 2.
| Cardiopulmonary resuscitation position | P | ||
|---|---|---|---|
| Lateral (LAT) | Over the head (OTH) | ||
| Total compressions* | 221.8 (216.9–226.6) | 222.6 (217.4–227.8) | 0.455 |
| Compressions with no error (%) | 66 (12–90.5) | 73 (37.5–92.5) | 0.183 |
| Compressions with adequate depth (%) | 47.9 (5.5–92) | 32.0 (6–89.5) | 0.406 |
| Mean compression depth (mm)* | 47.3 (44.9–49.6) | 47.1 (44.9–49.2) | 0.774 |
| Compressions with adequate recoil (%) | 88.0 (22.5–100) | 92.0 (47.5–100) | 0.109 |
| Chest compression fraction (%) | 100 (100–100) | 100 (100–100) | 0.542 |
Median, interquartile ranges and Wilcoxon rank sum P value unless indicated. *Mean, 95% confidence interval and paired t-test P value
For the primary outcome, P<0.05 was regarded as significant. To adjust for multiple testing, for all secondary outcomes, P<0.01 was used. For outcome data, paired t-tests and Wilcoxon rank sum tests were used to compare the effects of the two different CPR chest compression positions under assumed approximate normality and non-normality of outcome distributions. Student paramedics were not given any feedback about their performance and no financial remuneration or other incentives were offered for participation.
Ethical considerations and approval
The study received ethical approval from the research ethics committee at Queen Mary University of London and complied fully with Good Clinical Practice, the Declaration of Helsinki and relevant legislation.
Results
Seventy-five student paramedics participated in the study; baseline demographic data are displayed in Table 1.
Chest rompression rate
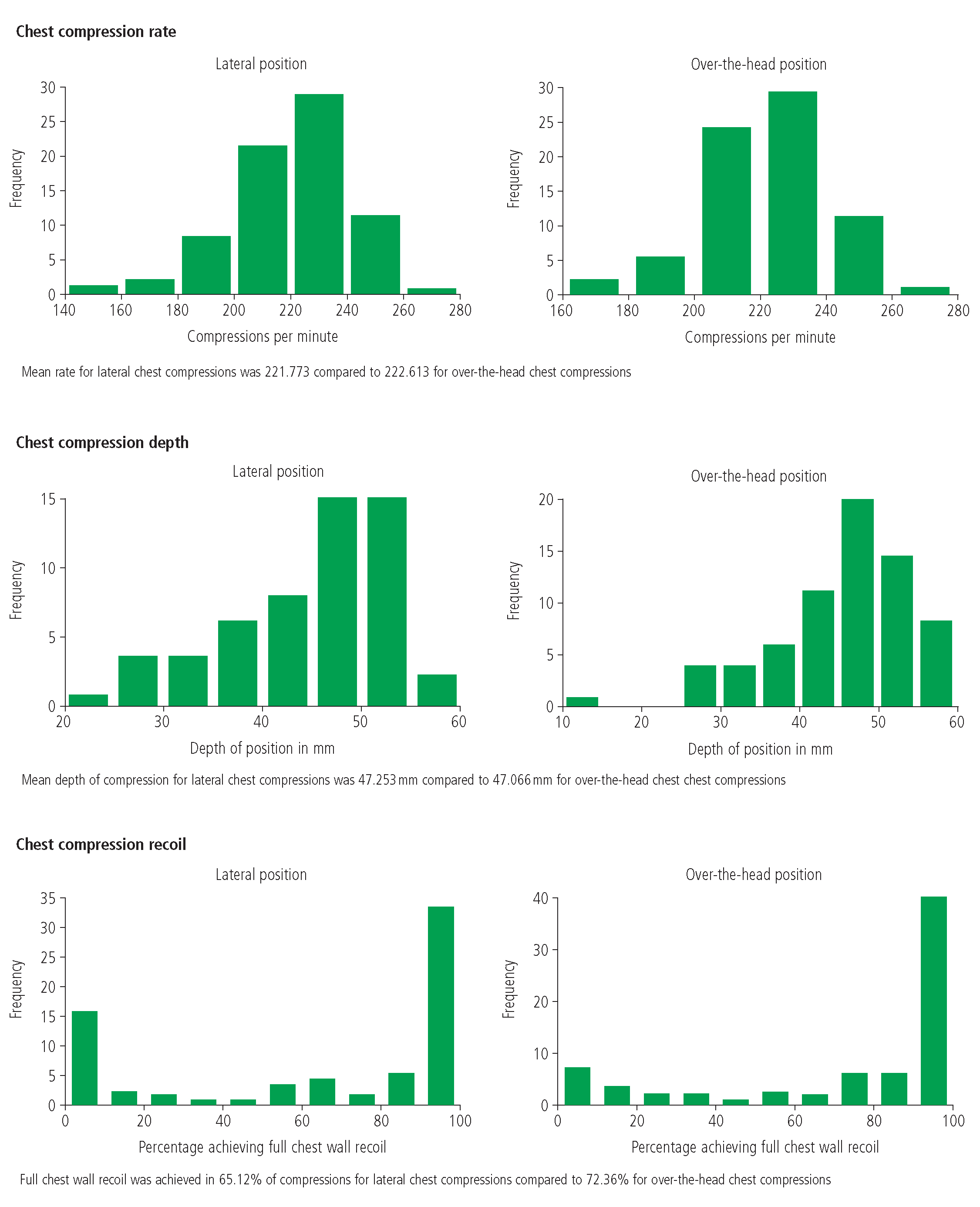
Chest compression rates (the mean number of LAT compressions was 221.773 (216.9–226.6) over a 2-minute period compared with 222.613 (217.4–227.8) for OTH compressions) (p=0.455) were similar between the two arms of this study; 60% of student paramedics performed >240 compressions in a 2-minute cycle (Figure 3).
Chest rompression depth
In the LAT arm, 41/75 (54.67%) student paramedics performed chest compressions with a mean depth outside international guidelines. In the majority of cases, compressions were of insufficient depth (37/41; (90.24%). In the OTH arm, 46/75 (61.33%) student paramedics performed chest compressions with a mean depth outside international guidelines; in the majority of cases, compressions were of insufficient depth (42/46; 91.30%). Overall mean depth in the LAT arm was 47.3 mm (44.9–49.6), compared with 47.1 mm (44.9–49.2) in the OTH arm (p=0.774) (Figure 3).
Chest rompression recoil
Full chest wall recoil was achieved in 92% (47.5–100) of compressions for rescuers in the OTH position compared with 88% (22.5–100) for rescuers in the LAT position (p=0.109) (Figure 3).
Discussion
The principal finding is that there was no substantial difference between chest compression quality between those performed from an OTH position and those from the lateral position measured against a range of metrics (Figure 2).
This study shows that OTH compressions are as effective as lateral ones and are a viable alternative in the difficult-to-access arrested patient. Although no significant differences were observed between the two arms of this study, another key theme emerged: in both groups, chest compressions were frequently performed suboptimally across a range of metrics. These two themes form the basis of this discussion.
Effect or rescuer position
Chest compression rates (the mean number of LAT compressions was 221.773 over a 2-minute period compared to 222.613 for OTH compressions) and depths (mean depth LAT: 47.253 mm; mean depth OTH 47.066 mm) were similar between the two arms of this study, suggesting that rescuer position had minimal impact on these two metrics. Chest compression recoil, however, although similar, was more nuanced.
Full chest wall recoil was achieved in 92.0% of compressions for rescuers in the OTH position, contrasting somewhat with 88.0% for rescuers in the LAT position.
It has not been possible to determine the reasons for this but one possibility is that rescuers in the LAT position find that it is easier to rest or lean between compressions than in the OTH position, resulting in more effective chest wall recoil. This practice of leaning on the anterior chest wall during CPR in order for the rescuer to conserve energy impedes venous return and cardiac output; however, the practice is commonplace and may occur in up to 91% of cases. Fried et al (2011) have suggested that the practice could be mitigated by the use of automated feedback devices.
Fried et al (2011) have suggested that the practice could be mitigated by the use of automated feedback devices. Many such devices also monitor rescuer hand position and the authors of the present study found that hand position was more often correct in the OTH position. Further research is required to assess the accuracy of hand position placement during chest compressions and whether hand dominance has any impact upon the quality of chest compressions.
Suboptimal rate and depth
While there was no evidence that rescuer position affected the quality of chest compressions, the authors found chest compressions were frequently performed suboptimally and that a significant percentage of student paramedics performed chest compressions at a rate inconsistent with international guidelines.
This research has demonstrated that almost 60% of student paramedics perform >240 compressions in a 2-minute cycle. It is likely that compression rates were excessively fast. This finding appears to be consistent with the Resuscitation Outcomes Consortium, which reported that EMS rescuers frequently applied compression rates of >100/minute, with rates >120/minute occurring in one third of cases (Idris et al, 2012). Faster than recommended compression rates remain well established in the literature (Wik et al, 2005; Fletcher et al, 2008).
There are, of course, inherent limitations with manikin-based studies but it is probable that actual compression rates would be increased further during the management of a cardiac arrest because of performance stress.
Various authors have suggested the use of metronomes as a device to ensure optimal compression rates and there is empirical evidence demonstrating their effectiveness as a tool for providing optimal rates of chest compressions (Kern et al, 1992; Fletcher et al, 2008).
This lack of adherence to international guidelines was not limited to chest compression rate. Chest compression depth was also consistently suboptimal regardless of rescuer position. In the LAT arm, 41/75 (54.67%) student paramedics performed chest compressions with a mean depth outside international guidelines. In the majority of cases, compressions were of insufficient depth (37/41; 90.24%). This was also reflected in the OTH arm, where 46/75 (61.33%) student paramedics performed chest compressions with a mean depth outside international guidelines; in the majority of cases, compressions were of insufficient depth (42/46; 91.30%).
Multiple studies have demonstrated a correlation between chest compression depth and survival (Hostler et al, 2011; Stiell et al, 2012b; 2014c). Vadeboncoeur et al (2014) undertook a prospective analysis of 593 patients who presented with cardiac arrest of presumed cardiac aetiology and found mean depth was significantly deeper in survivors (53.6 mm) than non-survivors (48.8 mm). The authors concluded that each 5 mm increase in chest compression depth significantly increased the odds of survival and survival with favourable neurological outcome (Vadeboncoeur et al, 2014).
This research has not determined the reasons why compression depth is frequently suboptimal. However, a lack of underpinning knowledge of the mechanism by which chest compressions drive forward the flow of blood, limited clinical exposure and infrequent continuous practice and robust assessment with feedback are likely to be contributory factors.
Limitations
Although a sample size calculation was performed, the COVID-19 pandemic meant recruitment had to be terminated prematurely resulting in a sample size of 75. Data were collected from just one higher education institution and this research is not sufficiently powered to draw any conclusions with statistical confidence.
While this study is bound by the inherent limitations of manikin-based studies, it has contributed to the existing body of knowledge in this area and the authors hope readers will digest their research in this context.
Conclusion
There was no statistically significant difference in the quality of chest compressions between the two positions and, while cognisant of the study's inherent limitations, the authors concur with previous authors that over-the-head chest compressions are equally as effective as lateral compressions and, in some areas, might confer marginal gains.
Hand placement was more often correct in the over-the-head position and this position appeared to provide more effective chest wall recoil as well. Further research is required in this area. Hand placement was more often correct in the OTH position, which also appeared to provide more effective chest wall recoil. This is likely due to rescuers having to stretch to reach the mid-to-lower third of the sternum and therefore over-stretching and compressions performed too inferiorly are unlikely to occur. It is probable that this position also makes leaning on the anterior chest wall less likely.
Although no significant difference between the two positions was noted, there was deviation from international guidelines in several metrics including chest compression rate, which was frequently too fast, and chest compression depth, which was often too shallow.
Although it is not possible to extrapolate this data to student paramedics nationwide, it is possible these findings are not unique. This provides UK higher education institutions with an opportunity to collaborate with researchers to identify whether the metronomes and automated feedback devices could be used to improve BLS training. While the investment might be small, the outcomes could be huge.

