
Learning Points
Electrocardiograms (ECGs) have become an integrated part of an ambulance clinician's toolkit, with thousands being performed each year (Brady et al, 2012). Invented in 1903 by Willem Einthoven, a dutch physiologist, the ECG has become a necessary non-invasive diagnostic tool for identifying cardiac and non-cardiac conditions, such as electrolyte imbalances, pulmonary embolisms, various coronary syndromes, cardiomyopathy and arrhythmias (Brady et al, 2012; Harrigan et al, 2012).
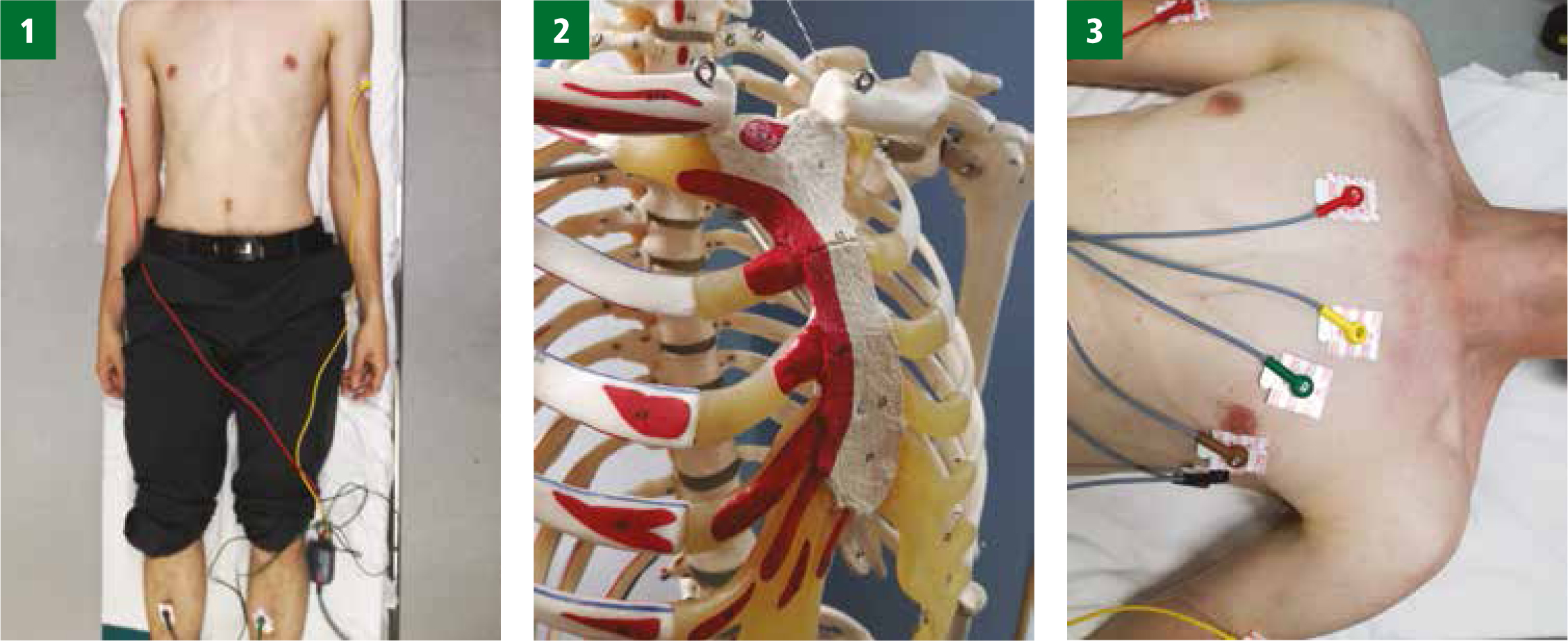
This article is designed to support clinicians in locating the landmarks which are vital for correct ECG electrode placement (Figure 1). It is imperative for clinicians to be trained in ECG electrode placement and maintain their skills (Brady et al, 2012; Health and Care Professions Council (HCPC), 2016).
While the 12-lead ECG is an essential diagnostic tool, inaccurate lead placement can result in a wave amplitude change, causing misinterpretation—and potentially, inappropriate treatment for patients (Kania et al, 2013; Dougherty et al, 2015). McCann et al (2007) and Karnia et al (2013) highlight inaccurate placement of the electrodes on the chest and limbs prior to the recording taking place as a significant issue. Harrigan et al (2012) suggest that inaccuracies could lead to up to 24% of ECGs being incorrect; however, there has been little research carried out in the out-of-hospital environment.
Considerations prior to ECG
The Society of Cardiological Science and Technology (SCST) (2017) recognises that 12-lead ECGs are taken in a wide range of environments and under varying degrees of emergency and urgent situations. However, clinicians are encouraged to strive for best practice in all conditions.
Patient positioning
The supine/horizontal position is recommended for 12-lead ECG recordings; any variant of the patient's position should be documented as it may create misleading results (Brady et al, 2012; Crawford, 2012; SCST, 2017). A semi-recumbent position of no more than 45o from the supine can be considered if more appropriate (SCST, 2017). The limbs should be relaxed and supported to minimise interference of amplitude on the ECG reading (Dougherty et al, 2015).
Dignity, diversity, equality
Differences, such as gender, religion and culture, should be respected, and clinicians should ensure they adhere to the HCPC (2016) code of conduct, performance and ethics. Health professionals should respect cultural sensitivities of the patient and minimise embarrassment (HCPC, 2016). Patients may feel uncomfortable and self-conscious about a 12-lead ECG being taken; therefore clinicians should promote care, compassion and empathy (Keough, 2014; HCPC, 2016). Following the completion of the ECG, the patient should be re-dressed or covered with a blanket, and a consultation about the findings should then proceed (Nicol et al, 2013; Marcus et al, 2018).
Electrode placement
The following leads are required to perform a 12-lead ECG: limb leads I, II, III (Bipolar leads); limb leads: aVR, aVL and aVF; chest leads: V1, V2, V3, V4, V5 and V6.
Limb leads
Quite simply, limb leads should be placed on the limbs, not the torso, as this can affect the wave amplitude on the ECG (Dougherty et al, 2015; SCST, 2017). Limb electrode positions:
Readers who trained a few years ago may remember the useful mnemonic ‘read your green book’ to recall the colour sequence (Figure 1; Image 1).
Chest leads
Studies have demonstrated that the V1 and V2 electrodes are frequently placed too high and the V4, V5 and V6 electrodes too low (Alinier et al, 2006; Soliman, 2008; Khunti, 2013; Khan et al, 2015). These errors can result in diagnostically misleading alterations to the ECG waveform (Rajaganeshan et al, 2007).
The angle of Louis (or Manubriosternal joint) must first be found to ensure the intercostal spaces are located for the correct placement (Figure 1; Image 2). This is located by placing a finger on the sternum and running it downward until a ridge on the sternal bone is felt (Day et al, 2015; SCST, 2017).
The third intercostal space should be in line with the angle of Louis; count this and then locate the fourth intercostal space. Common mistakes are made here as V1 and V2 electrodes are placed too high if the fourth intercostal space has not been correctly located. V1 and V2 leads should be placed ether side of the sternum in the fourth intercostal space. Find the fourth space on the left sternal edge as rib spacing can differ on either side. Conversely, the V3, V4, V5 and V6 are placed too low (Rajaganeshan et al, 2007; Day et al, 2015; Marcus et al, 2018).
The V4 electrode should be placed in the fifth intercostal space, in line with the mid-point of the clavicle. The V3 should be placed midway between V2 and V4. The V5 and V6 electrodes should then be positioned in horizontal alignment with the V4 electrode. The V5 electrode should be placed on the anterior axillary line and the V6 electrode should be placed on the mid-axillary line (Figure 1; Image 3).
Other considerations
Breast tissue
At present, there is limited evidence to suggest ECG electrode placement is affected by breast tissue (Macfarlane et al, 2004; Wallen et al, 2014). The SCST (2017) suggests placing V4, V5 and V6 under the breast. Use the back of the hand to lift the breast and endeavour to respect dignity, care and sensitivity while placing electrodes (Williams et al, 2013; HCPC 2016; SCTC, 2017). You could consider the patient lifting their own breast; however you must ensure they do not shift their position too much as this may affect the placement of the electrode. Breast implants have little impact on 12-lead ECG unless they cover the fifth intercostal space or have leakage from the implant itself (Williams et al, 2013; HCPC, 2016; SCTC, 2017).
Patients who have had a mastectomy may have scar tissue which could affect the contact of the electrode with the skin; therefore, in this situation, be mindful of this and ensure good skin contact with the electrode (Crawford et al, 2001; Nicol et al, 2013; Wallen et al, 2014).
Obesity and extensive muscle tissue
Excess tissue and muscle fibres can create a barrier when locating the angle of Louis and intercostal spaces (Crawford et al, 2001). Clinicians tend to assert more pressure when trying to locate the key anatomical landmarks, which can cause patient discomfort (Crawford et al, 2001). More experienced clinicians are recommended to perform the 12-lead ECG in this case (SCST, 2017).
Tremor and movement
Tremors or movement can affect the ECG recordings. Any variation caused by movement or tremor on the standard 12-lead ECG record should be documented (Dougherty et al, 2015). If the patient is experiencing pain or has a neurological condition such as Parkinson's disease, or if there is anything affecting their relaxation, this should be documented. Any difficulties and variation should be documented accordingly on each ECG trace taken.
Compassion and care
The unique out-of-hospital environment can be distressing to a patient as they have experienced an unexpected event which has resulted in the ambulance being called. Clinicians should be aware that this can be a distressing time for the patient, acting with compassion and care as always (HCPC, 2016).

