How to use these guides
The articles in this series, which can be torn out for use in practice, are intended to support clinician development and to assist in the overall assessment of patient presentations. The information should be used to aid consideration of differential diagnoses in situations where life-threatening conditions have been ruled out.
The extent and explanation of each examination will not be to the depth of those provided in core literature texts, so further reading and consolidation are advised to support understanding supplemental to these articles. Key questions are included for reader consideration and to direct further study.
Most examinations are taught in a rigid format. However, in clinical practice, practitioners need to be flexible and adapt their approach depending on the presenting condition and circumstances. While there is no single set way to carry out each of these examinations, a good structure will reduce omissions and errors, and support the gathering of information to inform patient care.
Contemporary texts provide the underpinning reference sources throughout this series, as many of the examination processes and techniques are universally applied; however, differences will be highlighted. Readers will be signposted to these key texts for each clinical examination.
The series will cover the following systems:
- Cardiovascular system
- Peripheral vascular system
- Neurological system (upper and lower limbs)
- Cranial nerves
- Gastrointestinal system
- Respiratory system
- Musculoskeletal system
Respiratory examination
This article summarises a structured approach to the assessment of the respiratory system. This examination enables clinicians to identify acute and chronic abnormalities (Lane and Rouse, 2016). Further study is required to understand the sensitivity and specificity of each assessment.
Of classifiable diagnoses, respiratory conditions are the second most common (Baker, 2017). The majority are benign and require no intervention, some are more serious but can be treated safely in the community and a few are life-threatening.
Clinicians must inform their management plan with well-structured, thorough history-taking and clinical examination. A full, in-depth examination is not necessary for time-critical emergencies.
Before starting, the clinician must introduce themselves, state their role and briefly explain what the assessment entails to obtain informed consent.
Equipment required
- Stethoscope
- Pulse oximetry device
- Peak-expiratory flow rate (PEFR) meter
- End-tidal carbon dioxide (EtCO2) monitor.
Patient positioning
The most convenient position is for the patient to sit, allowing the clinician full access to the thorax. This also allows for easier expansion of the lungs (Moore, 2017) and possibly assists with respiration in a symptomatic patient. The thorax should be exposed; dignity and comfort should be considered throughout and, where practical, a chaperone should be offered.
General observations
First, note any general observations:
- Presenting symptoms
- Respiratory rate, rhythm and depth. If possible, measure these over a full minute
- Ability to speak: can the patient talk in full sentences?
- Pursing of the lips (seen in emphysema)
- Stridor or audible breathing sounds without auscultation
- Accessory muscle use
- Obvious cyanosis
- Items of note near the patient such as medications, home oxygen, respiratory hazards (including chemical and biological) or evidence of smoking
- A productive cough, which should provoke questions over its origin and sputum details.
REFLECTION
How much can be discovered from an ‘end-of-bed’ inspection before assessment?
Hands
Consider the appearance of then inspect the hands. Start with the nails, followed by the dorsum then the palms. You should be able to recognise and consider the significance of the following:
- Peripheral cyanosis
- Minor tremors may indicate bronchodilator use (Simpson, 2006; Thomas and Monagan, 2014)
- Asterixis (flapping tremor) in CO2 retention (Simpson, 2016; Innes et al, 2018)
- Warm and sweaty hands, again in CO2 retention (Thomas and Monagan, 2014)
- Nicotine staining
- Clubbing in patients with long-term respiratory conditions is normally caused by chronic hypoxia (Simpson, 2006)
- Skin thinning associated with long-term steroid use.
A radial pulse should be taken and SpO2 recorded if not done already (Kirk, 2018a; Matthews, 2018)
- A weak radial pulse could indicate circulatory compromise from pneumothorax or haemothorax (Simpson, 2006)
- Bounding tachycardia could indicate CO2 retention (Thomas and Monagan, 2014)
- Low SpO2 should be recorded and interventions given as per local or national guidelines.
Blood pressure should be measured if not taken during the primary survey (Thompson (2018):
- Pulsus paradoxus could be sign of pericardial effusion; it could indicate severe asthma but this should have other symptoms (Sarkar et al, 2018).
REFLECTION
Why is it important to examine the hands when assessing the respiratory system?
Face
Mouth
Findings may include:
- Central cyanosis, evident on the tongue and oral membranes, which may indicate hypoxia of respiratory or cardiac origin.
Candidiasis may be present in patients on inhaled steroids or immunosuppressants (Thomas and Monagan, 2014).
Lymph nodes
Lymphadenopathy or lymphadenitis (terms often used synonymously for abnormal size, consistency, or inflammation of the lymph nodes) may indicate infection. Inflammation of the submandibular and submental lymph nodes may indicate infections of the oral cavity; tonsillar inflammation may indicate infections of the tonsillar and posterior pharyngeal regions; raised supraclavicular nodes may indicate pulmonary infections (Rawles, 2015).
Neck
Inspect the trachea. Observations could include (Rawles, 2015):
- Tracheal tug, which can be found in patients (especially paediatric) with accessory muscle use and respiratory distress
- Tracheal deviation: ipsilateral could be a sign of pulmonary fibrosis or collapse; contralateral could indicate pulmonary effusion or pneumothorax.
A raised jugular venous pressure could indicate pulmonary vasoconstriction, pulmonary hypertension or right-sided heart failure (Thomas and Monagan, 2014).
This area should be inspected for scars, which could indicate a previous surgical airway insertion.
REFLECTION
Which parts of the respiratory system can be physically seen and what can be elucidated from those observations?
Chest
The inspection, palpation, percussion, auscultation (IPPA) approach is used here.
Inspection
A full visual inspection should be done, including anterior, posterior and below both mid-axillary lines. Historical or chronic findings may include:
- Pectus excavatum (not usually clinically significant)
- Thoracotomy scars
- Surgical scars, which in older patients could be a sign of a previous tuberculosis infection
- Obvious abnormal movement such as reduced, asymmetrical or flail segments
- Hyperinflation as found in patients with chronic obstructive pulmonary disease (COPD)
- Local skin thickening associated with radiotherapy
- Prominent veins, indicating a poor venous return
- Deformities such as kyphosis and scoliosis.
Palpation
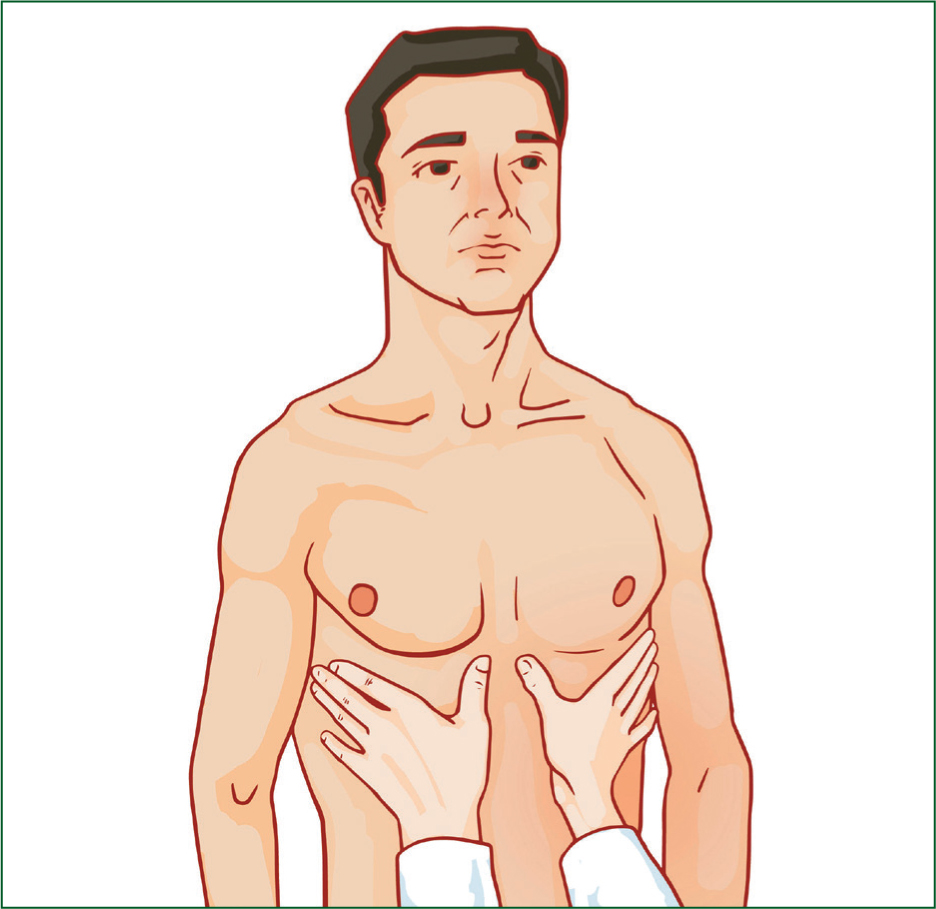
Palpation of the anterior and posterior chest should include the examinations below. Although palpation, percussion and auscultation are non-invasive, informed consent should be gained for each, and patient comfort and dignity considered.
- Chest expansion can be measured in several ways:
- First, place hands ipsilaterally on the chest wall, below the nipple line and using the fingers to anchor at the sides (Figure 1)
- Extend the thumbs so they touch at full expiration
- The patient should be asked to take in a full breath, and movement observed. The thumbs should be drawn apart; clinicians should be cautious not to pre-empt any movement
- Tactile fremitus can be tested, but vocal resonance during auscultation is usually assessed instead now (Rawles, 2015)
- Ask the patient to repeat ‘111’ and feel the vibrations. The authors prefer to use the edge of the hand along the fifth metacarpal to do this
- Trachea positioning can be determined by placing two fingers above the sternal notch then palpating (Thomas and Monagan, 2014)
- Any tenderness and crepitus should be noted, and interventions provided. Patient comfort should be considered if either is discovered.
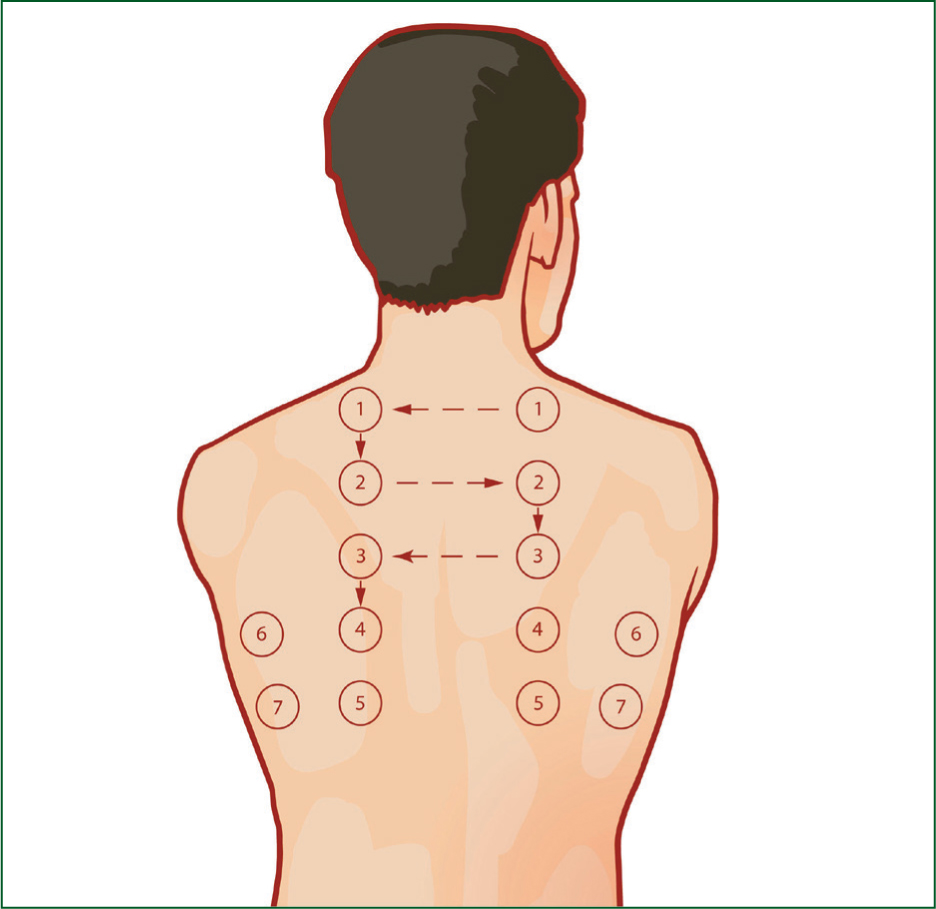
Percussion
The clinician should spread their fingers over the chest with the middle finger running along the intercostal space and pressure applied. The middle finger should then be struck quickly by the middle finger of the other hand so as not to muffle the tone. Percussion should be started above the clavicle at the lung apex, moving down the anterior of the chest at intervals of 3–4 cm (Figure 2), for comparing ipsilaterally before moving inferiorly in position (Lane and Rouse, 2016).
Percussion should be done in a quiet area; the sound produced once this skill is acquired should be audible without causing discomfort. It should be practised regularly on normal people so the clinician can recognise normal resonance and perfect the skill. The sound could be (Thomas and Monagan, 2014):
- Normal resonance with a thud and some resonance in a patient with no concerns
- Hyporesonance: where dullness can be heard over consolidation or collapse; and stony dullness over pleural effusion
- Hyper-resonance with an extended resonance indicates a lower density than expected, such as in pneumothorax or emphysema.
Auscultate
Auscultation should be completed in the anterior, posterior and axillary regions. The diaphragm of the stethoscope should be used. All lobes should be checked; there are six areas on the anterior, eight on the posterior and three in each axillary region. The patient should sit; they can be rolled on their side but only if sitting is not possible (Sarkar et al, 2015). Sounds on auscultation can include:
- Expiratory wheeze from narrowing of the airways
- Inspiratory wheeze from foreign body obstruction
- Crackles, crepitus and rales are interchangeable terms that indicate air entering a collapsed airway or mucus movement (Thomas and Monagan, 2014)
- Fine crackles (similar to pulling hook-and-loop material apart) later in inspiration result from small airways reopening or fluid in the alveoli
- Coarse crackles (like popping breakfast cereal) on inspiration and expiration indicate sputum or fluid in the airway
- Crackles at the lung base can be normal, and should clear if the patient is prompted to cough
- Rub (like creaking leather or walking on fresh snow) indicates inflamed pleural surfaces
- Absent breath sounds indicate no air movement
- Vesicular sounds are normal. Inspiration and expiration times may vary because of asthma or chronic bronchitis. Exaggerated vesicular sounds may mean the lungs are working harder because of a chronic condition or damage to one area (Sarkar et al, 2015).
Vocal resonance should be assessed. Ask the patient to repeat ‘111’ while auscultating in the same areas as above. A higher volume because of better sound conduction will be heard in areas with greater than normal density, and can indicate consolidation or collapse. An alternative is to assess for whispering pectoriloquy by asking the patient to whisper ‘111’. A true whisper should not be heard in normal lung fields. Greater sound conduction in higher-density fields allows whispers to be heard.
Temperature and PEFR should be recorded (Kirk, 2018b) and interventions considered as needed.
REFLECTION
These practical skills take practice. Am I confident in diagnosing a patient using them?
Use of the stethoscope
Many stethoscopes have a bell and a diaphragm. The bell is primarily for lower frequency sounds; the diaphragm can limit lower-frequency sounds so higher frequency sounds are more obvious. The bell has therefore been said to be superfluous in respiratory assessments (Welsby et al, 2003).
The diaphragm should be used; both high- and low-frequency sounds can be heard in normal and abnormal presentations. With the author's stethoscope, resting the diaphragm on the chest allows for auscultation of low frequencies, and restricting its movement by using firm pressure means higher frequencies can be auscultated. Stethoscopes vary so clinicians should read the instructions to use them correctly and to their full potential.
REFLECTION:
Do I really know how to use my stethoscope?
EtCO2 monitoring
EtCO2 monitoring may be used in acute and serious cases, including obstructive issues such as COPD and asthma, pulmonary embolism and heart failure resulting in dyspnoea. The expired CO2 and wave form can inform the extent and severity of conditions and the effectiveness of treatment. EtCO2 monitoring can also be useful in monitoring patients experiencing trauma or shock (Aminiahidashti et al, 2018). Deighton (2018) describes EtCO2 monitoring and its prehospital use.
REFLECTION
Can I read capnography readouts sufficiently to understand the aetiology?
Circulatory considerations
Respiratory presentations can result from a circulatory problem, especially pulmonary oedema and heart failure. Therefore, if the symptoms of respiratory distress appear to be idiopathic, a cardiovascular examination, such as that described by Dearnley-Lane (2020), should be completed.

