On 31 December 2019, COVID-19, a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported to the World Health Organization (WHO). On 11 March the next year, the WHO declared COVID-19 a global pandemic (Cennimo, 2022).
On 21 January 2020, the first confirmed case of COVID-19 in the United States was found in Washington state and reported by the Centers for Disease Control (Haynes et al, 2020). COVID-19 quickly spread across the United States, partially because transmissibility (R0) of SARS-CoV-2 is extremely high, estimated to be between 2.3 and 5.7 (Li et al, 2020; Sanche et al, 2020), placing those in regular contact with infected patients at elevated risk.
The risk of contracting COVID-19 was found to be highest for people who were regularly in close contact with those who were actively sick with COVID-19 (Zhang, 2021). This high-risk group included paramedics and paramedic students who provided essential primary emergency healthcare (Zhang, 2021) in a hostile and unpredictable environment (Barr et al, 2017).
To protect first responders and the public as infection spread, substantial changes were made to clinical care guidelines across the United States. COVID-19 is prevented through the implementation of public health measures (such as social distancing and mask wearing) and clinical practices that reduce aerosolisation of the virus (Tang et al, 2020). Changes to clinical guidelines included avoiding the use of bag-mask ventilations, prioritising preoxygenation with non-aerosolised means (Cheung et al, 2020) and limiting the use of oxygen to the lowest flow necessary to meet minimum blood oxygen saturations of 90–92% (Kovacs et al, 2020).
Simultaneously, rapid-sequence intubation and early intubation, in general, were encouraged because they allowed practitioners to control and filter a patient's exhalation and, with it, the potential for aerosolisation of COVID-19 (Brewster et al, 2020; Cheung et al, 2020).
Other changes included medication delivery changes; for example, the state of Pennsylvania authorised the use of intramuscular injections of terbutaline in place of aerosolised treatments for patients with asthma (Bureau of EMS, 2020).
Along with the changes to care recommendations, emergency medical services (EMS) call volumes decreased (Ferron et al, 2021; Goldberg et al, 2021; Satty et al, 2021) significantly nationwide and emergency department use dropped by 42%, reducing EMS students' opportunities to perform procedures critical to their education (Satty et al, 2021). This was problematic for paramedic students and patients as studies show that increased exposure to advanced airway procedure opportunities increases the success rate of airway placement and the management of respiratory emergencies in the clinical practice (Jacobs and Grabinsky, 2014).
As performing advanced airway procedures on live patients is necessary for well-rounded paramedic training and course completion, the aim of this study was to explore the effect of the pandemic on student paramedic opportunities in the United States to perform advanced airway procedures.
Methods
This retrospective study of student records explored airway procedure variables before and after the COVID-19 pandemic. Because of the timing of the pandemic and the start of research, student records from 2020 were selected from 1 July to 31 December. To minimise the effect of annual variation, student records for cases between July and December in the 3 years before the pandemic COVID-19 (2017 to 2019) were chosen for comparison.
A retrospective analysis of airway procedure data collected in the Fisdap database was conducted, comparing the 600 334 patient encounters recorded for the pre-pandemic period (July-December of 2017, 2018 and 2019) to the 128 453 patient encounters recorded during the COVID-19 period (July 2020–December 2020). Table 1 shows the original variables from the Fisdap data set before cleaning and analysis.
| Variable | Data type | Description |
|---|---|---|
| Patient ID | String | Unique case identifier |
| Patient performed | Categorical | Date of case. Dichotomised into new variable pre and post the COVID-19 period |
| Airway procedure | Categorical | Type of airway procedure attempted in case. Categories recoded into new variables |
| Airway size | Categorical | Size of airway adjunctw |
| Attempts | Ordinal | Number of attempts at procedure in each case |
| Airway success | Categorical | Whether the procedure was successfully performed |
| Airway performed by | Categorical | Whether the procedure was performed by the student or not |
The data from the two time periods were compared using descriptive and inferential statistics that included F-tests and chi-squared tests for independence. Effect size was explored using Cramer's V or eta squared to determine the strength of the association between variables where these were statistically significant. Only cases in the field were analysed—simulations and hospital-based cases were excluded from the analysis.
The Fisdap database was chosen for this study as it is a large, proprietary internet-based system of EMS student records designed to track clinical and procedural experiences. Furthermore, the Fisdap software is used by more than 175 of the 790 accredited paramedic training programmes in the United States (Cash et al, 2021).
The original data set was cleaned, duplicates removed and missing data analysis performed. The categorical variable airway procedure included all categories of all airway procedures performed in a case. Each category was separated into individual variables so the frequencies for each airway procedure could be identified.
Airway procedure variables that measured similar skill domains were combined into new variables; for example, the three types of intubation methods were combined into one variable: ‘all intubation’.
Table 1 shows the variables extracted from the original data set for each patient encounter. Twenty-one variables were included for analysis.
Inver Hills Community College Institutional Review Board provided approval for the prospective collection of paramedic student data. Approval was initially granted in 1996 and has since been renewed annually at that same institution. Students elect to provide consent for their records to be used in research when completing their account details.
Results
Table 2 shows the frequency and proportion of airway procedures before and after the pandemic period. After the data set had been cleaned and duplicates removed, a total of 728 785 student records of patient contacts were included for analysis in the study.
| Procedure | Average pre-COVID-19 frequency* (n) | Pre-COVID-19 proportion (%) | Post-COVID-19 frequency* (n) | Post-COVID-19 proportion (%) | Difference in proportion | Difference post-COVID-19 frequency† | Chi-squared | P | Cramer's V | Effect size |
|---|---|---|---|---|---|---|---|---|---|---|
| Airway procedure | 86 336 | 43.1 | 74 375 | 57.9 | 14.8 | −11961 | 9283.77 | <0.001 | 0.113 | Weak |
| Tracheostomy tube | 227 | 0.1 | 89 | 0.1 | 0.0 | −138 | 19.42 | <0.001 | 0.005 | Weak |
| Suction ET | 4205 | 2.1 | 2448 | 1.9 | −0.2 | −1757 | 19.96 | <0.001 | 0.005 | Weak |
| Suction airway (not ET) | 10 658 | 5.3 | 6831 | 5.3 | 0.0 | −3827 | 0.14 | 0.904 | N/A | |
| All suction | 13 668 | 6.8 | 8589 | 6.7 | −0.1 | −5079 | 3.45 | 0.063 | N/A | |
| All intubation | 33 050 | 16.5 | 33 805 | 26.3 | 9.8 | 755 | 6815.32 | <0.001 | 0.097 | Weak |
| PEEP | 1007 | 0.5 | 1084 | 0.8 | 0.3 | 77 | 219.52 | <0.001 | 0.017 | Weak |
| Nebuliser | 12143 | 6.1 | 4283 | 3.3 | −2.7 | −7860 | 1499.27 | <0.001 | 0.045 | Weak |
| CPAP | 6723 | 3.4 | 5025 | 3.9 | 0.6 | −1698 | 96.65 | <0.001 | 0.012 | Weak |
| Manual ventilation | 37 039 | 18.5 | 29 762 | 23.2 | 4.7 | −7277 | 1473.75 | <0.001 | 0.045 | Weak |
| NPA | 4051 | 2.0 | 3306 | 2.6 | 0.5 | −745 | 153.9 | <0.001 | 0.015 | Weak |
| Airway obstruction | 1179 | 0.6 | 2337 | 1.8 | 1.2 | 1158 | 2001.97 | <0.001 | 0.052 | Weak |
| Rapid sequence induction | 2768 | 1.4 | 1799 | 1.4 | 0.0 | −969 | 0.231 | 0.631 | N/A | |
| Ventilator operation | 3272 | 1.6 | 1831 | 1.4 | −0.2 | −1441 | 219.34 | <0.001 | 0.17 | Weak |
| Ventilator with PEEP | 1044 | 0.5 | 781 | 0.6 | 0.1 | −263 | 192.49 | <0.001 | 0.016 | Weak |
| All blind airway device | 7386 | 3.7 | 12339 | 9.6 | 5.9 | 4953 | 8208.7 | <0.001 | 0.106 | Weak |
| Respirator operation | 488 | 0.2 | 225 | 0.2 | −0.1 | −263 | 21.69 | <0.001 | 0.005 | Weak |
Figures taken from the Fisdap dataset for recorded patient contacts before (average n=200 111) and after (n=128 453) the COVID-19 period. Data before COVID-19 was collected July-December in 2017, 2018 and 2019. Post-COVID-19 data collection occurred in July-December 2020
Six-month average for the data collection from July to December in both before and after COVID-19 periods.
Post-COVID-19 proportion minus pre-COVID-19 proportion; minus sign indicates a reduction in the post-COVID-19 period
Post-COVID-19 frequency minus pre-COVID-19 frequency; minus sign indicates a reduction in the post-COVID-19 period
CPAP: continuous positive airway pressure; NPA: nasopharyngeal airway; PEEP: positive end-expiratory pressure; ET: endotracheal
For the pre-pandemic period, the number of student records was 600 334. There were, on average, 200 111 records of patient contacts per 6-month recording period in the years 2017–2019, compared to the 128 453 cases in the 6-month post-COVID-19 period in 2020. As such, 71 658 fewer cases were recorded in the Fisdap data set in the pandemic period compared to the average number of cases in the three time periods before the pandemic. With fewer overall patient contacts during the post-COVID-19 period, there was a reduction in the frequency of most airway procedures (Table 2).
However, three airway procedures (intubation, positive end-expiratory pressure (PEEP) and airway obstruction) were reported with an increased frequency in the post-pandemic period compared with the average pre-COVID-19 period, despite the lower total caseload in the later period. Table 2 shows that intubation rose by 755 cases, PEEP by 77 cases and airway obstruction by 1158 cases compared to previous periods. These increases in frequency were found to be statistically significant but with weak effect size (intubation: F(1,728785)=6879.6; P<0.001; η2=0.009; PEEP: F(1,728785)=219.6; P<0.001, η2<0.001; airway obstruction: F(1,728785)=2007.5; P<0.001; η2=0.052).
Furthermore, although the total number of cases attended during the post-COVID-19 period was lower, the overall proportion of airway procedures within the caseload increased by 14.8%. An F test showed the difference in proportion to be significant (F(1 728 785)=9403.5; P<0.001) but eta squared showed a weak effect of association (η2=0.013).
The airway procedures that increased as a proportion of the caseload in order or rank were: intubation (9.8%); blind airway device (5.9%); manual ventilation (4.7%); airway obstruction (1.2%); continuous positive airway pressure (CPAP) (0.6%); nasopharyngeal airway insertion (NPA) (0.5%); PEEP (0.3%); and ventilator with PEEP (0.1%).
Reductions in frequency were observed in: nebuliser use (−2.7%); ventilator operation (−0.2%); endotracheal tube suctioning (-0.2%); all suction (−0.1%); and respirator operation (−0.1%).
The procedures that did not change in frequency were: tracheostomy tube; suction airway (not endotracheal (ET); and rapid sequence induction.
Chi-squared for independence and Cramer's V for effect size were used to explore these distributions. Most differences were found to be statistically significant but with small effect size for association (Table 2).
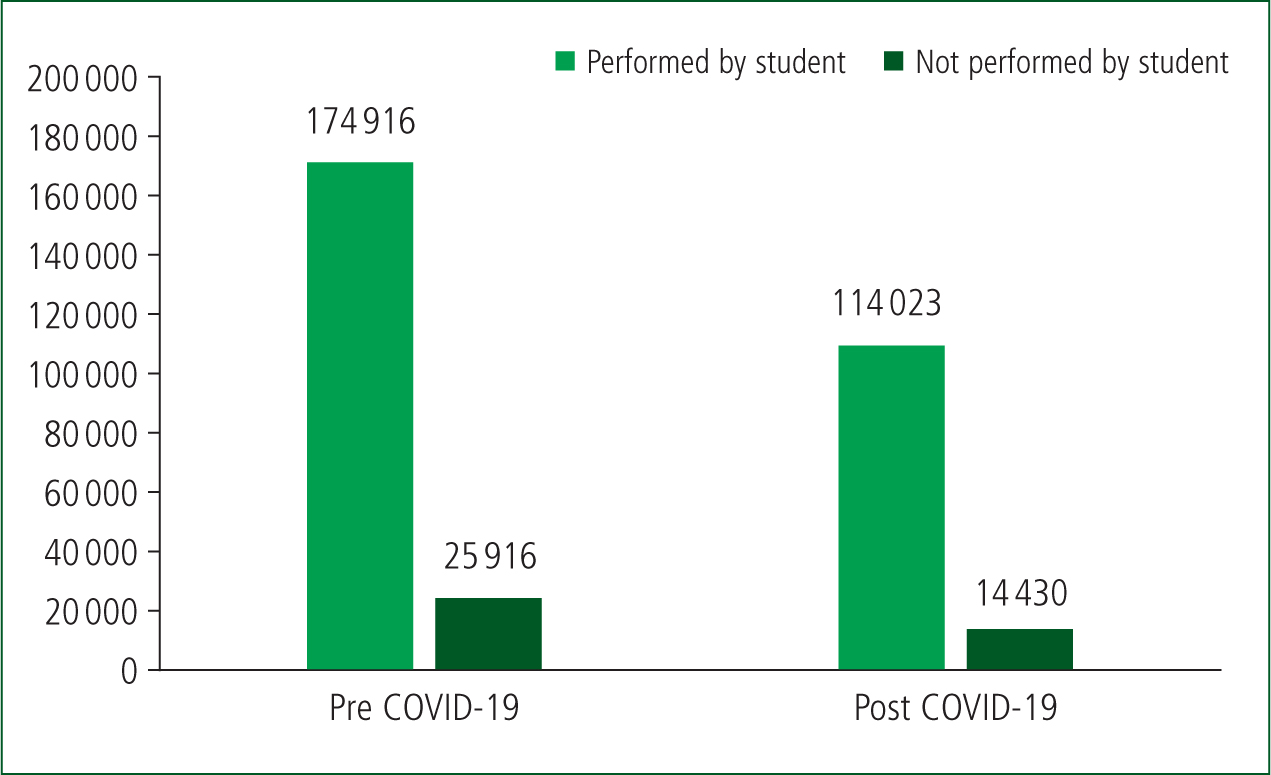
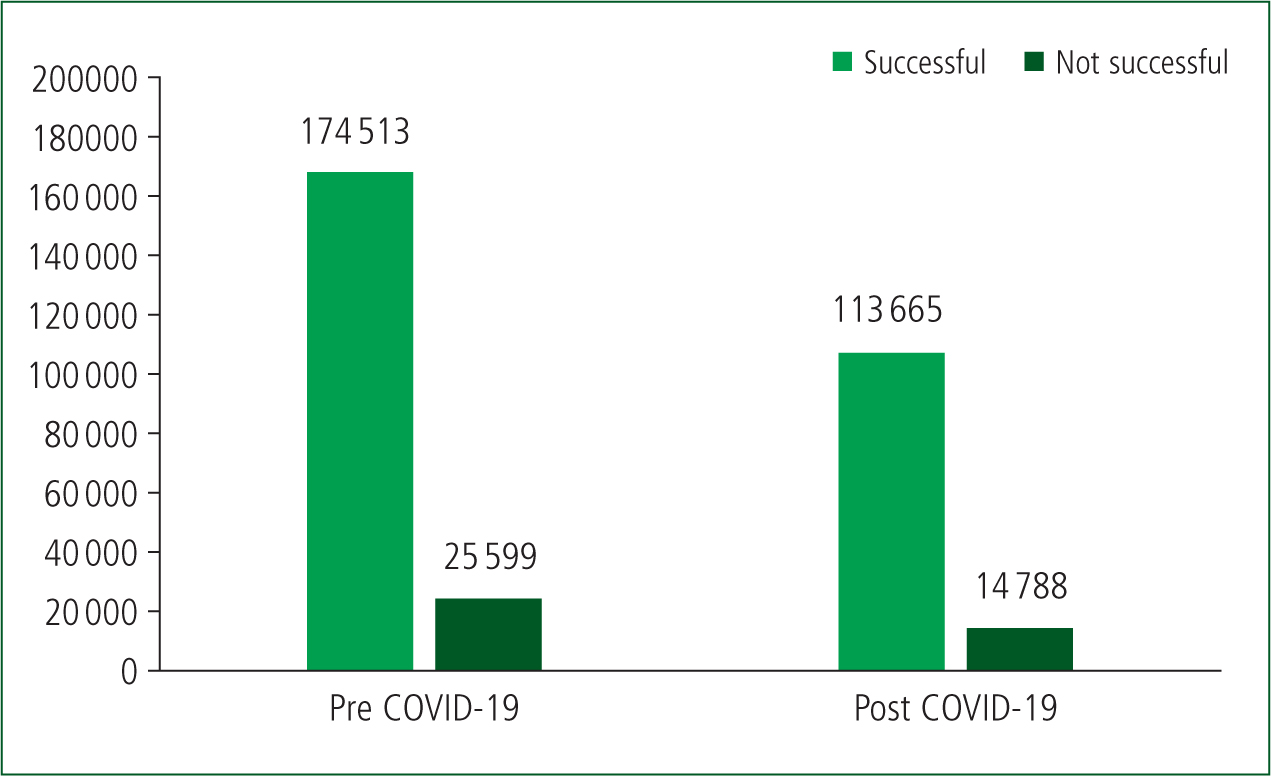
Procedures that a student is exposed to during a field placement are documented as being either performed or observed by the student. Figure 1 shows the frequencies for this variable before and after COVID-19. The data show that the frequency of airway procedure exposure fell by 34.8% from the 3-year pre-pandemic average of 174 916 cases to 114 023 cases after COVID-19. However, the proportion of skills performed by students was slightly higher in the post-COVID-19 period (87.1% before compared to 88.8% after), as did the proportion of successful airway procedures attempted by students (87.2% before compared to 88.5% afterwards) (Figure 2).
Discussion
The increase in proportion and the number of (advanced) airway procedures performed is counterintuitive. The nationwide recommendations for a reduction in the use of advanced airway procedures in patient care guidelines would be expected to lead to fewer opportunities to practise those skills across the board. Despite an overall reduction in the number of patient contacts made by students, these increases in the proportion and number of advanced airway procedures performed suggests an inherently sicker general population in the post-COVID-19 period.
This potentially provided a deeper educational experience and learning environment on in-field clinical rotations. In line with that hypothesis is the finding that the proportion of airway procedures successfully performed by students was slightly higher in the post-COVID-19 period than in the previous years. This may have been because more time and energy had been spent in simulation training before clinical rotations started to make up for the reduction of patient contacts nationwide. Nevertheless, repetition is required for skill mastery (Singhal et al, 2021) so the reduction in overall opportunities for paramedic students during the post COVID-19 period could potentially lead to paramedics in the field being underprepared.
It is important for EMS educators to consider a variety of ways to ensure the mastery of airway skills within a program of study. A potential solution to the lack of exposure and repetition of skills would be to supplement traditional education with additional time in simulation labs, skills-based training and in-hospital clinical placements with explicit learning outcomes.
It has been reported that pandemics will become more likely because of rising deforestation rates, the popularity of the unregulated wildlife trade in many countries and the reduction of biodiversity around the globe (Tollefson, 2020). EMS professionals and educators and society in general need to be prepared to adapt and overcome any problems this brings. That starts with understanding and learning from the COVID-19 pandemic. These lessons are invaluable not only for EMS students but also for all medical field personnel who require clinical-based learning opportunities if they are to be prepared for their careers.
Limitations
There were a few limitations to this study. Using student records relied on students accurately recording cases with airway procedures and all other patient contact information. As these entries are verified by the instructors, they are considered reasonably accurate.
The variable ‘performed by student’ indicates whether the student or instructor carried out the clinical procedure. It is not known if that pertains to all procedures in the case or just one procedure. The assumption is that the instructor performed all procedures in those cases. These cases were relatively stable across the two time periods (11% and 12%). A more conservative approach was taken in the analysis based on the assumption that the instructor performed all procedures in those particular cases.
Finally, analysis of large data sets can mean minor differences are identified as statistically significant. In this study, most effect sizes were shown to be weak associations, so it is important to consider clinical relevance, not just statistical significance.
Conclusion
Data presented here suggest the frequency and proportion of case type change significantly during a pandemic. There is indirect evidence that the acuity of cases may also change.
These data bring to light some issues in the current system used to decide practical skill graduation requirements in paramedic school. Going forward, students could benefit from educational institutions developing plans to adapt their clinical and skill-based requirements by ensuring they are adequate without being excessive, implementing alternative clinical placement locations, and investing in high fidelity simulation alternatives.
Consideration of how to ensure adequate training when the patient volume is unpredictable is critical, as well as the ability to adapt to simulation-based training quickly and efficiently.
Societal fluctuations, seasonal illnesses and trauma prevalence create varying clinical experiences across the nation. This study shows that pandemics also bring substantial variations in student experiences.
Now is time to consider how to move towards a more flexible, adaptable and scalable way to measure student competency in paramedicine—particularly in times of significant disruption such as that caused by pandemics.

