Post-traumatic stress disorder (PTSD) is a serious health concern. Worryingly, it is associated with all of the following:
The lifetime risk of PTSD in the general population has been reported as 5.6–10.1% (Frans et al, 2005; Kessler et al, 2012), and the 12-month prevalence in higher-income countries has been reported as 1.5–3.7% (Kessler et al, 2012; Karam et al, 2014). PTSD may be under-diagnosed in the clinical setting (Zimmerman et al, 1999), and screening is not routinely performed.
PTSD in health care
The presence of PTSD amongst healthcare workers may be of particular concern owing to the potential symptoms of hypervigilance, irritability, difficulty concentrating, avoidance behaviours, feelings of alienation, and problems sleeping. These symptoms in a health professional with PTSD may inadvertently interfere with the care of their patients. A previous survey of surgical trainees in the NHS found a prevalence of symptoms in keeping with PTSD to be at 12%, which was higher than expected (Thompson et al, 2017). Frontline emergency healthcare practitioners in prehospital emergency medicine (PHEM), the emergency department (ED), intensive care unit (ICU), and emergency operating theatres (OT), are exposed to regular stressful and traumatic events as part of their routine practice. An investigation of the effects of these events on their risk of PTSD is warranted.
A useful screening tool
The impact of events scale-revised (IES-R) is a 22-question survey that has been used to assess symptoms caused by routine stresses of life, everyday trauma, and acute stress (Wilson et al, 2004). It has been advocated as a useful screening tool for symptoms of PTSD (Morina et al, 2013). Each question addresses the frequency of common reactions to post-traumatic stress memories following an event, and the assessment is divided into three sections:
Answers are given from 0 (not at all); 1 (a little bit); 2 (moderately); 3 (quite a bit); and 4 (extremely). A total score of 24 or more indicates that PTSD may be of clinical concern (Asukai et al, 2002). A score of 33 or higher is in keeping with a probable diagnosis of acute stress response (ASR) when the symptoms last less than a month, and PTSD if they last longer than a month (Creamer et al, 2003).
Methods
Aim
The aim of the current study was to assess the effects of traumatic events on the risk of ASR and PTSD of members of staff in PHEM, ED, ICU, and OT using the IES-R scale. The authors hypothesised that there would be a high burden of hidden psychological morbidity, and that many of those most affected have not sought professional help.
Study design and setting
A cross-sectional observational study was conducted to assess the prevalence of symptoms in keeping with ASR or PTSD amongst frontline trauma care providers in PHEM, ED, ICU, and OT at a large regional trauma service in the UK. The study is reported according to Standards for Reporting Qualitative Research (SRQR) recommendations (O'Brien et al, 2014).
Ethical considerations
Approval from a Research Ethics Committee was not required in accordance with the online National Research Ethics Service (www.nres.nhs.uk), since the survey was entirely voluntary and anonymous, and no participant identifying details were obtained. Institutional approval was granted prior to data collection (Ref: CARMS-12636).
Survey tool
An anonymous online survey tool (SurveyMonkey Inc; Palo Alto, CA USA) was sent to each department using dedicated email distribution lists. Members of staff were asked to complete the survey on a completely voluntary basis. Additional printed copies were left in the department for participants who did not wish to complete the questions online, and an anonymous collection box was provided. The first half of questions replicated the IES-R questionnaire; the remainder asked about the experiences of the participants, and factors relating to team work and support, in the same fashion as a previous investigation of surgical trainees (Thompson et al, 2017). Most questions required a categorical answer, but there were some spaces for free-text for participants who wished to use these.
Although the study investigators are all healthcare practitioners in the same field, they did not complete questionnaires, and did not have any face-to-face interaction with study participants. This was to preserve anonymity and reduce the risk of influencing answers by participants.
Data collection
The survey was open from April 2016. The decision was made that when no surveys were completed over a full week, this would be the sample saturation point, and the survey was closed. This occurred in October 2016. After this period, summary data were collated centrally. Participant information included gender; age category; ethnicity; years of experience; prior or current military experience; full-time or less than full-time employment; role; and department. An IES-R score was calculated for each participant.
Data analysis
Summary data are presented as number and percentage for categorical data. Study participants were dichotomised according to their IES-R score; those with a score of 33 or higher (a score in keeping with a possible diagnosis of ASR or PTSD (Creamer et al, 2003) were compared to those with a score lower than 33. Categorical data are compared using Chi-squared test with Yate's correction for continuity. A p-value of <0.05 was considered significant.
Results
Study participants
There were 181 study participants, and their characteristics are shown in Table 1. There were no significant differences between IES-R categories for any of the participant characteristics (i.e. gender; age; ethnicity; years of experience; military experience; full-time/less than full-time working pattern; employment role; location).
| Characteristic* | All (N=181) | IES-R ≥ 33 (N=27) | IES-R < 33 (N=154) | p-value |
|---|---|---|---|---|
| Male gender | 65 | 8 (30) | 57 (37) | 0.603 |
| Age category | ||||
| 18–24 | 11 | 1 (4) | 10 (6) | 0.902 |
| 25–34 | 58 | 10 (37) | 48 (31) | 0.705 |
| 35–44 | 66 | 7 (26) | 59 (38) | 0.309 |
| 45–54 | 29 | 8 (30) | 21 (14) | 0.071 |
| >55 | 17 | 1 (4) | 16 (10) | 0.459 |
| Ethnicity | ||||
| Asian | 11 | 1 (4) | 10 (6) | 0.902 |
| Afro-Caribbean | 4 | 0 (0) | 4 (3) | 0.891 |
| Caucasian | 158 | 24 (89) | 134 (87) | 0.787 |
| Undisclosed | 8 | 2 (7) | 6 (4) | 0.756 |
| Years of experience | ||||
| 0–5 | 44 | 10 (37) | 34 (22) | 0.153 |
| 6–10 | 47 | 8 (30) | 39 (25) | 0.816 |
| >11 | 90 | 9 (33) | 81 (53) | 0.101 |
| Military experience | 28 | 6 (22) | 22 (14) | 0.445 |
| Less than full-time | 26 | 3 (11) | 23 (15) | 0.822 |
| Role | ||||
| Nurse or healthcare assistant | 123 | 20 (74) | 103 (67) | 0.607 |
| Doctor | 46 | 5 (19) | 41 (27) | 0.514 |
| Paramedic | 12 | 2 (7) | 10 (6) | 0.860 |
| Location | ||||
| Intensive care unit | 78 | 9 (33) | 69 (45) | 0.368 |
| Emergency department | 54 | 10 (37) | 44 (29) | 0.510 |
| Emergency theatre | 27 | 5 (19) | 22 (14) | 0.782 |
| Prehospital | 20 | 3 (11) | 17 (11) | 0.991 |
| Undisclosed | 2 | 0 (0) | 2 (1) | 0.552 |
Impact of events
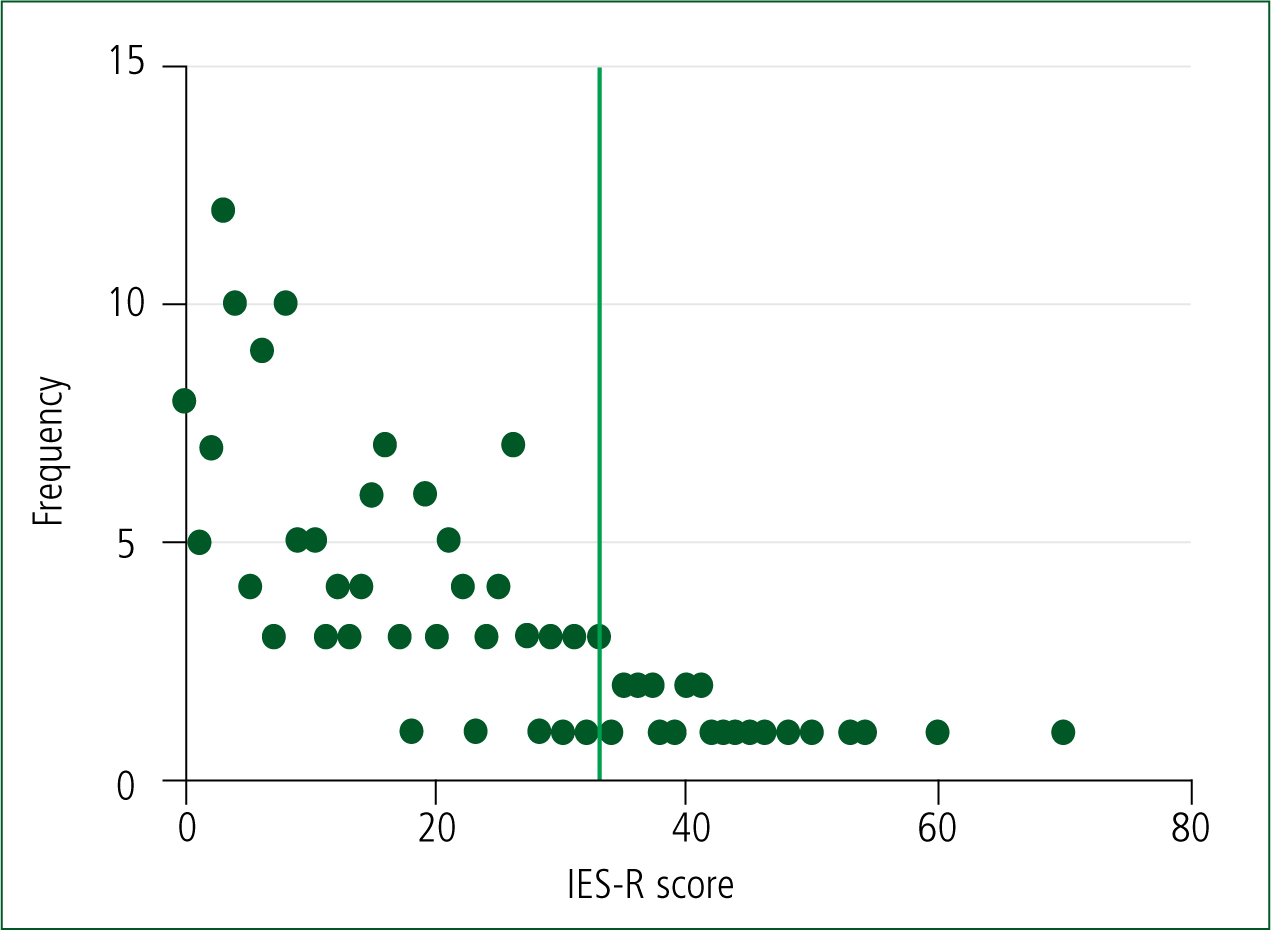
There were 27/181 (15%) participants who scored 33 or higher according to the IES-R tool. There were 8 participants with symptoms lasting less than a month, and 19 (10.5%) with symptoms lasting longer than a month, in keeping with a possible diagnosis of PTSD. A further 26/181 (14%) scored from 24 to 32—the range of clinical concern or potentially partial PTSD symptoms. The frequency of scores for all participants is illustrated in Figure 1.
Experiences
When participants were asked about their experiences of 10 types of stressful events, there was a high burden of stress among all participants. However, there were no experiences that showed significant differences between the IES-R ≥33 and <33 groups (Table 2). Six of 27 participants with IES-R scores of 33 or higher answered that they believed patient safety would be compromised by their stressful experiences.
| Experience* | All N=181 | IES-R ≥ 33 (N=27) | IES-R < 33 (N=154) | p-value |
|---|---|---|---|---|
| Injured military patient | 115 (64) | 18 (67) | 97 (63) | 0.881 |
| Dying patient | 148 (82) | 21 (78) | 127 (82) | 0.755 |
| Cardiac arrest | 151 (83) | 25 (93) | 126 (82) | 0.268 |
| Traumatic injury | 144 (80) | 22 (81) | 122 (79) | 0.992 |
| Pain | 143 (79) | 22 (81) | 121 (79) | 0.931 |
| Major burns | 119 (66) | 17 (63) | 102 (66) | 0.912 |
| Acute haemorrhage | 133 (73) | 21 (78) | 112 (73) | 0.755 |
| Life altering injuries | 142 (78) | 22 (81) | 120 (78) | 0.872 |
| Liaising and support families in severe distress | 141 (78) | 22 (81) | 119 (77) | 0.814 |
| Dealing with acute psychological trauma | 124 (69) | 21 (78) | 103 (67) | 0.368 |
Support and mentorship
There were 29/181 (16%) participants that answered that they had received some professional help in the past (including pharmacological treatment) for mental health issues. Seven of the 27 participants with IES-R scores of 33 or higher had sought professional psychiatric intervention (5 with symptoms longer than 1 month; and 2 with symptoms less than 1 month). In contrast, 10 of the 27 participants with scores of 33 or higher answered that they had used alcohol or other un-prescribed drugs in order to manage their stress.
Teams
When asked whether they worked in a group called a ‘team’, 171/181 (94%) answered ‘yes’, and this was not significantly different between the IES-R ≥33 and <33 groups. Questions regarding team behaviour (working together in a coordinated manner; having explicit common objectives; formally reviewing performance) were lower, indicating that the phenomenon of ‘pseudo-teams’ may be present (Table 3). A ‘pseudo-team’ is a phenomenon described by West and Lyubovnikova (2013) as a group of people who call themselves (or are called by others) a ‘team’, and yet they have different ideas about team objectives; they work alone or in different groups towards contrasting goals, with highly variable team boundaries; and individuals are unsure who is a member of the team, and who is not. There was a low number of positive answers (39%) when asked about whether participants either had a ‘mentor’ or knew of a ‘mentorship programme’ at their place of work (Table 3).
| Question* | All | IES-R ≥ 33 N=27 | IES-R < 33 N=154 | p-value |
|---|---|---|---|---|
| Do you have a ‘mentor’? | 104 (57) | 14 (52) | 90 (58) | 0.669 |
| Does your employer organise a formal ‘mentorship’ programme? | 71 (39) | 8 (30) | 63 (41) | 0.372 |
| Is the group in which you work in called a ‘team’? | 171 (94) | 24 (89) | 147 (95) | 0.357 |
| Does your group: | ||||
| Work together in a coordinated interdependent manner? | 157 (87) | 24 (89) | 133 (86) | 0.961 |
| Have an explicit common objective? | 162 (90) | 26 (96) | 136 (88) | 0.364 |
| Formally review its own performance, and make changes to improve? | 129 (71) | 22 (81) | 107 (69) | 0.298 |
Discussion
The main finding from the current study is that 15% of frontline emergency practitioners, drawn from multiple employers across a single region in the UK, had reactions to stress in keeping with a possible diagnosis of ASR or PTSD; yet only a small proportion of these (7/27) sought professional support. A further 14% were at a potential clinical risk, with partial symptoms. There did not appear to be any predictive characteristics of participants or stressful experiences that might allow for identification of individuals at risk. The level of risk of PTSD in this population is similar to that of other health professionals (Thompson et al, 2017). However, it is much higher than the expected prevalence of 1.5–3.7% for a higher-income country (Karam et al, 2014).
Repeated episodes of trauma
Frontline emergency providers are exposed to repeated episodes of trauma throughout their working lives, as confirmed by the answers of those participants surveyed in the present study. Repeated traumatic events may increase the risk of PTSD (Breslau et al, 1999; Kessler, 2000), which may account for the higher-than-expected IES-R scores. Exposure to these events cannot be avoided; therefore, efforts to protect, support and manage frontline emergency providers may need to be directed towards appropriate support networks, and healthy behaviours which may increase resilience.
Perceived lack of support
A perception of reduced social support can be a risk factor for PTSD following traumatic events (Brewin et al, 2000; Ozer et al, 2003). Although no causal link can be made from the study, a lack of mentorship, support and appropriate team behaviours were reported by participants. A holistic approach to addressing these would be required by any service seeking to reduce risk to its employees.
Treatment
The National Institute for Health and Care Excellence (NICE) recommends trauma-focused cognitive behavioural therapy or (CBT) eye movement desensitisation and reprocessing (EMDR) be offered to all with PTSD (National Collaborating Centre for Mental Health and NICE, 2005). These treatments cannot be delivered if sufferers do not seek professional help. It is a concern that more individuals ‘self-treated’ their stressful symptoms with alcohol or other drugs than sought psychological intervention.
Barriers to help-seeking
Barriers to self-presentation include:
Addressing such barriers may require systematic change in attitudes amongst healthcare workers so that help is sought in an appropriate manner which does not compromise patient care.
Limitations
Although the survey was anonymous and voluntary for participants, the survey design is at potential risk of selection bias, since those volunteers with strong feelings one way or another may be more likely to return a questionnaire. No formal psychiatric assessment was undertaken for any participant in this study, and IES-R scores were attributed without clinical exposure. The study survey was brief, and did not address mental health issues other than the potential symptoms of PTSD. It is possible that other psychological comorbidities were prevalent among the survey respondents, but are not presented here. The IES-R is one of several screening tools for PTSD, but all of these are lacking in high sensitivity and specificity (Shalev et al, 1997). Rather than being diagnostic, the survey in the current study was designed to screen for the potential presence of hazardous symptoms amongst a population in which this may be of particular concern.
Conclusion
There appears to be a hidden and unaddressed prevalence of symptoms in keeping with PTSD, amongst frontline emergency healthcare practitioners that is higher than that found in the general population. A minority of these have sought professional support. There is an urgent need to address this issue in order to protect those frontline workers who are exposed to repeated episodes of trauma, and optimise patient care.

