Methamphetamine use in Australia has attracted substantial attention from the media in recent years (Usher et al, 2015), with more than 100 newspaper articles on the issue published in 2014 alone (Lim et al, 2014). Methamphetamine, particularly in its purest form ‘ice’, has a high potential for harm with users often displaying erratic, sometimes violent behaviour leading to ambulance and/or police attendance (Fulde and Forster, 2015). Between 2012 and 2013, ambulance attendances related to methamphetamine use almost doubled from 592 to 1112 (Lloyd et al, 2014). However, it is likely that these figures do not capture all methamphetamine-related attendances, as emergency ambulance data collection may not include cases related to chronic drug use, only acute episodes (Lloyd et al, 2015). The prevalence and effects of this drug have led to it being labelled as an ‘Ice Epidemic’ by Australian media outlets, politicians and policy makers (Chalmers et al, 2016).
Methamphetamine is a highly addictive recreational stimulant commonly used within the Australian drug-taking community (Quinn et al, 2013). It is a psychostimulant that increases the release of noradrenaline, serotonin and dopamine from nerve endings (Kish, 2008), giving the user a feeling of alertness, wakefulness, well-being and euphoria (Quinn et al, 2013). The three major forms of methamphetamine used in Australia are speed, base and crystal methamphetamine (Ice). Ice consists of clear crystal shards and is the highest purity of the three forms of methamphetamine, with purity at upwards of 80% (McKetin, 2005). Base has an oily texture and is approximately 20% pure (McKetin, 2005). Speed is a white powdery substance with a low purity of 10% (McKetin, 2005). However, the purity of powdered methamphetamine has been reported to have increased to 37% in recent years (Scott et al, 2015).
Methamphetamines can be administered in a number of ways. The most common use is intravenous, but smoking, ingesting, intranasal and anal administration are also used (Australian Criminal Intelligence Commission 2016; Stafford and Breen, 2016). The drug is sourced through both domestic production in clandestine laboratories and through international importation. Manufacture occurs through converting precursor compounds such as pseudoephedrine and phenyl-2-propanone into methamphetamine using reactive metals or acids (Quinn et al, 2013).
There are a number of health issues experienced by users of methamphetamine. While the scenario of a drug-related psychosis may be perceived as typifying methamphetamine use, this condition only makes up a minor portion of the mental health issues experienced (Darke et al, 2008; Lim et al, 2014). Depression, anxiety, suicidal ideation and suicide attempts, are all particularly common amongst users (Darke et al, 2008). Methamphetamine is also known to cause cardiotoxicity and places significant strain on the heart causing cardiomegaly, coronary vasospasm and aortic dissection (Darke et al, 2008). Polypharmacy is also common with this population and individuals can suffer from issues associated with other drug use such as opioid overdose and dependence (Quinn et al, 2013). Physical disability is common with half of all regular users developing some form of physical disability as a result of their use. Twenty percent of users go on to subsequently have a moderate or severe disability (McKetin, 2005). Other common complaints among users are sleep disturbances, teeth grinding, weight loss and generalised chest pain (Darke et al, 2008). The most common presentations leading to hospital admission are agitated delirium, acute psychosis, assault, injury and suicide attempts or ideation (Gray et al, 2007).
There is a significant impact on health providers, both the staff and services, due to methamphetamine related admissions. One study has shown that amphetamine related hospital presentations make up 1.2% of the overall workload of emergency departments (Gray et al, 2007). Others estimate that anywhere between 7% and 18% of psychiatric admissions to hospital are directly related to use of this drug (Gray et al, 2007; Cloutier et al, 2013). These patients can be volatile and aggressive with this presentation associated with prolonged length of stay in the emergency department requiring significant resources to manage. These patients have been shown to have a dose-related increase in violent behaviour, independent of psychotic episodes, which impacts on emergency services both inside and outside of the hospital (McKetin et al, 2014). A recent enquiry in emergency department violence showed that 43% of assaults on staff were perpetrated by a person affected by drugs or alcohol, although the exact proportion of methamphetamine use was not made clear (Parliament of Victoria, 2011).
Methamphetamine use has become a significant issue for emergency ambulance services around Australia. There has been a documented increase in methamphetamine related ambulance attendances in recent years (Lloyd et al, 2014). In the 2003/2004 financial year there were less than 5 ambulance attendances per 100 000 Victorian residents. In the 2012/2013 financial year this increased to over 25 attendances per 100 000 Victorians (Lloyd et al, 2014). However, there has been little research on the impact of methamphetamine use on emergency health services (Fulde and Forster, 2015). The increase in ambulance attendances necessitate ambulance services and personnel being adequately educated and capable of rendering effective assistance to this cohort of patients and therefore further research in this area is warranted (Lim et al, 2014, Lloyd et al, 2014). This paper aims to determine the current body of research surrounding the use of methamphetamine in Australia and its impact on emergency ambulance services by using a scoping study framework. The results of this study may be used to inform practice and guide future research in this area.
Methods
This study used scoping review methodology which aimed to identify, map and review existing literature on a selected topic (Levac et al, 2010). The search was inclusive of both peer-reviewed research and grey literature (i.e. non peer-reviewed material and material that may lack sufficient basic bibliographical information such as author or publishing body) in order to obtain a broad overview, identify gaps in the literature, and inform further research. This scoping review used the methodology was originally developed by Arksey and O'Malley, (2005) and further developed by Levac et al, (2010). The six stages of scoping reviews are:
Each of these stages are discussed below.
Step 1: Identifying the research question
Coverage of methamphetamine use in the mass media has been increasing, as has utilisation of emergency medical services for methamphetamine-related events (Hughes et al, 2011; Lim et al, 2014; Lloyd et al, 2014). The research team identified two broad research questions designed to identify relevant information about methamphetamine prevalence and its impact on emergency ambulance services: (a) Who is currently using methamphetamine in Australia and how has prevalence changed over time? (b) What is the impact of methamphetamine use on emergency ambulance services in Australia?
Step 2: Identifying the relevant studies
The search strategy used two separate engines OVID and Scopus. The OVID engine was used to search Medline, Embase, EBM Reviews and PsycARTICLES full text, while Scopus was searched separately. The MeSH terms used in the database search included psychostimulant*, amphetamine*, methamphetamine* and Australia. Grey literature such as government reports were located through online searches as well as examination of reference lists from relevant peer-reviewed publications.
Step 3: Study selection
Titles and abstracts of articles retrieved in Step 2 were screened independently by two authors using the inclusion and exclusion criteria outlined in Table 1. Articles selected by both researchers were collated and duplicates were removed. The full text of selected studies was then read in depth to ensure relevance to this study, and a final number of included articles was agreed upon by both researchers.
| Inclusion | Exclusion |
|---|---|
| Written in English | Written before 2005 |
| Focused on methamphetamine use | Focused on specific treatment methods |
| Australian data used | Focused on drug use other than methamphetamine |
Step 4: Charting the data
Data from the included articles was placed into tables related to their study design (Tables 2–4). These tables include information about the article such as journal title, article title, aims, results and conclusions. The data was extracted by one researcher and reviewed by the other to ensure relevance to the research questions.
Step 5: Collating, summarising and reporting results
Relevant themes to address the research questions were established by the research team. The themes are explored in depth in the discussion portion of this paper.
Step 6: Consultation
The scoping methodology used in this study includes an optional sixth stage of consulting relevant parties external to the authors, such as experts in the area of interest or pertinent community organisations. Given the lack of previous research regarding the impact of methamphetamine on emergency ambulance services, this stage was omitted.
Results
Applying the general search strategy into OVID found 656 results. A search of Scopus found a further 769 articles. A further nine government and research centre reports were identified and those with the most recent available data from the National Illicit Drug Reporting System (IDRS) and the National Drug Strategy Household Survey (NDSHS) were included. Title and abstract review and removal of duplicates revealed 63 to be subject to full-text screening. After in depth review of each article by both researchers, 38 articles remained for inclusion (Figure 1).
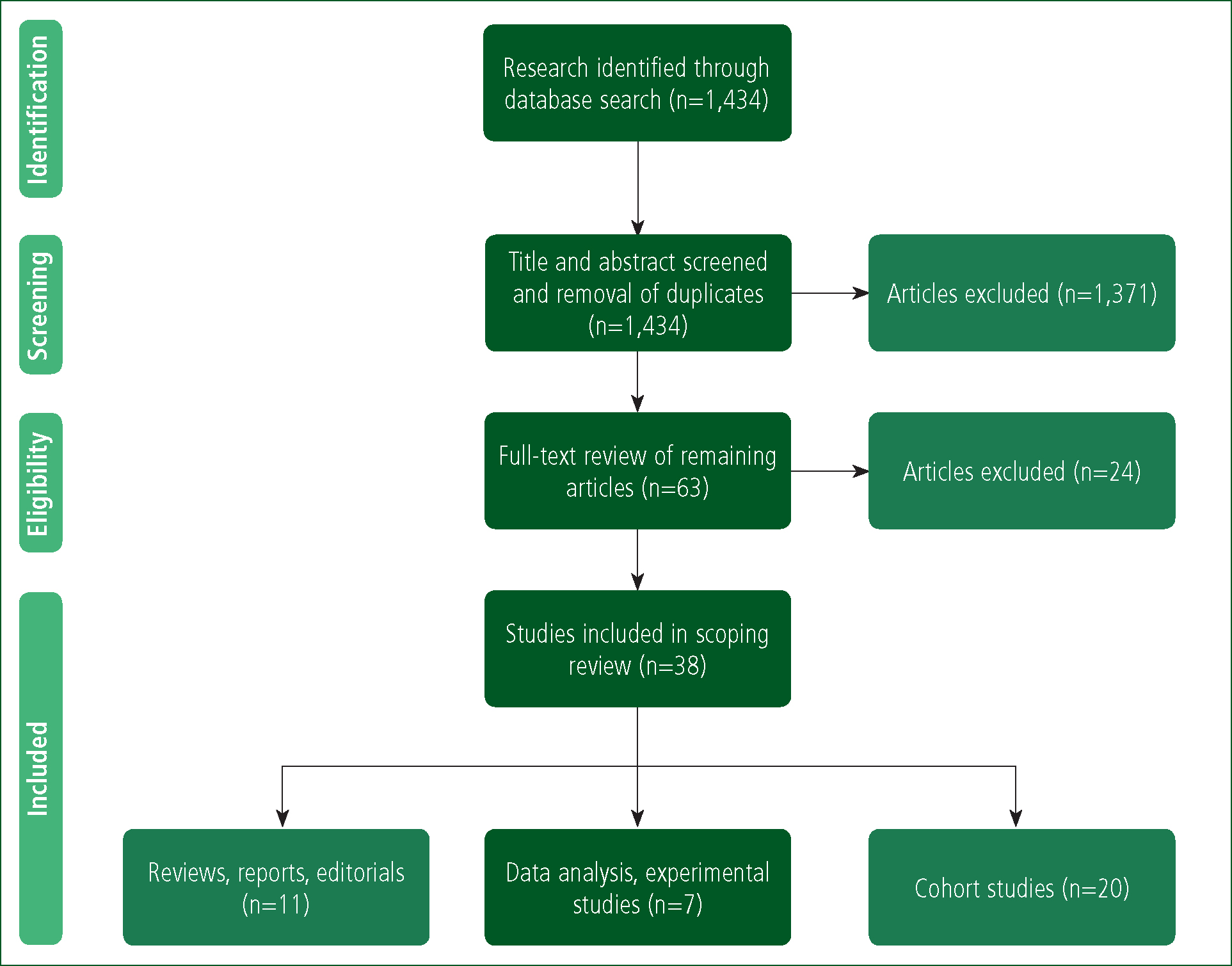
The included articles were separated into three tables. Table 2 included literature reviews, government reports and editorials (n=11), Table 3 comprised articles reporting on data analyses and experimental studies (n=7), and Table 4 outlined articles using cohort studies (n=20). The most common journal to publish methamphetamine-related studies was Drug and Alcohol Review, with 12 of the included articles being published there. There were no articles found in journals directly related to pre-hospital care. Two articles were published in emergency medicine journals (Tables 2–4).
| Author, Date | Date | Title | Journal | Design | Conclusions |
|---|---|---|---|---|---|
| Al-Obaidi TA, Fletcher SM (Al-Obaidi and Fletcher, 2014) | 2014 | Management of clandestine drug laboratories: Need for evidence-based environmental health policies | Environmental Health and Preventive Medicine | Review | Clandestine drug laboratories are a growing environmental health issue in Australia. More research and guidelines are needed for the safety of the public and health workers who may come into contact with them. |
|
Australian Institute of Health and Welfare
|
2014 | National Drug Strategy Household Survey detailed report 2013 | Australian Institute of Health and Welfare | Government Report | MA use continues to be stable at 2.1% while use of crystal MA has increased from 22% to 50%. |
|
Caldicott D, Pigou PE, Beattie R and Edwards JW
|
2005 | Clandestine drug laboratories in Australia and the potential for harm | Australian and New Zealand Journal of Public Health | Review | Clandestine drug laboratories are an increasing issue in Australia. Clinicians should be made aware of potential harms and chemicals used in this environment to help mitigate potential injuries. |
|
Darke S, Kaye S, McKetin R, Duflou J
|
2008 | Major physical and psychological harms of methamphetamine use | Drug and alcohol review | Review | MA use is associated with a number of serious health consequences. While psychosis is given significant coverage many other serious issues can be caused by MA use. |
|
Fulde G and Wodak A
|
2007 | Ice: Cool drug or real problem? | Medical Journal of Australia | Editorial | While use of MA is relatively stable harms associated with MA use have increased. More funds should be allocated to health-based approaches than law-enforcement approaches to this problem. |
|
Greene SL, Kerr F, Braitberg G
|
2008 | Review article: Amphetamines and related drugs of abuse | EMA Emergency Medicine Australasia | Review | Amphetamine abuse is common in Australia. Patients present to ED with varying issues including amphetamine toxicity and secondary complications. |
|
Lloyd B, Matthews S, Gao XC
|
2014 | Trends in Alcohol and Drug related Ambulance Attendances in Victoria 2012/13 | Turning Point | Data Analysis | There has been a significant increase in the number of ambulance attendances related to crystal MA. This has been more significant in rural Victoria. |
|
Ritter A
|
2007 | Methamphetamine alarm: Are we forgetting what we know? | Drug and Alcohol Review | Editorial | There has been significant research into MA use in Australia. Drawing on this knowledge will assist in interventions. Policy responses should be based on an illicit drugs combined approach not MA specific. |
|
Roxburgh A and Burns L
|
2015 | Cocaine and Methamphetamine related drug-induced deaths in Australia, 2011. | National Drug and Alcohol Research Centre | Research Centre Report | In Australia in 2011 there were 101 MA-induced deaths among those aged 15-54 years. The rate of MA-related deaths in this cohort was 8.1 per million persons (compared to 7.1 in 2010). MA was the underlying cause of death in 21% of all MA-related deaths. |
|
Searby A, Maude P and McGrath I
|
2015 | Growing Old With Ice: A Review of the Potential Consequences of Methamphetamine Abuse in Australian Older Adults. | Journal of Addictions Nursing | Literature review | Older MA users may demonstrate considerable effects of long-term MA use, including psychological comorbidity, psychological distress (eg. paranoia), chronic cognitive deficits, and blood-borne viruses from needle-sharing behaviour. Health services catering to their needs must be informed about the complex and unique needs of this cohort. |
|
Stafford J, Breen C
|
2016 | Australian Drug Trends: Findings from the Illicit Drug Reporting System (IDRS) | National Drug and Alcohol Research Centre | Research Centre Report | The use of ice/crystal was significantly higher in 2015 (67%) compared to the previous (2014) report (61%). Recent use of and base remained stable and speed was lower in 2015 (25%) compared with 2014 (30%) |
| Author, date | Date | Title | Journal | Design | Aim/Research question | Results, Findings | Conclusion |
|---|---|---|---|---|---|---|---|
| Degenhardt LG, Sara R McKetin A, Roxburgh T, Dobbins M, Farrell L, Burns and W Hall |
2017 | Crystalline methamphetamine use and methamphetamine-related harms in Australia. | Drug and Alcohol Review | Data analysis | To describe how changes in the availability and use of Crystal MA have impacted on MA-related harms in Australia. | Increase in the number of laboratory detections, domestic seizures and drug purity indicates that the availability of crystal MA has increased. More users are using crystal MA rather than the lower purity powder MA, and more frequently. |
Increased availability and use of crystal MA have been associated with an increase in MA-related harms (dependence, psychosis, violence and crime) |
| Degenhardt LS, Larney G, Chan T, Dobbins M, Weier A, Roxburgh WD, Hall and McKetin |
2016 | Estimating the number of regular and dependent methamphetamine users in Australia, 2002–2014. | Medical Journal of Australia | Data analysis | To estimate the number of regular and dependent MA users in Australia | The population rate of regular MA use in 2013-14 was 2.09%, compared to 0.74% in 2009-10 and the previous peak rate of 1.22% in 2006-7. | There have been substantial increases in the numbers of both regular and dependent users of MA since 2010. These increases were most evident among those aged 15-34 years. |
| Degenhardt L, Roxburgh A, Black E, Bruno R et al |
2008 | The epidemiology of methamphetamine use and harm in Australia | Drug and Alcohol Review | Data analysis | To provide an overview of current data on the epidemiology of MA use in Australia | Prevalence of MA use has remained low at 2-3% over the last 10 years. Use of crystal MA in regular injecting drug users increased from 14% in 2000 to 57% in 2006. | Availability of crystal MA has increased and this has been reflected by increased use by injecting drug users |
| Irvine R, Kostakis C, Felgate P, Jaehne E et al |
2011 | Population drug use in Australia: A wastewater analysis | Forensic Science International | Experimental | To study wastewater samples in metropolitan and regional areas to estimate stimulant drug use and compare use to established European data. | Ecstasy was high in rural areas whilst MA was high in metropolitan areas. MA use was seen to be 30-times higher than in European cities | This method of analysis shows MA use to be high in metropolitan cities. |
| Lai FY, Thai PK, O'Brien J, Gartner C et al |
2013 | Using quantitative wastewater analysis to measure daily usage of conventional and emerging illicit drugs at an annual music festival | Drug and Alcohol Review | Experimental | To use wastewater analysis to measure and compare use of illicit drugs at an annual music festival. | MA was found in both years studied. A level equating to 12 doses per 1000 people in 2010 decreased to 3 doses per 1000 in 2011. | There was a significant decrease in MA use between 2010 and 2011 at this annual music festival. |
| Roche A, Pidd K, Bywood P, Freeman T |
2008 | Methamphetamine use among Australian workers and its implications for prevention | Drug and Alcohol Review | Data analysis | To examine drug consumption patterns in the Australian workforce | 4.8% of male workers and 3.0% of female workers used MA. Hospitality (9.5%), construction (5.4%), transport (5.4%) and tradespeople (6.5%) were the most common industries. | Current findings suggest that MA use is significantly more common in employed Australians than previously indicated. |
| White A, Chan GC, Quek LH, Connor JP et al |
2013 | The topography of multiple drug use among adolescent Australians: Findings from the National Drug Strategy Household Survey | Addictive Behaviours | Data analysis | To examine the degree of clustering of drug types within individuals and the extent to which demographic and psychosocial predictors are related to cluster membership. | 1% of adolescents had tried MA during their lifetime compared with 52% trying alcohol, 16% trying cigarettes and 11% trying marijuana. | There is little evidence to support large groups of adolescents using drugs such as MA. |
| Author, date | Date | Title | Journal | Study Size | Aim/research question | Results, findings | Conclusion/summary |
|---|---|---|---|---|---|---|---|
| Ali R, Marsden J, Srisurapanont M, Sunga A et al |
2010 | Methamphetamine psychosis in Australia, Philippines, and Thailand: Recommendations for acute care and clinical inpatient management | Addictive Disorders and their Treatment | 150 | To describe the management of patients with MA-induced psychosis and offer recommendations for effective treatment | 61% presented with first episode of psychosis. Most common symptoms were persecutory delusions and auditory delusions. One fifth of patients we still experiencing psychotic symptoms at discharge. | Careful use of front line sedatives such as benzodiazepines is recommended treatment along with second-generation anti-psychotics. |
| Davey J, Armstrong K, Martin P |
2014 | Results of the Queensland 2007-2012 roadside drug testing program: The prevalence of three illicit drugs | Accident | 2129 | To present an overview of roadside drug driving enforcement and detections in Queensland | 2% of roadside tests were positive for drug use in 2007. This number increased to 4% in 2012. 40% of positive results were for MA making it the most prevalent drug used after alcohol. | There is a large number of drug driving apprehensions for MA. The number of apprehensions is increasing likely due to better policing and increased number of individuals driving under the influence of this drug. |
| Fatovich DM, Davis G, Bartu A |
2012 | Morbidity associated with amphetamine-related presentations to an emergency department: A record linkage study | EMA Emergency Medicine Australasia | 138 | To examine hospitalisations in a cohort of patients presenting with an amphetamine related problem to an ED in 2005. | Most common presentation to ED was for mental disorders and injury/poisoning. | Amphetamine related presentations to ED are associated with a significant cluster of hospitalisations. |
| Gray S, Fatovich D, McCoubrie D, Daly F |
2007 | Amphetamine-related presentations to an inner-city tertiary emergency department: a prospective evaluation | Medical journal of Australia | 156 | To describe the prevalence, characteristics and outcomes of amphetamine related presentations to a tertiary hospital ED. | 57.1% of admissions were habitual users, 45.5% had been to ED for previous amphetamine related presentations. 32% arrived by ambulance, 16% arrived with police. 32% required sedation. | Amphetamine related presentations comprise of 1.2% of all ED attendances. Patients are often agitated and aggressive requiring extensive resources. |
| Kaye S, Darke S, Duflou J, McKetin R |
2008 | Using quantitative wastewater analysis to measure daily usage of conventional and emerging illicit drugs at an annual music festival | Drug and Alcohol Review | Experimental | To use wastewater analysis to measure and compare use of illicit drugs at an annual music festival. | MA was found in both years studied. A level equating to 12 doses per 1000 people in 2010 decreased to 3 doses per 1000 in 2011. | There was a significant decrease in MA use between 2010 and 2011 at this annual music festival. |
| Kinner SA, Degenhardt L |
2008 | Methamphetamine use among Australian workers and its implications for prevention | Drug and Alcohol Review | Data analysis | To examine drug consumption patterns in the Australian workforce | 4.8% of male workers and 3.0% of female workers used MA. Hospitality (9.5%), construction (5.4%), transport (5.4%) and tradespeople (6.5%) were the most common industries. | Current findings suggest that MA use is significantly more common in employed Australians than previously indicated. |
| Lappin JM, Roxburgh S, Kaye J, Chalmers G, Sara T, Dobbins L, Burns and M Farrell |
2016 | The topography of multiple drug use among adolescent Australians: Findings from the National Drug Strategy Household Survey | Addictive Behaviours | Data analysis | To examine the degree of clustering of drug types within individuals and the extent to which demographic and psychosocial predictors are related to cluster membership. | 1% of adolescents had tried MA during their lifetime compared with 52% trying alcohol, 16% trying cigarettes and 11% trying marijuana. | There is little evidence to support large groups of adolescents using drugs such as MA. |
| Lyons A, Pitts M, Grierson J |
2013 | Methamphetamine use in a nationwide online sample of older Australian HIV-positive and HIV-negative gay men | Drug and Alcohol Review | 1135 | To identify factors associated with reported MA use among older Australian gay men. | 13% of the sample reported MA use. HIV positive men reported 24% while HIV negative reported 11% | Relatively high rates of MA use were found in older HIV positive gay men. |
| McKetin RL, Degenhardt M, Shanahan AL, Baker NK, Lee and Lubman DI |
2017 | Health service utilisation attributable to methamphetamine use in Australia: Patterns, predictors and national impact. | Drug and Alcohol Review | 484 | To estimate the health service utilization attributable to MA use and its national impact. Other predictors of health service utilsation among dependent MA users were also examined. | In 2013, MA use accounted for 28,400–80,900 additional psychiatric hospital admissions and 29,700–151,800 additional emergency department presentations. |
Frequent MA use is associated with a lower use of non-acute health services and more use of higher acuity health services such as emergency departments and psychiatric hospitals. |
| McKetin R, Lubman D, Najman J, Dawe S et al |
2014 | Does methamphetamine use increase violent behaviour? Evidence from a prospective longitudinal study | Addiction | 278 | To determine whether violent behaviour increases during periods of MA use and whether this is due to MA induced psychotic symptoms | Violent behaviour was 6.2 times more likely when using MA. High levels of use were associated with a 15-fold increase in violent behaviour. | There is a dose related increase in violence during periods of MA use which is largely independent of psychotic symptoms |
| McKetin R, Kelly E |
2007 | Socio-demographic factors associated with methamphetamine treatment contact among dependent methamphetamine users in Sydney, Australia | Drug and Alcohol Review | 173 | To identify the socio-demographic factors associated with not having received treatment for MA use among dependent users. | Users who were female, born outside of Australia or full time employed were less likely to seek treatment. Users who smoked were less likely to seek treatment than those who injected. | Further research is required to understand the barriers to receiving treatment for this population of drug users. |
| McKetin R, Kelly E, McLaren J |
2006 | The relationship between crystalline methamphetamine use and methamphetamine dependence | Drug and Alcohol Dependence | 309 | Is crystal MA more addictive than other forms of MA and can this be attributed to their drug use history? | 61% of users of crystal MA were dependent compared with 39% who used other forms of MA. 67% of injecting users were dependent and 58% of smoking users were addicted compared with 36% of oral/nasal users | Users of crystal MA are more likely to be dependant than those who use other forms of the drug. Users who inject or smoke are also more likely to be dependant |
| McKetin R, Lubman DI, Baker AL, Dawe S et al |
2013 | Dose-related psychotic symptoms in chronic methamphetamine users: Evidence from a prospective longitudinal study | JAMA Psychiatry | 278 | To determine the change in the probability of psychotic symptoms occurring during periods of MA use. | Likelihood of psychotic symptoms was 5 times higher during periods of MA use. This is further increased with frequent cannabis and alcohol use. | There is a large dose dependent increase in risk of psychotic symptoms during periods of MA use. |
| McKetin R, Ross J, Kelly E, Baker A et al |
2008 | Characteristics and harms associated with injecting versus smoking methamphetamine among methamphetamine treatment entrants | Drug and Alcohol Review | 400 | To compare the harms and characteristics associated with injecting and smoking MA among users entering treatment | Smokers of MA rarely injected. They were more likely to be female and use ecstasy rather than heroin when compared. There is no significant difference in mental health status between the two groups. | Smoking MA was associated with lower levels of dependency but more regular use and similar levels of harm when compared with injecting users. |
| McKetin R, McLaren J, Lubman DI, Hides L |
2006 | The prevalence of psychotic symptoms among methamphetamine users | Addiction | 309 | To examine the prevalence of psychotic symptoms among regular MA users | 13% of users experienced a psychotic episode on the past year. 23% had experienced symptoms of psychosis. Dependent users were more likely to experience psychotic symptoms. | Rates of psychosis are 11 times higher in MA users than the general population and dependant users are at higher risk than non-dependant users |
| O'Neill TB, Rawlins JM, Rea S, Wood FM |
2011 | Methamphetamine laboratory-related burns in Western Australia - Why the explosion? | Burns | 9 | To describe the mechanism of burns seen in MA production, pattern of injury and difficulties treating patients. | 9 patients were treated over the study period. All were male, with burns varying from 1%-40% TBSA. Injuries were both chemical and thermal in nature. | Patient management is complex and requires substantial analgesic, anxiolytic medication in conjunction with clinical psychology and psychiatry as an inpatient. |
| Paratz ED, Zhao J, Sherwen AK, Scarlato RM, and MacIsaac AI |
2016 | Is an Abnormal ECG Just the Tip of the ICE-berg? Examining the Utility of Electrocardiography in Detecting Methamphetamine-Induced Cardiac Pathology. | Heart Lung and Circulation | 212 | To determine the frequency and severity of ECG abnormalities amongst MA users upon hospital presentation compared to a control group. | ECG abnormalities are significantly more common in MA users (71.7%) than age and gender matched controls (32.1%). Specific abnormalities that were significantly more common were: tachyarrhythmias, right axis deviation, left ventricular hypertrophy, p pulmonale pattern, inferior Q waves, lateral T wave inversion, and longer QTc interval. | Due to the high frequency of abnormalities, ECGs should be performed in all MA users who present to hospital as well as undergoing further cardiac investigations. |
| Pennay AR, Jenkinson B, Quinn NT, Droste A, Peacock, Lubman DI and Miller PG |
2017 | Investigating Differences Between Drugs Used in the Australian Night-Time Economy: Demographics, Substance Use, and Harm. | Substance Use and Misuse | 6,984 | To investigate the correlates of drugs used in the Australian night-time economy (NTE) relating to demographics, alcohol use and experience of harm. | MA was the third most commonly self-reported substance use on the night of survey (2.6%), compared with ecstasy (4.0%) cannabis (2.9%), and cocaine (1.6%). Those reporting MA use were 1.6 times more likely than non-MA users to have been involved in physical aggression around licenced venues in the past 3 months. | MA users were more likely to interviewed later in the night (1am or later), to have engaged in pre-drinking behaviour and to have been engaged in physical aggression recently. |
| Quinn B, Stoove M, Papanastasiou C, Dietze P |
2013 | Methamphetamine use in Melbourne, Australia: Baseline characteristics of a prospective methamphetamine-using cohort and correlates of methamphetamine dependence | Journal of Substance Use | 255 | To describe the baseline health, social and drug using characteristics of a sample of community based MA users and examine the relationship between these characteristics and MA dependence. | Use of MA is seen in mainly in 30 year old users, 74% unemployed and 64% male. Main source of MA is speed (63%) and mostly injected (62%). Half of users have also used heroin in the last month. | The sample of regular MA users in Melbourne generally resembles that found in other Australian jurisdictions. |
| Wallace C, Galloway T, McKetin R, Kelly E et al |
2009 | Methamphetamine use, dependence and treatment access in rural and regional North Coast of New South Wales, Australia | Drug and Alcohol Review | 140 | To identify the socio-demographic, health, drug use patterns, treatment coverage and barriers to treatment among regular MA users in rural and regional NSW | MA use is mostly by men in their mid-30's who are unemployed with a low level of education and a history of injecting drug use. | MA users in rural and regional areas require treatment tailored to their needs due to unique stresses of rural and regional living. |
Discussion
Demographics of methamphetamine users
Seven articles described the demographics of methamphetamine users as a whole (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al; 2013; Al-Obaidi and Fletcher, 2014; Lappin et al, 2016; Paratz et al, 2016). These articles reported that the average age of methamphetamine users was range of ages from 26.5–34 years, although one paper simply reported the median age to be <40 years (Lappin et al, 2016). The majority of users were male; however, the proportion varied considerably between studies from 57–76% (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher, 2014; Lappin et al, 2016; Paratz et al, 2016). Unemployment was high, and equally variable between 52–85.6% (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher, 2014; Lappin et al, 2016). The majority of users were Australian born (80–87%), and almost all users spoke English as their language of choice (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher; 2014). Few users had finished high school education, with the average years of completed schooling in all studies being 10 years (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher; 2014) Some form of tertiary education was completed by 46% of users while 6–11% had completed a university degree (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher, 2014). Rates of dependence also varied between 45.6–60% (McKetin et al, 2006a; 2006b; Degenhardt et al, 2008; Quinn et al, 2013; Al-Obaidi and Fletcher, 2014; Lappin et al, 2016).
A number of articles sampled specific populations and their methamphetamine use. These specific populations show unique differences in particular areas of Australia. Wallace et al's study showed rural and regional users have a higher median age and a higher rate of homelessness than the other studies (Wallace et al, 2009). Roche et al's study of employed methamphetamine users showed that employed users were more likely to be younger, between 18-29 years of age (Roche et al, 2008). Another paper showed users of ecstasy who also used methamphetamine were more likely to be employed and be younger than those who primarily used methamphetamine (Kinner and Degenhardt, 2008).
Dependent users showed a number of unique statistics that differ from the general population. Four articles looked specifically at groups of methamphetamine dependent individuals. These articles showed a narrower age range of between 30–31.7 (McKetin and Kelly, 2007; McKetin et al, 2008; McKetin et al, 2013; McKetin et al, 2014). These individuals showed slightly higher unemployment rates of between 66–81% (McKetin and Kelly, 2007; McKetin et al, 2008; McKetin et al, 2013; McKetin et al, 2014). Interestingly, they had similar rates of education at both secondary and tertiary levels (McKetin and Kelly, 2007; McKetin et al, 2008; McKetin et al, 2013; McKetin et al, 2014). Periods of homelessness in the last 12 months were significantly higher in dependent methamphetamine users; 40% compared with non-dependent users at 29% (Quinn et al, 2013).
As a summary, most studies agree on a few key points. Users of methamphetamine in Australia are mostly male, aged late twenties to early thirties and born in Australia. They generally have a low level of education, high levels of unemployment and homelessness, and a high rate of dependence on the drug.
Changes in methamphetamine use
Gross rates of methamphetamine use have not changed significantly over the past 10 years (AIHW, 2013). The National Household drug survey describes use as being stable from 2010 to 2013 at approximately 2.1% of the population (AIHW 2013). Degenhart et al's paper indicates that rates of methamphetamine use have been stable at 2–3% since as far back as 1993 (Degenhardt et al, 2008). However, there has been a change in the form of methamphetamine being used, specifically in those users who inject the drug (Stafford and Breen, 2016). In 2005, 60% of users were taking speed, 39% were taking base and 43% were using crystal methamphetamine. In 2015, this changed significantly to 25% using speed, 10% using base and 67% using crystal methamphetamine (Stafford and Breen, 2016). This change in user habits has been verified by other reports (Degenhardt et al, 2008). These studies clearly indicated that while overall rates of methamphetamine usage have not changed, the proportion of users taking stronger forms of the substance has increased dramatically. Users of crystal methamphetamine typically demonstrate a higher prevalence of negative mental and physical sequelae than users of other forms of methamphetamine (Lappin et al, 2016; Degenhardt et al, 2017). This may be a contributing factor in the increased media attention recently; however, none of the studies specifically mentioned this link.
Health issues associated with methamphetamine use
An increasing number of individuals are using higher potency crystal methamphetamine compared with powdered methamphetamine and this has been associated with an increase in methamphetamine-related harms (Degenhardt et al, 2017). This is illustrated by a concomitant increase in related drug helpline calls, arrests, hospital admissions and treatment (Degenhardt et al, 2017). In 2013 alone, methamphetamine accounted for an extra 29 700–151 800 presentations to Australian emergency departments (McKetin et al, 2017).
A number of different health issues related to methamphetamine have been identified. Electrocardiograph abnormalities are more common in methamphetamine users (71.7%) than matched controls (32.1%). The drug may also cause other cardiac conditions such as cardiotoxicity, cardiomegaly, coronary vasospasm and aortic dissection (Darke et al, 2008). McKetin et al's paper on associated harms between injecting and smoking methamphetamine users showed that HIV is common in both of these populations (McKetin et al, 2008). It was shown that almost a quarter of injecting users shared or borrowed used needles and similar rates of unprotected casual sex were seen in this population (McKetin et al, 2008). While smoking, users did not experience the risk of infection from needle sharing, they did have significantly higher rates of unprotected sex (McKetin et al, 2008). Roche et al showed that rates of absenteeism in the workforce were significantly greater in methamphetamine users than any other illicit drug users. This trend was seen for injury and illness directly associated to drug use as well as unrelated illnesses (Roche et al, 2008).
Mental health issues are a significant harm linked to methamphetamine use and this was shown across a variety of the studies. Self-reported psychotic illness has a higher prevalence in crystal methamphetamine users (12.0%) compared with users of other forms of methamphetamine (3.9%) (Lappin et al, 2016). In 2013, methamphetamine was responsible for an extra 28 400–80 900 admissions to psychiatric hospitals (McKetin et al, 2017). Wallace et al showed that 43% of non-dependent and 80% of dependent users suffered from a mental disability (Wallace et al, 2009). Quinn et al showed 58% of users had sought professional help from mental health services and 42% were also currently prescribed medications for their mental illness (Quinn et al, 2013). McKetin et al stated that psychosis was common among dependent drug users with 27% experiencing clinically significant episodes (McKetin et al, 2006b). This study also excluded those who had a pre-existing psychiatric condition, thereby indicating the episodes were directly linked to the use of methamphetamine (35). Methamphetamine use in the context of mental health in ageing was explored in a 2015 study. With consideration of the aging population and the prevalence of methamphetamine use, the authors discussed potential challenges for healthcare of the aged in the future. These challenges included chronic neurophysiological and psychiatric conditions as well as issues regarding healthcare for those with a positive immunodeficiency virus status (Searby, 2015).
Causes of death linked to methamphetamine use were identified in a number of studies. Kaye et al released a study specifically focused on fatalities related to methamphetamine use (Kaye et al, 2008). This study identified that in almost all fatalities multiple drugs were used, the most common of which were benzodiazepines and morphine. Almost all deaths were accidental with only 14% being determined to be suicide. The majority of fatalities could be directly attributed to methamphetamine toxicity. Roxburgh and Burns (2015) reported on methamphetamine-related drug deaths in Australia in 2011. The rate of methamphetamine-related deaths for those aged 15–54 years was 8.1 per million persons, which was an increase from 7.1 in the previous year, with a projected increase in this rate for subsequent years. Fatovich, Davis and Bartu noted four deaths in their study of hospitalisations related to amphetamine use (Fatovich et al, 2012). The causes were due to drug toxicity, cardiomegaly, seizure disorder, and the final death was due to multiple organ failure secondary to pneumonia.
Pre-hospital and emergency presentations of methamphetamine use
Hospital presentations from methamphetamine use have increased in recent years and this is linked to a number of issues unique to methamphetamines (Stafford and Breen, 2016). Gray et al showed in 2007 that 1.2% of the workload of Royal Perth Hospital was causally related to amphetamine use (Gray et al, 2007). The most common reason for admission to hospital was agitated delirium and psychosis, followed by assault and other injury. These patients were often aggressive and 32% of the patients included in the study required sedation. A study by Fatovich, Davis and Bartu likewise found that mental disorders were the foremost reason for admission to hospital (Fatovich et al, 2012). This was followed by injury and poisoning, which mirrors Gray et al's findings. An article written by O'Neill, Rawlins and Wood outlined the dangers of methamphetamine lab explosions (O'Neill et al, 2011). While this was a small population, 9 patients over a 12-month period, it gave some important insights into patient behaviour in hospital. The study showed over half of the patients were discharged early due to threatening and antisocial behaviour which was compromising safety of hospital staff. This validates and highlights the findings from Gray et al that methamphetamine cases in hospital are associated with high rates of sedation (Gray et al, 2007). Ali et al similarly recommended judicious use of sedatives as a first line treatment for psychosis for methamphetamine users (Ali et al, 2010).
Conclusions
Methamphetamine use is a growing concern to the emergency healthcare industry. While overall rates of use haven't changed significantly over the past decade, the type of methamphetamine being used has changed towards the purer crystal methamphetamine. The number of hospital admissions and ambulance attendances has increased, likely due to the purer form of drug and adverse effects associated with it. Some research has been undertaken in this field; however, there are yet to be any paramedic-led studies. The related physical and mental health issues associated with methamphetamine use, coupled with the increasing hospital and ambulance utilisation by this population, warrant more research being undertaken on this issue.
