Every 3 seconds, somebody in the World dies from sepsis (Hall et al, 2011), and with research suggesting sepsis has a mortality rate 5–6 times higher than acute coronary syndrome or stroke (Daniels, 2011), it is easy to see why sepsis is one of the leading causes of death in the World (McPherson et al, 2013). There is a multitude of reasons for the high mortality of sepsis (Martin, 2012); however, it appears poor recognition and delays to antimicrobial therapy remain the biggest factors (Puskarich et al, 2011).
The UK Sepsis Trust has published guidelines based on contemporary evidence relating to the early recognition and management of sepsis. These guidelines highlight the importance of obtaining serial lactate as part of the sepsis six (Daniels, 2011). Obtaining an early lactate value allows the clinician to stratify the risk to the patient; this is of particular value in sepsis where cryptic shock is prevalent, meaning blood pressure may be an unreliable means of measuring hypoperfusion (Kirby, 2013). Cryptic shock is where patients in septic shock have global tissue hypoxia, but maintain normotension (Puskarich, 2011). Previous literature reviews have highlighted the paucity of research in the pre-hospital field evaluating point-of-care (POC) lactate testing (McClelland et al, 2012; Kirby, 2013; Charlton, 2014). A lack of evidence to inform the pre-hospital phase of care for patients with suspected sepsis prompted this evaluation of POC lactate measurement in an ambulance service.
Sepsis prior to Sepsis-3 was defined as a clinical syndrome characterised by the presence of both infection and a systemic inflammatory response. Sepsis may result in organ dysfunction, shock and death (Wang et al, 2010). Since February 2016, septic shock is defined as a subset of sepsis where there are profound circulatory, cellular and metabolic abnormalities associated with a greater risk of mortality than sepsis alone (Singer et al, 2016).
At the time of this study, sepsis was recognised using the severe inflammatory response syndrome (SIRS) criteria. Sepsis was indicated where a patient is suspected of having an infection, and, physiological parameters indicate two or more of the following:
Since this study completed a new consensus on defining sepsis and clinical criteria to recognise sepsis, Sepsis-3, has been published (Singer et al, 2016).
Aims and Objectives
Methods
A small ambulance station within South Western Ambulance Service NHS Foundation Trust (SWAST) was purposively selected to participate in the study based on its size, location, usual patient numbers and staffing profile. Staff eligible to participate were paramedics and technicians.
Of the 34 staff members based at the ambulance station, a total of 23 participated in the study. Participating staff were trained in the use of a commercially available point-of-care, capillary lactate monitor, prior to the start of the study. The training was delivered by a member of the Trust's training team alongside an expert in the use of the device from the commercial provider of the device. One training session was provided for the staff based at the participating ambulance station. The training session consisted of a device specific element in addition to an update on the recognition and management of sepsis. Training focused on obtaining reliable capillary blood samples and use of the device. Staff unable to attend the training day were offered one-to-one sessions by ambulance officers trained in the use of the device, or by a member of the research team. During training, staff were informed of the data recording and reporting process. This required staff to record the lactate value on the patient clinical record (PCR) form and to complete a case record form (CRF). The case record could be completed retrospectively, and required the clinician to document the reasoning behind using the device, the lactate result and any problems encountered. Clinicians were advised that a lactate of >2mmol may indicate severe sepsis and >4mmol septic shock. As clinicians were only using the lactate monitor in patients they suspected as having sepsis, they were advised to convey patients to ED where a lactate of >2mmol was recorded.
The study took part over a six-month period, from 01 April 2014 until 30 September 2014. CRFs were collected for the whole study period.
A data collection period of one month was pre-specified for the fifth month of the study (August 2014). The methodology of only collecting one month's data was used due to the absence of funding and to allow the lactate monitor to be established in practice before data collection. During the data collection period PCRs were reviewed where there was the presence of an infection and there was evidence of 2 or more SIRS criteria. These PCRs were cross-referenced with the CRFs. Reviewing the relevant PCRs for a one month period aimed to capture those instances where a lactate monitor had been used but its use not recorded on a study specific CRF.
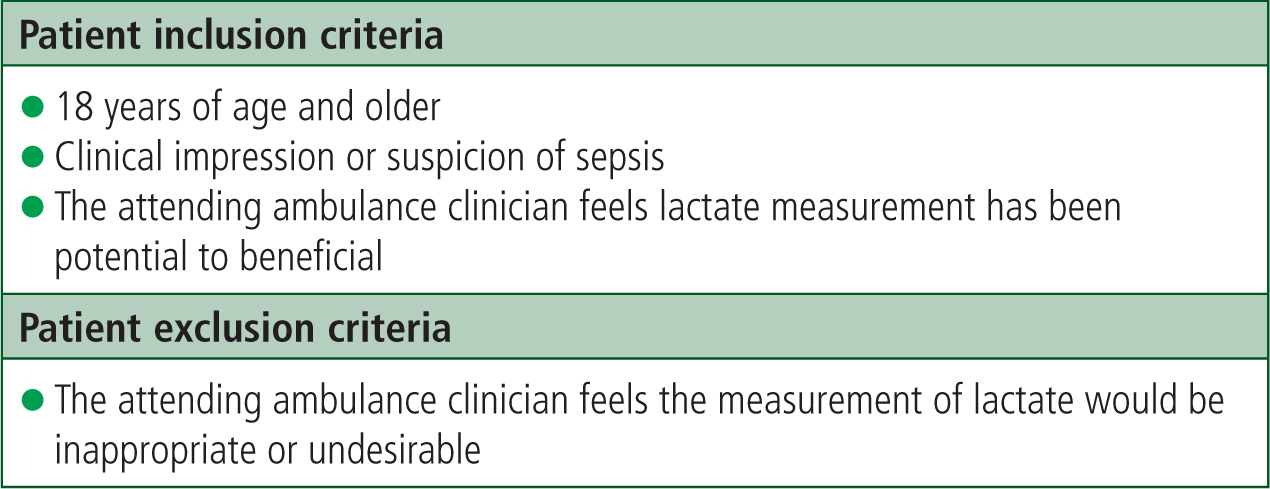
The study design was a pragmatic evaluation to reflect the “real-life” introduction of new equipment and practices into the ambulance service. The inclusion criteria were intentionally broad and are illustrated in figure 1.
A local data-sharing agreement had been established previously between ambulance stations in the region and a local Emergency Department (ED). This agreement provided patient outcome data from the ED to ambulance clinicians.
Results
During the data collection period the participating ambulance station returned 585 PCRs. A total of 47 patients had both SIRS x 2 and a documented infection and an indication to obtain a pre-hospital lactate reading. Of the 47 patients where a lactate measurement was indicated, a lactate reading was taken and documented in 6 out of 47 patients (12.7%). In the 6 cases where a lactate value was obtained appropriately and documented, the pre-hospital lactate ranged from 1.5 – 7.5 mmol/L, with a mean of 4.0 mmol/L (see table 1). Of these 6 patients, only two had subsequent lactate values recorded in the ED. One patient met the SIRS x 2 plus infection criteria and had a lactate >2mmol and was not conveyed to hospital.
| Pre-hospital Lactate Values Taken (Infection present and SIRS x 2) - August 2014 | |
|---|---|
| Prehospital Lactate (mmol/L) | Hospital Lactate (mmol/L) |
| 2.9 | Direct to MAU* |
| 6.8 | 2.1 |
| 2.6 | Not Conveyed |
| 2.5 | Not Recorded |
| 7.5 | Not Recorded |
| 1.5 | 2.2 |
| Pre-hospital Lactate Values Taken (no infection present and no SIRS x 2) | |
| 0.7 | Not Recorded |
| 1.9 | Not Recorded |
There were a further 2 incidents during the data collection period where a lactate measurement was recorded but sepsis was not identified according to the UK Sepsis Trust Prehospital Screening and Action Tool (2014).
Table one shows the instances during the data collection period, where a pre-hospital lactate reading was obtained.
There was an incident during the 6 month study period where a lactate monitor was mistaken for a blood glucose monitor and the lactate reading was thought to have been a low blood glucose reading. This incident did not compromise patient care, and immediate action was taken to ensure that the lactate monitors were given a clear label to mitigate any future confusion.
Discussion
This evaluation sought to determine the feasibility of using a commercially available lactate device in the detection of septic shock. This was a small pragmatic study, which aimed to evaluate the use of testing in as close to routine clinical practice as was possible; no statistically significant results were sought. The results of the study indicate that the lactate monitor was used in only 6 of 47(12.7%) cases where a pre-hospital lactate reading was indicated, according to the UK Sepsis Trust (2014).
The reasons for the low levels of device utilisation in potentially eligible patients is not clear. Possible factors could include:
Follow up exploration of these factors with staff may help to identify reasons for the low-utilisation rates of the device during the study period.
On the two occasions where pre-hospital and in-hospital values were available for comparison, there does appear to be a difference between values. There are many potential causes for a change in lactate value between pre-hospital measurement and ED measurement. Any treatment causing an improvement in hypoperfusion could cause a reduction in lactate; this is particularly pertinent in this study as a time delay existed between pre-hospital and in-hospital lactate readings, providing additional time for treatment to take effect. It is also worth noting that pre-hospital values were obtained from a capillary sample, whereas hospital values were obtained from venous or arterial samples. Previous pre-hospital research investigating venous and capillary samples obtained pre-hospital has revealed that capillary samples are associated with a higher lactate value (Younger and McClelland, 2014).
Limitations
This study was a small evaluation with no external funding.
There are likely to have been occasions where the device was used but not recorded on the PCR or a CRF completed, and therefore not included in the study.
Relief and bank staff working at the ambulance station during the study period have not been taken into account in the analysis.
There is a clear need for further qualitative work to understand the experiences of staff when using the devices.
Conclusions
In this evaluation, a commercially available, point of care, lactate testing device was used in a limited number of the potentially eligible cases.
Limited documented use of the device meant that potential alterations to the patient's management could not be assessed. It is not clear from the study findings whether the clinicians using the device considered it acceptable and further work to explore this is indicated. The device was underused during the study period, and this meant that it was not possible to demonstrate the usefulness of prehospital point of care lactate testing in identifying septic shock. The underuse of the device requires further exploration to establish if this study has highlighted a training need for ambulance clinicans in the recognition of sepsis.
