
Since April 2018, paramedics have been able to train as independent prescribers. Independent prescribing is prescribing by a paramedic who is responsible and accountable for the assessment of people who use their services, who have an undiagnosed or diagnosed condition and for whom decisions about the clinical management are needed. Independent prescribers are able to prescribe on their own initiative any medicine within their scope of practice and in line with legislation.
Supplementary prescribing is a voluntary partnership between a doctor and supplementary prescriber to prescribe within an agreed clinical management plan (CMP) that is specific to the service user. Once qualified, a supplementary prescriber may prescribe any medicine within their clinical competence within the limits of the CMP (Royal Pharmaceutical Society (RPS), 2016; Health and Care Professionals Council (HCPC), 2019).
This article introduces the forthcoming series on pharmacology aimed at the aspiring paramedic prescriber. The series will also be of interest to paramedics and student paramedics.
Pharmacology
Pharmacology is a key component of undergraduate paramedic programmes. The HCPC (2014) and the College of Paramedics (CoP, 2019) curriculum guidance include pharmacology explicitly in standards and guidance.
At the point of registration, the paramedic is required to demonstrate proficiency in several areas (Box 1).
Paramedic development
Roles continue to emerge in all healthcare professions, including paramedic practice. These roles are evolving rapidly, and demand higher levels of critical thinking and clinical decision-making.
The prehospital care role continues to widen. Students are being prepared to take on advanced roles, as well as to be ‘prescribing-ready’ upon registration.
Registered paramedics are required to undertake continuing professional development (CPD). The HCPC (2018) defines CPD as ‘a range of learning activities through which health professionals maintain and develop throughout their career to ensure that they retain their capacity to practice safely, effectively and legally within their evolving scope of practice’.
CPD, in its many forms, provides the paramedic with opportunities and requirements to continue to learn and develop as lifelong learners, enabling them to keep their skills and knowledge up to date so as to practise safely, effectively and within the law.
Paramedic independent prescribing
While all student paramedics have to undertake a programme of study that considers pharmacology, paramedics are not required to undertake a programme to become independent prescribers. The safety of patients is key and the strict eligibility criteria for admission onto a prescribing education programme reflect this.
NHS England (2020) sets out the requirements that must be met to be able to train as non-medical independent prescribers.
All paramedic entrants have to meet the following:
Service check within the previous 3 years. Currently, four allied health professional professions have been given prescribing responsibilities (independent and supplementary prescribing):
Prescribing requires an additional HCPC annotation. Only programmes that have been approved by the HCPC can provide eligibility for this annotation. A paramedic may only practise as a prescriber if they have completed HCPC-approved training and have an annotation on the register to demonstrate that they have completed that training.
The overall aim of any non-medical prescribing programme is to make sure the paramedic is ready for a role as an independent prescriber.
The Allied Health Professions Federation (AHPF) (2018) has provided an outline curriculum framework for education programmes that prepare the paramedic to be an independent/supplementary prescriber. This outline curriculum framework document is intended for education providers who aim to develop programmes and individuals interested in education programmes for paramedics to fulfil the requirements for annotation on the HCPC register as both independent and supplementary prescribers.
Independent prescribing is a key element of NHS modernisation and is intended to extend practice beyond traditional professional boundaries, making better use of professional skills (Department of Health and Social Care (DHSC), 2006). The advantages to patient care from non-medical prescribing are significant—it improves patient-centred care, gives prompt access to treatment and increases patient choice without compromising safety (DHSC 2005; 2006). Prehospital urgent care plays a significant role in the NHS Long Term Plan (NHS, 2019) and prescribing as part of advanced practice is a key component of the plan.
Prescribing standards
The HCPC Standards for Prescribing (HCPC, 2019) use A Competency Framework for all Prescribers published and maintained by the RPS (RPS, 2016). The standards, which are for all prescribers, set out the knowledge, understanding and skills that the paramedic must have when they complete their prescribing training and which they must continue to meet once in practice.
The standards set out safe and effective prescribing practice and are the threshold standards considered necessary by the HCPC to protect members of the public. While the standards use numbers to identify each standard, this is for ease of access. They are not hierarchical—they are all equally important for practice.
Paramedic independent prescribers can prescribe any licensed medicine from the British National Formulary. They must do this within national and local guidelines for any condition within the practitioner's area of expertise and competence within the overarching framework of planned, unscheduled and/or undifferentiated care for patients across a range of practice settings (AHPF, 2018).
Paramedics must work only within their scope of practice. If a paramedic extends their role to a new area—a new sphere of practice—they are required to show that they are competent in that area.
New pharmacology series
The Journal of Paramedic Practice has commissioned a pharmacology series to be published over the next year. Contributors to the series are paramedics and academics.
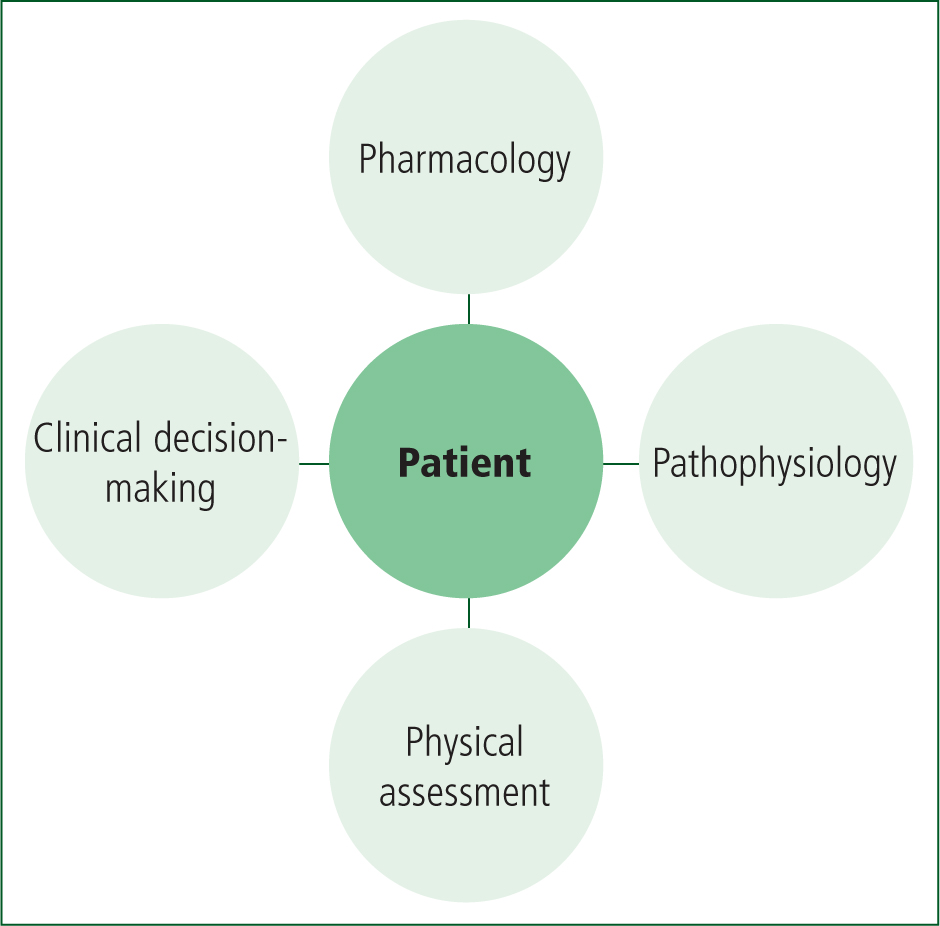
Programmes of education develop the paramedic's key clinical knowledge and skills through the study of pharmacology, pathophysiology, physical assessment skills and clinical decision-making. Figure 1 shows these component parts with the patient at the centre of all that is done.
The aim of any paramedic programme is to ensure the integration and application of theory and practice to produce an adaptable, innovative paramedic who is able to demonstrate excellent professional skills, using a research-based, evaluative, problem-solving approach to clinical practice. Paramedics need to be equipped with the skills that will enable them to be lifelong learners and to embrace technology and technology-enhanced learning, as IT is key in any contemporary healthcare system.
The Journal of Paramedic Practice series on pharmacology has been designed to provide the paramedic with:
This new, easy-to-read series will feature the most relevant topics to paramedics who are new to non-medical prescribing, both registered and student paramedics. It will be applied clearly to real-world practice, and be easy to digest, concise and written in plain language in an engaging tone.
The themes addressed in the series are shown in Box 2. The series is being launched in the current issue with an article on evidence-based prescribing (p. 10–13), followed by an article outside the series on p. 14–23 about whether paramedic prescribing is being practised as was expected.
Each of the subjects in Box 2 begins with an introduction to the topic area along with a rationale as to why this area is an important one. The body of the article outlines the context and draws on an evidence base with regards as to how to manage specific issues being discussed. Patient vignettes are used to relate the theory to practice and to aid recall. Each article ends with a conclusion emphasising what this means for patient care and the paramedic.
Conclusion
Independent prescribing by paramedics has the potential to enable new roles and ways of working to improve service quality and delivery of safe, effective services focused on the patient experience. It also facilitates partnership working across professional and organisational boundaries, redesigning care pathways that are cost-effective and sustainable. Independent prescribing can enhance choice and competition, maximising benefits for patients.

