The COVID-19 pandemic has placed the UK NHS under considerable stress (NHS Providers and Association of Ambulance Chief Executives (AACE), 2021). One consequence of delivering the frontline response was the reduced capacity of UK emergency medical service (EMS) ambulance organisations to provide practical placement opportunities for undergraduate paramedic students (Council of Deans of Health, 2020). Physical distancing requirements (Sørensen et al, 2021) prevented many students from undertaking ‘on-the-road’ ambulance shifts, compromising their learning experience. To ensure that paramedic students received the training required to meet course objectives, a large NHS EMS organisation in South West England secured funding from Health Education England (HEE) to explore whether virtual reality (VR) technology could bridge the gap.
VR has been defined in a number of ways depending upon context, the level of immersion, and the methods used to simulate experiences without the student going through the real event. This article discusses the use of three-dimensional (3D) VR methods for simulating prehospital emergency ambulance scenarios. A range of scenarios delivered through a head-mounted display, accompanied by lights, sounds and smells, produced a medium-to-high immersive experience for students (Kardong-Edgren et al, 2019).
Bradley (2006), and van Merriënboer and Kirschner (2017), suggest that simulation is a useful adjunct to learning, providing the learner with a safe environment where they have more control over their experience. Gaba (2004: i2) describes simulation as a technique used ‘to replace or amplify real experiences with guided experiences, often immersive in nature, that evoke or replicate substantial aspects of the real world in a fully interactive fashion’. Gaba's vision both predates and predicts the advent of accessible VR technology. Scenarios using VR have the benefit of increased opportunity for student support and guidance compared with what may be available during the emergency demand and time constraints of a traditional ambulance shift (Radianti et al, 2020). VR also creates the opportunity for students to undertake tasks and decision-making relating to rare patient illness and injury, that may not be encountered during traditional placements and would otherwise be impossible to experience due to limited resources or materials (Fromm et al, 2021).
Planning
Using the Plan, Do, Study, Act (PDSA) improvement cycle, the Trust's in-house technology enhanced learning (TEL) team created scenarios using the XVR ‘on scene’ platform (XVR Simulation B.V, 2022). Ongoing collaboration and support from in-house learning and development (L&D) and information and communication technology (ICT) teams ensured that the scenarios met course objectives and student needs. Scenarios were created by mapping learning outcomes from two universities in south west England, relating to year one paramedic science BSc syllabus objectives, against activities that can be achieved using VR. The mapping process was undertaken by paramedic course tutors and was underpinned by learning taxonomies and Biggs' (2003) model of Constructive Alignment in Curriculum design (Anderson et al, 2001; Appendix 1). Given the restrictions placed on EMS estates by COVID-19 safety guidelines, external venues were sourced that maximised the safety of students and faculty. The sessions covered the following subjects as mapped out during planning;

Scenarios
During Spring 2021, when COVID-19 physical distancing restrictions prevented students from undertaking traditional ambulance shifts, undergraduate paramedic students were invited in groups of up to 12 to undertake classroom-based training where practical scenarios were completed using simulations played through VR. The students worked in pairs; one wore a headset and navigated their way through the simulation, while the other could view what their partner was seeing through a headset attached to a laptop screen. The students could move around the virtual environment scenario at their own pace and decide whether it was safe to approach and what action to take. For example, during the mass casualty scenario, students chose in which order to approach patients based upon the visual and audible information provided in the virtual environment. However, the ability to manipulate and interact with the scenarios was limited and the simulated patient outcomes would eventually be the same for each student.
Psychological safety
To maintain psychological safety and maximise the learning opportunities, each session included structured one-to-one debriefings between the student and the L&D tutor. This was followed by a whole group discussion framed by Guirguis and Cox's (2007) Advocacy-Inquiry method, which includes:
Evidence suggests that psychological distress can occur when participants are exposed to simulation-based experiences (Fanning and Gaba, 2007; Kolbe et al, 2020). Factors such as exposure of knowledge gaps and performance anxiety in front of peers, combined with risk of recall of traumatic memories, can cause distress and result in a negative impact upon learning (Henricksen et al, 2017). Psychological preparation and support was vital for minimising any psychological distress and for enabling simulation-based education participants to learn safely (Palaganas et al, 2014).
Student feedback
It is usual business for participant/learner feedback to be collected following any L&D activity in the Trust. Under the terms of reference of the Trust's research and development department, ethical approval is not required when anonymous feedback is publicly reported. The feedback garnered following education using VR was particularly interesting, as the use of VR was novel under the circumstances. At the end of each session, students were asked to provide written feedback using internal feedback forms relating to how they felt about the learning experience. During April and May 2021, 60 undergraduate BSc paramedic science students participated in one day of ambulance scenarios using VR in the Plymouth area of the UK and 53 students undertook two half-day simulated ambulance scenarios using VR in the Gloucestershire area. There were 36 students in Plymouth and 17 students in Gloucester who provided feedback giving a response rate of 60% and 32%, respectively. Students provided free-text comments in response to five questions about the quality of the content of the learning, the quality of the tutors (such as their ability to provide clear, inclusive and supportive sessions (van Dijk et al, 2020)), whether they felt VR was a suitable platform for learning, and whether they felt they had achieved the learning outcomes as required in their undergraduate course portfolio.
Feedback summary
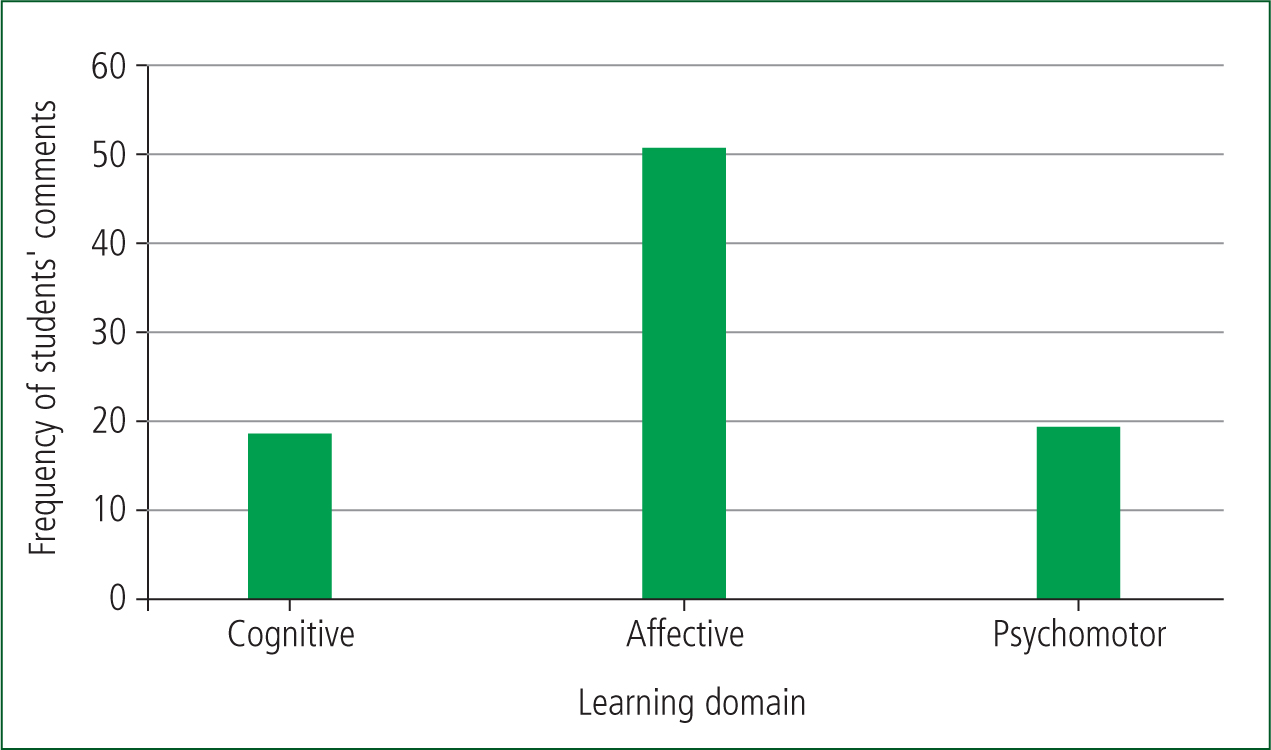
Feedback from across the two sites was examined using content analysis. Eighty-eight nodes, systematically generated from the feedback provided by 53 students, were reduced to 14 categories, which in turn were condensed into nine themes relating to three domains of learning. An overarching theme of ‘enthusiasm for VR learning’ was identified. Three domains of learning; cognitive, affective, and psychomotor formed the conduit into which nine themes of ‘knowledge’, ‘personal development’, ‘experience’, ‘confidence’, ‘future learning’, ‘tutor interaction’, ‘lost placement hours’, ‘scenarios’, and ‘road versus academic learning’ were identified. The nine themes were distilled into the three domains of learning and quantified by the frequency of comments relating to each domain (Figure 1). Simulation-based learning using VR appears to relate more closely to the affective domain of learning.
Overall, students reported positive perceptions of the learning content, quality, and suitability of VR as a learning platform. The majority of students reported that although scenarios through VR were useful, they were not a substitute for the real-world experience of a traditional ambulance shift. The opportunity to put classroom-based theory into practice was welcomed and most reported that the VR experience not only helped to increase their knowledge, but also boosted their confidence. However, some reported that the VR approach did not suit their learning style and the quality of the equipment and simulations at the time hampered the learning experience. Nonetheless, when compared to practical classroom-based scenarios in university settings, overall, students preferred a VR approach.
Discussion
Scenarios using VR appear to be acceptable to undergraduate paramedic students as part of their training, although VR is not a substitute for the real experience. This information is important for COVID-19 pandemic contingency planning, where hours spent ‘on the road’ undertaking practical ambulance placements may be reduced to ensure student, staff, and patient safety (NHS Providers and AACE, 2021). HEE (2018) published a national framework for simulation-based education and their recent guidance highlights that simulation can support key factors such as clinical effectiveness, patient safety, staff wellbeing, patient experience, quality improvement, and productivity—all of which improve outcomes for the workforce, the wider healthcare system and the patients (HEE, 2020). The VR approach appears to be particularly useful for supporting the affective domain of paramedic learning (Bloom, 1956), with several students reporting increased self-confidence, positive interactions with course facilitators, and the opportunity to put classroom knowledge into practice. Evidence suggests that paramedic confidence and mental wellbeing have been worsened by the pandemic, highlighting the importance of alternative and novel methods of confidence-building for paramedics entering the profession at this time (Hogan et al, 2020). However, a number of research studies have identified common side effects which may hamper user experience and learning when using VR technologies (Garrett et al, 2018). Due to the inconsistent sensory inputs, body systems can become conflicted when immersed in VR, leading to cybersickness (similar to motion sickness) (Palmisano et al, 2020). Cybersickness is a commonly reported side-effect, with symptoms such as nausea, vomiting, ataxia, and dizziness (Caserman et al, 2021). Training plans should include consideration of side-effect management such as dynamic depth-of-field blurring which simulates the blurring of objects located in front or back of the focus point of the eyes to minimise any negative effects (Carnegie and Rhee, 2015).
The provision of VR ambulance scenarios may enable ambulance organisations to counterbalance any inability to provide the desired practical placement hours (and the lack of exposure to patients, which can be caused by prolonged handover delays during placements) for student paramedic programmes. The incorporation of VR learning could also provide opportunities for confidence-building and learning from experience, in a safe environment. This may be particularly important for infrequently-encountered incidents that could now be replicated in VR, enabling students to gain experience where otherwise none would be had (Bailenson, 2018).
Consistent with paramedic student feedback, McKenna et al (2015) found that effective use of VR relies upon appropriate equipment as well as trained faculty. Furthermore, Watts et al (2021) emphasise that the design and content of the VR experience are important. VR equipment and delivery can be expensive. However, Pottle (2019) suggests that VR offers healthcare organisations a number of benefits and enables the delivery of practical learning experiences using fewer resources, compared with a traditional shift, at reduced costs. A recent study by Halabi et al (2022) identified that the costs of training ambulance staff in VR simulation are at least 60% less than when the same activity is performed in a real-world setting, when cost factors such as vehicles, equipment and maintenance were taken into consideration.
Infrequently encountered incidents are a challenge for all paramedics and ambulance staff, as well as students. VR provides opportunities to engage in scenarios of high-stakes, low-frequency incidents, which may increase confidence, enhance patient safety, and reduce the risk of error (Kiernan, 2018; Wheeler and Dippenaar, 2020; Wood et al, 2022).
Conclusion
Overall, the use of VR during scenarios for undergraduate paramedic students appears to be a useful and acceptable adjunct to traditional ambulance shifts. It seems particularly useful for supporting the affective domain of learning with students reporting increased self-confidence, positive interactions with course facilitators, and the opportunity to put classroom knowledge into practice. VR was a useful training aid for supporting placement gaps during COVID-19 physical distancing measures. However, VR would also be a useful addition to ambulance training programmes to supplement future learning, development, and improve the confidence of paramedic students in a safe and controlled environment.
The next steps for VR in paramedic undergraduate learning should focus on improving the quality of scenarios and the equipment used. Research is recommended to identify which areas of paramedic training would most benefit from a VR adjunct and what equipment would optimise student experience and learning.

