The Government is overwhelmingly the most influential body shaping health care in the United Kingdom (UK) (Walshe and Smith, 2006). Evidencing this, NHS England (2014) released a Sepsis Stage 2 Patient Safety Alert requiring each ambulance service to have in development a screening tool, treatment pathway and educational programme for sepsis. At the time of this release, no active sepsis pathway was being utilised within the North West Ambulance Service NHS Trust (NWAS).
Sepsis is defined as:
‘an overwhelming uncontrolled, systemic inflammatory response which is mediated by the immune system, the vascular endothelium and inflammatory pathways in response to an infective trigger’
There are 100 000 cases of sepsis each year in the UK, with 36 800 deaths attributed to sepsis (Harrison et al, 2006). Despite internationally agreed sepsis definitions (Box 1) and the introduction of the ‘Sepsis Six’ bundle of care (Box 2) as part of the ‘Surviving Sepsis Campaign’ (Dellinger et al, 2008), sepsis remains responsible for 27% of all intensive care unit beds in England and Wales (Robson et al, 2009).
Despite medical therapy advances during the last 30 years, mortality for severe sepsis remains higher than 30% (Francis et al, 2010). These high rates of mortality suggest a lot more can be done within the NHS—and subsequently NWAS—to improve care of the sepsis patient.
Background
The ‘Surviving Sepsis Campaign’ (SSC), launched in 2002, aimed to reduce sepsis attributed mortality by at least 25% (Slade et al, 2003). Compliance with a care bundle, the ‘Sepsis Six’, was shown to reduce the incidence of death by 46.6% (Daniels el al, 2011). Evidence such as this led to the Royal College of Nursing, the Intensive Care Society and the Society for Acute Medicine adopting this policy (Levy et al, 2010). Despite its re-launch in 2008, compliance with the ‘Sepsis Six’ in emergency departments was only shown to be 18%, compared to the 66% of patients that received thrombolysis for myocardial infarction from associated hospitals and ambulance services (Boardman et al, 2009). The disparity of care provided to sepsis patients has led experts to review the role of paramedics in sepsis treatment, highlighting them as a key component in improving sepsis survival rates (Robson et al, 2009; Cronshaw et al, 2011). A study by Gray et al (2013) found that 88% of patients treated in A&E for sepsis were transported by ambulance, showing a large scope to influence and improve sepsis care with early identification in the pre-hospital environment.
Hospital-based studies such as the ‘GenESIS Project’ (Generalized Early Sepsis Intervention Strategies) identified a 15% increase in the identification rate of sepsis, a 14% reduction in mortality, a 24.6% reduction in the hospital length of stay and a 33% reduction in the hospital cost per admission for each sepsis patient (Cannon et al, 2013). A lack of protocols to date in pre-hospital sepsis care was shown by Seymour et al (2010) to produce varying levels of care. In contrast, when ambulance staff report a suspicion of sepsis to hospital staff it is shown to reduce the time taken for the patient to receive an appropriate ‘bundle’ of care (Studnek et al, 2012; Robson et al, 2009). However, in confirmed cases of sepsis, the primary impression of sepsis was reported to emergency department staff only 21% of the time (Studnek et al, 2012). Guerra et al (2013) also reported sepsis is completely missed by emergency service staff 51–63% of the time prior to attending emergency department. This has a direct negative impact on the septic patient's treatment.
Within NWAS the ‘Paramedic Pathfinder Tool’ is used to aid in identifying the correct treatment pathway for patients in the pre-hospital arena (Newton et al, 2013). However, this tool, based on ‘Manchester Triage’ (Manchester Triage Group, 2005), does not specifically allow for the identification of the sepsis patient, nor does it direct the paramedic to a specific treatment protocol. Conditions such as myocardial infarction, cerebral vascular accident and major trauma are exempted from this triage tool, though protocols and education packages have addressed the recognition of these conditions and allowed paramedics to provide prompt and appropriate treatment and transport (Robson et al, 2009). This, however, leaves the patient at risk of a delayed identification of sepsis. Each hour of delay in giving antibiotics to a patient with severe sepsis has an increased mortality of 7.6% (Kumar et al, 2006). If identified early by ambulance clinicians, a subsequent reduction in time to antibiotics and an increase in compliance with the ‘Sepsis Six’ care bundle is noted in severe sepsis patients (Seymour et al, 2014).
Based on the associated risks evidenced of not identifying sepsis, why has there not been a move nationally to produce a pre-hospital sepsis screening tool and protocol?
Diagnosing sepsis has proved difficult (Robson et al, 2009). Symptoms such as fever, rapid pulse and an increased respiratory rate can frequently be confused with other conditions. A reason stated by Nguyen and Smith (2007) that no ratified guidelines exist is that pre-hospital research carried out to date is not linked to hospital records to confirm if patients transported were actually septic. A lack of research—a view supported by McClelland and Younger (2013)—is likely to be a major reason that pre-hospital sepsis tools and treatment are yet to be agreed nationally. Without a confirmation of sepsis as an end diagnosis, policy makers will remain unsure or unconvinced that the cases identified and indicated for treatment by suggested tools are actually treating septic patients.
However, more recently, research by Seymour et al (2014) has shown that pre-hospital actions based on the in-hospital protocols can affect the sepsis patient's treatment within the emergency department. Structured training including guidelines, posters, and diagnostic/treatment algorithms have been shown to improve compliance and treatment of the sepsis patient within ED (Plambech et al, 2012). There is therefore an expectation that the development of a sepsis screening tool and pilot within NWAS would reap positive patient care outcomes for sepsis patients and a potential reduction in mortality attributed to sepsis.
Methods
An initial retrospective clinical audit was completed of 259 hospital diagnosed cases of sepsis in adults conveyed by NWAS to Salford Royal Foundation Trust (SRFT) emergency department. The analysis looked at elements of sepsis care that research (covered in the discussion section) both pre- and intra-hospital suggests would amount to ‘best practice’ in the pre-hospital field (Box 3).
A clear benefit was noted if a sepsis pathway was initiated at or near a time of sepsis recognition (Jones et al, 2010). Therefore, if sepsis is identified pre-hospital, elements of the ‘Sepsis Six’ care bundle can be commenced prior to reaching hospital including fluid boluses, which have been shown to reduce the odds of developing organ failure during hospitalisation with sepsis (Seymour et al, 2014).
This therefore culminated in the development of a modified UK Sepsis Trust (2014) ‘Red Flag’ Sepsis Screening Tool for adults (see Figure 1) and a treatment pathway derived from hospital-based studies identified in literature (See Figure 2). A 2-hour sepsis training package was delivered to 100 frontline clinicians within the central Manchester pilot site. These clinicians then used the screening tool and treatment pathway to identify and treat 100 patients over 16 years of age with potential sepsis that were subsequently conveyed to SRFT or Central Manchester Foundation Trust (CMFT) emergency departments. Analysis was then completed of the patient report forms for these 100 cases, checking the screening tool had been applied correctly, comparing the treatment provided against that delivered in the retrospective audit to confirmed sepsis cases. Ethical approval and institutional support from NWAS was gained for the pilot study.


As well as analysing ‘retrospective versus prospective’ data, a further retrospective analysis of the data from SRFT was completed to see if any elements of care delivered pre-hospital were seen to affect the compliance and timeliness of delivery of the ‘Sepsis Six’ within the emergency department.
Results
The retrospective audit contained the analysis of 259 hospital confirmed cases of sepsis. When the modified screening tool was applied to the NWAS patient report form of these cases, it was found that 89% (n=236) of all sepsis cases and 90% (n=123) of severe sepsis patients were identified. The prospective audit pilot contained 100 potential cases of NWAS identified sepsis. The screening tool was applied correctly in 99% (n=99) of the cases, with only one case not meeting the sepsis criteria due to having less than two systemic inflammatory response syndrome (SIRS) markers evidenced.
In all types of sepsis, compliance with identifying and documenting the suspicion of sepsis on the patient report form in the prospective audit was evidenced in 90% (n=90) of cases, compared to 16% (n=41) in the retrospective audit. In cases of severe sepsis, retrospectively, sepsis was found to be documented in 25% (n=33) of cases, compared to 98% (n=49) in the prospective trial.
Initially, in identifying a suspicion of sepsis, current guidelines state two or more SIRS criteria must be evidenced. In the retrospective audit, the SIRS criteria were fully assessed in 90% (n=233) of cases, with blood sugar measurement not recorded on 68% (n=18) of occasions. Prospectively, compliance with fully completing the SIRS measurement increased to 98% (n=98). Furthering this, the documentation on the patient report form of a ‘suspicion of sepsis’, along with a full completion of the SIRS markers, increased from 15% (n=39) to 94% (n=94) in the prospective audit.
The greatest increase shown by the introduction of the sepsis protocol was shown in the delivery of a ‘best practice’ bundle of care to ‘Red Flag’ sepsis patients. This bundle comprised of IV access, fluid boluses, high flow oxygen, documentation of a suspicion of ‘Red Flag Sepsis’ and a pre-alert to the receiving hospital. In the retrospective audit, compliance with this sepsis bundle was 10% (n=13) in confirmed severe sepsis patients. In the prospective audit, compliance with this bundle in ‘Red Flag’ sepsis patients increased to 90% (n=45). There were no exemptions to gaining IV access in either audit for severely septic patients.
Further analysis of confirmed severe sepsis cases in the retrospective audit revealed that 50% (n=65) of these patients received IV antibiotics in under an hour, a standard required in the ‘Sepsis Six’. Of the patients receiving antibiotics under an hour, 68% (n=44) of these were pre-alerted to the emergency department. Overall, in severe sepsis, patients pre-alerted to the department had an average time to antibiotic administration of 66 minutes, compared to 109 minutes in patients not pre-alerted to the department.
| Retrospective audit (n=259) | Prospective audit (n=100) |
|---|---|
| Sepsis cases = 129 | Sepsis cases = 50 |
| Severe sepsis/sepsis shock = 130 cases | Red flag/severe sepsis = 50 cases |
| Sepsis metric | Retrospective audit | Prospective audit |
|---|---|---|
| SIRS criteria fully assessed | 90% | 98% |
| Suspicion of sepsis documented on PRF and SIRS fully assessed | 15% | 94% |
| Hospital pre-alert for severe sepis/red flag sepsis | 54% | 98% |
| Severe/red flag sepsis patients receiving IV fluids | 20% | 88% |
| Severe/red flag sepsis patients with a BP <90 mmHg receiving IV fluid | 54% | 100% |
| Severe/red flag sepsis patients with IV access gained | 25% | 90% |
| Severe/red flag sepsis patients receiving IV fluids, O2 (if indicated), pre-alert and documented suspicion of sepsis on PRF | 10% | 90% |
Further to this, 46% (n=60) of severe sepsis patients presented to the ambulance crew with an initial systolic blood pressure of <90 mmHg. However, only 54% (n=32) of these patients had IV access gained and received IV fluid. On average, patients with pre-hospital IV access gained received IV antibiotics in hospital within 75 minutes, compared to 90 minutes in patients without pre-hospital IV access.
Discussion
The screening tool implemented was found to identify 89% of all sepsis cases and 90% of all confirmed severe sepsis cases. This would suggest the tool has a high degree of ‘sensitivity’ and is assumed to have reduced the episodes of NWAS clinicians not identifying sepsis cases if applied correctly. This directly challenges Guerra et al (2013) finding that sepsis is missed 51–63% of the time pre-hospital.
The pilot implementation evidenced an increased compliance with the full measurement of SIRS markers currently used to identify sepsis patients, and the subsequent documentation of a suspicion of sepsis from 15% (n=39) to 94% (n=94). Though not statistically comparable, the results do show evidence that staff are documenting a suspicion of sepsis as per pathway guidelines, which Studnek et al (2012) state reduces the time for the ‘Sepsis Six’ to be delivered in hospital. The complete assessment of SIRS markers, including blood glucose measurement which was the most commonly missed (68%) observation, potentially enabled an increased number of patients with sepsis to have their condition identified.
It is noted that there is a likely move away from SIRS criteria as the basis of sepsis identification, but until the proposed sepsis classification changes are announced, two or more SIRS markers, plus a suspicion of infection, remains the current definition of sepsis. There are patients such as those on beta blockers that will not show raised SIRS markers despite having sepsis. Clinicians should therefore be mindful of taking a full history including an assessment of the patient's medication when assessing if a patient with an infection is potentially septic.
Research has shown that if suspected severely septic patients receive pre-hospital fluid boluses, supplemental oxygen and a hospital pre-alert (Seymour et al, 2014), and the suspicion of sepsis is documented on the patient report form (Studnek et al, 2012), patient mortality is reduced. The results of the prospective study show significant improvements in the evidence-based care bundle delivered to sepsis patients, improving from 10% (n=13) to 90% (n=45). Therefore, summary can be made that the patients in the pilot received improved care and a potential reduction in mortality. This evidences the research of Plambech et al (2012) that the introduction of diagnostic and treatment pathways in conjunction with education improves compliance with evidence-based care bundles. It also reflects the need for a standardised national pre-hospital sepsis policy, as is currently being developed by the Joint Royal Colleges Ambulance Liaison Committee (JRCALC), with the National Institute for Health and Care Excellence also reviewing and identifying ‘best practice’ for sepsis identification and management. A lack of condition specific guidelines has in the past shown a variation in care levels provided (Middleton et al, 2001), something this pilot evidences can be reduced if a specific sepsis guideline is introduced.
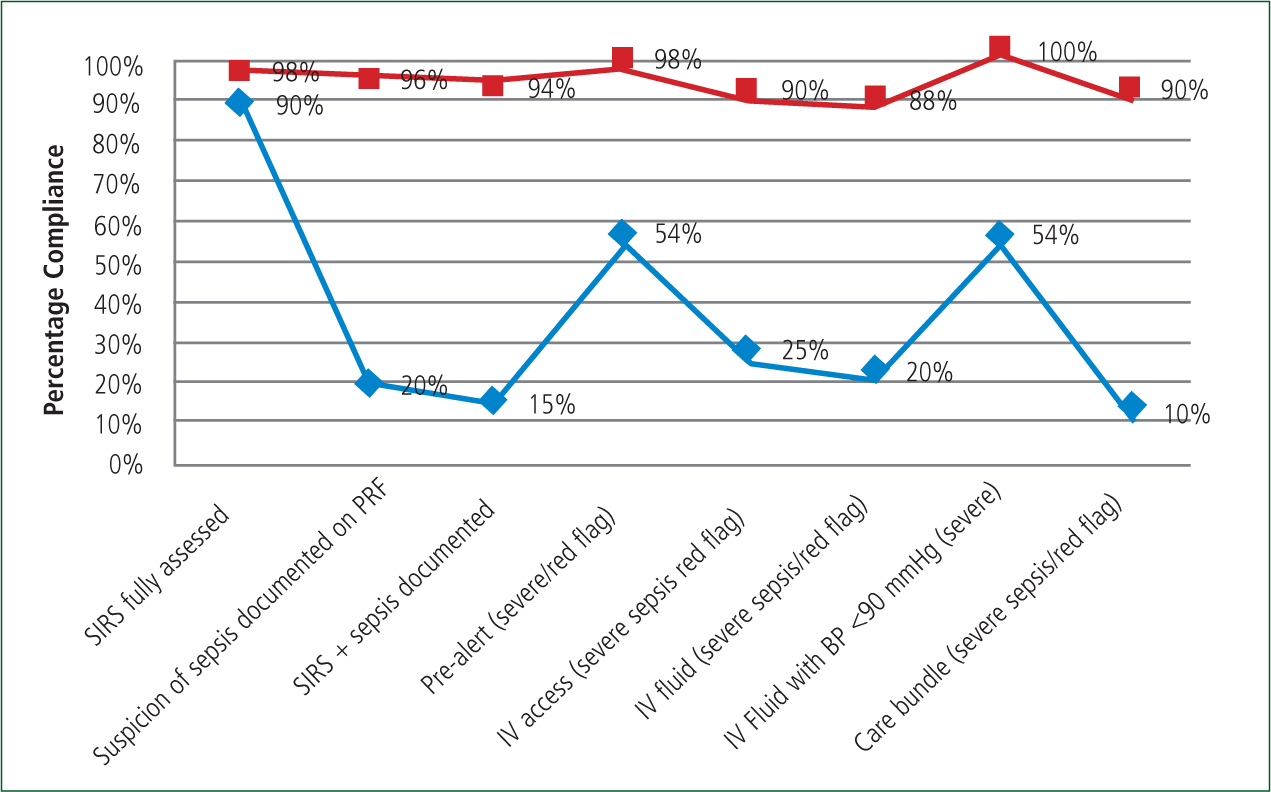
The 259 case retrospective audit evidenced that if patients received a hospital pre-alert, then the average time for patients receiving IV antibiotics reduced from 109 (n=46) minutes without to 66 (n=66) minutes with. If IV access was gained, the average time to antibiotics fell from 90 (n=77) minutes without to 75 (n=31) minutes with IV access gained. As an increased percentage of patients have been shown in the prospective trial to receive appropriate pre-alerts from 54% (n=70) to 98% (n=49), and IV access from 25% (n=32) to 90% (n=45), assumption can be made this will mean an increased percentage of patients will subsequently receive IV antibiotics within a shorter time frame, hence reducing mortality (Seymour et al, 2012). This will minimise the likelihood of delayed antibiotics, which increases mortality by 7.6% per hour delay in severe sepsis (Kumar et al, 2006).
The retrospective study also evidenced that only 46% (n=60) of patients with severe sepsis diagnosed on arrival at hospital had a pre-hospital systolic blood pressure of less than 90 mmHg. Current JRCALC and NWAS guidelines only indicate fluid therapy/boluses in patients with a systolic blood pressure <90 mmHg. The duration of hypotension before antibiotic administration has been shown to be a critical determinant in mortality by Talan et al (2008). However, this indication for fluid boluses has to be balanced against the risk of over compensation with fluids (Boyd et al, 2011).
This study therefore evidences that 56% (n=70) of severe sepsis patients that would benefit from pre-hospital fluid boluses would not be indicated for IV fluids under current JRCALC guidelines, therefore presenting with ‘cryptic shock’. This exists when a patient's blood pressure is >90 mmHg, but there is evidence of tissue hypoxia and worsening sepsis. In this pilot, a 250 ml bolus of normal saline was indicated in suspected ‘Red Flag’ sepsis, repeated once if necessary after reassessment of the patient's vital signs. This, as discussed, was outside current JRCALC pre-hospital guidelines, but it was determined the benefit to the patient outweighed the risk of over infusion. Another reason for the inclusion of IV fluids in normotensive patients was if a patient is cannulated and/or given intravenous fluid by paramedics then a faster triage and quicker initiation of care within ED is reported and a subsequent reduction in mortality (Seymour et al, 2014). Compliance with IV fluids in severe sepsis increased from 20% (n=26) to 88% (n=44) in the prospective trial without any adverse incidents being recorded. This would suggest that paramedics are safely able to give IV fluid boluses to suspected severe sepsis patients that are normotensive.
Previous research by Vanzant and Schmelzer (2011) suggests difficulty in identifying patients and a desire for clinicians to treat conservatively as reasons for resistance to protocol uptake within A&E. During this pilot, this was not evidenced and the overall positive feeling among staff was relief that guidance had been provided on managing sepsis, a typically poorly recognised/treated condition in the pre-hospital environment. This lack of resistance was evidenced in the accurate application of the tool, and good compliance with the treatment pathway.
Recommendations for enhancement
The key development for this sepsis pilot is highlighting a need for change, evidencing a ‘research-practice gap’ which can generate larger scale change across NWAS (Antman et al, 1992). Evidence suggests that triage tools based on ‘Manchester Triage’ do not identify sepsis (Burney et al, 2012), leaving the patient at risk from delayed sepsis identification. The results of the audit to date indicate a need for a sepsis protocol to be rolled out across NWAS to supplement ‘Paramedic Pathfinder’ and for the protocol to be further developed as more research is published.
The project continues to run in its prospective phase. The second phase of this plan, using the 100 prospective cases of sepsis, is tracking the end diagnosis of each case at hospital and assessing the ‘specificity’ of the newly introduced pre-hospital sepsis screening tool. The tool introduced has been shown to have a high degree of sensitivity in this pilot. The ‘end diagnosis’ assessment will continue and be written up in a subsequent paper evaluating the ‘sensitivity’ and ‘specificity’ of the ‘Red Flag Sepsis’ concept introduced by the UK Sepsis Trust.
Limitations
The pilot at this stage does not report back on the end diagnosis of the patients treated for ‘Red Flag’ sepsis. There is therefore an assumption at this stage that identification of ‘Red Flag’ sepsis criteria links to a hospital diagnosis of severe sepsis. It is not possible to confirm that severe sepsis patients in the prospective pilot received care that incorporated an increased compliance with an appropriate care bundle for their diagnosed condition. This analysis is continuing and will be reported in a separate paper.
The increases in compliance with delivery of a sepsis care bundle, though obvious in terms of percentage increase, are not reported in terms of ‘statistical significance’. This may leave the pilot's improvement claims open to suggestion of a lack of scientific rigor in its design.
Conclusions
The introduction of a modified ‘Red Flag’ sepsis screening tool and treatment pathway, alongside a taught education package, evidenced a high degree of sensitivity in sepsis identification and has improved the level of compliance with a tailored treatment bundle of care, potentially reducing intensive care unit admissions, avoiding significant costs, and subsequently reducing mortality levels.
Specific sepsis care interventions, such as fluid bolus and high flow oxygen, have been delivered to potentially severe sepsis patients without untoward incident. It was also found that a hospital ‘pre-alert’ and ‘IV access’ seemed to reduce the time to patients receiving IV antibiotics for sepsis in hospital.
Irrespective of whether this sepsis protocol is expanded to cover NWAS, what has been shown within literature and this pilot is the importance of using the terminology ‘sepsis’ and ensuring this is documented clearly on any patient documentation in increasing the hospital's ‘Sepsis Six’ bundle compliance. This small change does not challenge any existing practice, but ensures all clinicians are adopting the same language and terminology in highlighting and treating this potentially fatal illness.
Key Points
Conflict of interest: none declared.

