Trauma is a primary contributor to the burden of disease globally (World Health Organization (WHO), 2010). In the UK and North America, trauma is the leading cause of death for people aged 1–44 years, with 70% of these deaths occurring to those in the 15–24 age group (WHO, 2010). Trauma haemorrhage is the leading cause of preventable deaths, accounting for approximately 40% of all cases worldwide (Frith and Brohi, 2010).
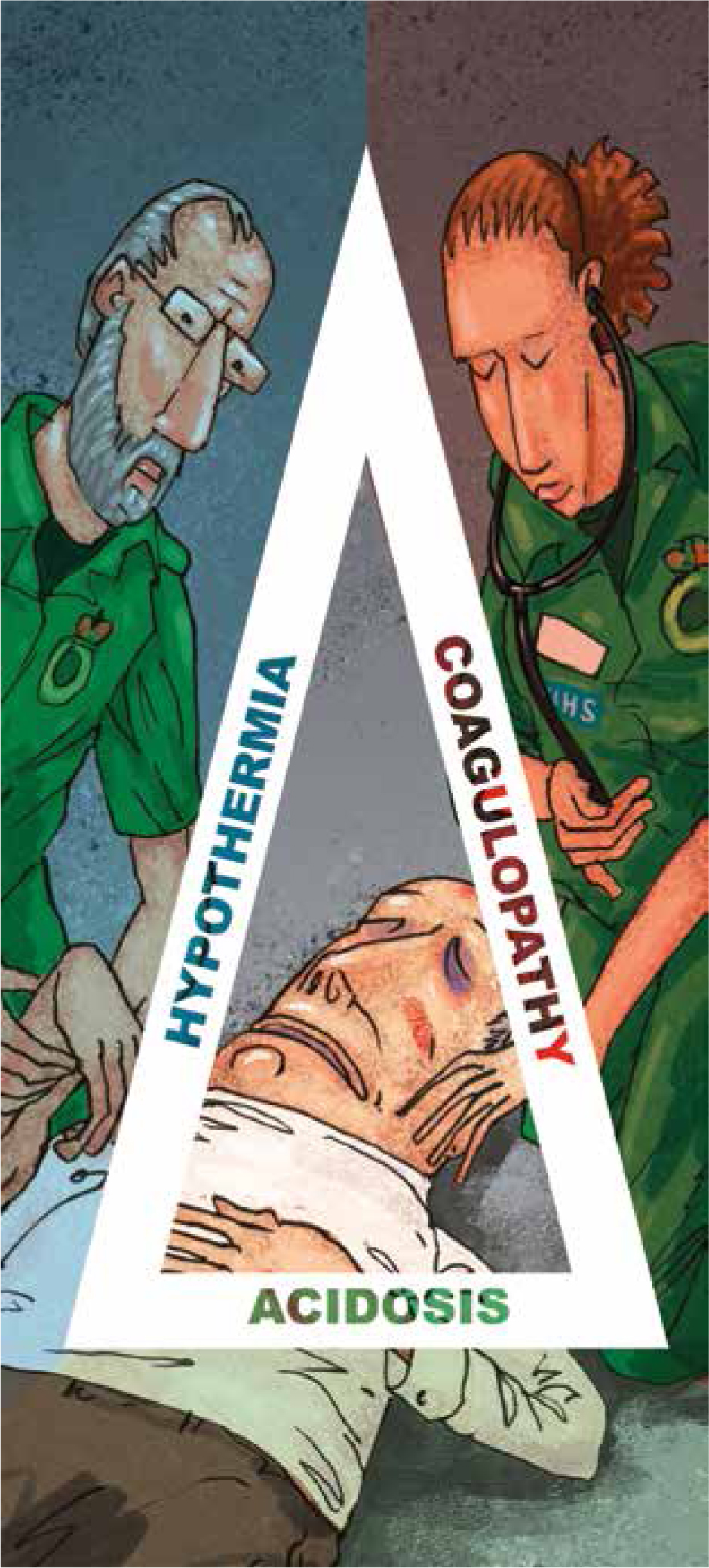
Acute traumatic coagulopathy (ATC) is an internal process initiated by significant trauma because of hypoperfusion resulting from hypovolaemic shock, activation of protein C, platelet dysfunction and disruption to the endothelial glycocalyx (Duan et al, 2015). ATC can be exacerbated by hypothermia, acidosis and dilution coagulopathy, which together are known as the ‘lethal triad’ of trauma (Credland, 2016).
The pathophysiology of ATC includes massive or significant trauma and in addition to leading to hypoperfusion, subsequent activation of protein C, platelet dysfunction and endothelial glycocalyx destruction, it reduces the available fibrinogen (Davenport, 2013).
Damage to the vascular endothelium caused by significant trauma results in the release of protein C, which is a key mechanism for the activation of ATC (Floccard et al, 2012). ATC is common in patients who have been involved in severe trauma, and results in high rates of mortality and morbidity (Gando et al, 1999).
ATC can occur relatively early in the patient who has experienced significant or massive trauma and manifests primarily because of tissue and or vascular injury and subsequent hypovolaemic shock (Davenport, 2013).
ATC has a profound effect on the normal response to major haemorrhage, with mortality being 2–3 times greater than in patients with normal coagulation values, as it has a major effect on the body's ability to arrest significant bleeding (Hess et al, 2006).
Knowledge of ATC's pathogenesis will enable the prehospital practitioner to provide clinical interventions to arrest its development in the critically injured patient. The combination of hypothermia, acidosis and coagulopathy as a result of trauma—the ‘lethal triad’—has long been thought to be the primary cause of death among patients of major trauma (Li and Sun, 2015).
Hypothermia
The prehospital clinician is often the first to manage a patient with a reduced temperature as a result of loss in circulatory volume caused by trauma so has an important early role in the management of hypothermia. Hypothermia is defined as a core body temperature below 35°C, with mild hypothermia categorised as 32–35°C, moderate hypothermia as 28–32°C and severe hypothermia below 28°C (Joint Royal Colleges Ambulance Liaison Committee (JRCALC), 2016).
Patients presenting with ATC in the emergency department are four times more likely to die than patients with a normal state of blood coagulation (Brohi et al, 2008). ATC can be exacerbated if the patient's body temperature falls to a hypothermic level and their blood becomes acidic (Moffatt, 2013). The combination of hypothermia and acidosis has an adverse effect on the body's ability to arrest haemorrhage and results in a further increase in mortality and intensive care unit admissions (Gando et al, 1999).
Haemorrhage from major organs, bones and other tissues results in a fall in circulatory volume, which in turn decreases the body's ability to maintain its core temperature because the supply of oxygenated blood vital to organs and tissues is reduced (Credland, 2016). However, in patients who have experienced trauma, a temperature <36°C is considered as hypothermia with severe hypothermia at <32°C (Thorsen et al, 2011).
The regulation of body temperature is influenced by many factors such as the weather, prolonged entrapment and cold intravenous fluid administration; cellular hypoperfusion because of trauma also plays a significant role in the loss of body heat (Søreide, 2014). These factors when combined with injury have been referred to as trauma-induced hypothermia whose cellular effects result in a switch from aerobic cellular respiration and the use of adenosine triphosphate (ATP) to the anaerobic form of energy production using adenosine diphosphate (ADP). ATP is far more efficient at generating heat than ADP and, as a result, heat production is further impaired (Kheirbek et al, 2009).
Furthermore, as temperature falls, the production of thrombin (factor IIa) is reduced and, as a consequence, coagulation time is prolonged; this is exacerbated as the patient's temperature continues to decrease (Simmons et al, 2014). At temperatures <33°C, the coagulation activity of tissue factor and factor VIIa is reduced, which has a direct effect on the synthesis of fibrinogen (Martini, 2009). This state of trauma-induced hypothermia can result in a reduction of coagulation clotting factors by approximately 5% for every 10°C loss in body temperature (Kermode et al, 1999). Thorsen et al (2011) identified that thermoregulation is impaired as a consequence of severe injury, which results in the body becoming unable to shiver as a means to generate heat.
A large-scale study, the Prospective Observational Multicenter Major Trauma Transfusion Study (PROMMTT) (Holcomb et al, 2013), which enrolled 1245 patients, at 10 level 1 trauma centres throughout the US, concluded that a temperature <35.8°C was an independent risk factor for the development of ATC, resulting in a higher mortality than when patients had a normal body temperature. A study by Ireland et al (2011) reviewed 732 medical records of major trauma patients presenting to an adult major trauma centre. The mortality of patients with hypothermia secondary to major trauma was 29.9%, with a threefold independent risk of death.
The PROMMTT study also found that decreases in temperature to 32°C resulted in higher mortality and that a temperature of <35°C is an independent predictor of mortality following major trauma (Holcomb et al, 2013).
In moderate hypothermia, platelet function is also decreased with their activation, aggregation and adhesion properties impaired. Hess et al (2006) suggested that this is because vWF traction on the surface of platelet glycoprotein receptors is reduced, adding that when a patient's temperature falls <30°C, the interaction of vWF glycoprotein receptors and platelets ceases in 75% of all cases. Meng et al (2003) identified a reduction of 20% in the effectiveness of platelet function and enzyme activities at temperatures <33°C. Research since has identified that thrombin generation is also reduced in hypothermia (Mitrophanov et al, 2013).
Hypothermia management advocates the active warming of patients with trauma-induced hypothermia and the use of blankets, heat pads and, where possible, a safe and rapid extrication of patients from the scene (Aitken et al, 2009).
Lundgren et al (2011) showed significant evidence of the positive effects that the prevention and management of hypothermia can have on mortality. This has been further highlighted by guidance on the initial assessment and management of major trauma from the National Institute for Health and Care Excellence (NICE, 2015), which suggests the use of warmed crystalloid fluids or blood products instead of cold fluids which could increase the risk of further temperature impairment.
Acidosis
Patients who have experienced severe haemorrhage because of traumatic injury have a consequent reduction in their oxygen circulatory carrying capacity (Simmons et al, 2014). This results in less oxygen being available for cellular respiration.
Cellular energy is predominantly fuelled by oxygen and its interaction with ATP with the presence of glucose and oxygen within cells, resulting in the production of 38 molecules of ATP. When metabolised, this reaction produces energy byproducts of water and carbon dioxide (CO2), which are primarily removed by the respiratory and renal systems (Edwards, 2008).
Reduced oxygen to the cells as a consequence of trauma hypoperfusion leads to a decrease in available ATP, which results in adverse cellular damage caused by hypoxaemia (Edwards, 2003). To facilitate energy production, cellular metabolism switches from aerobic cellular respiration to anaerobic respiration. In an attempt to meet cellular energy demands in the presence of cellular hypoxia, the body endeavours to produce energy via glycolysis (Guyton and Hall, 2015). This source of ATP production, however, is less efficient than aerobic metabolism and only two ATP molecules are produced per glucose molecule so this energy source can be sustained for only a very short period of time before cellular damage occurs (Michiels, 2004). During prolonged anaerobic metabolism, harmful byproducts are generated in the form of carbon dioxide and lactic acid. Carbon dioxide and lactic acid in the blood result in a build-up of hydrogen ions (H+) and a subsequent decrease in the blood's pH (Campbell, 2006).
To compound this process, cell membranes become leaky, resulting in cellular oedema, which further impairs oxygen delivery to tissues. Anaerobic metabolism, combined with the effects of cellular oedema and decreased cellular oxygenation, results in an even greater production of lactic acid and free radicals (Martini, 2016). Continued failure of the circulation system because of hypovolaemia induces a state where acidaemia occurs because the body is unable to remove lactate at a rate sufficient to maintain blood pH within its optimal range. Prolonged anaerobic metabolism results in high concentrations of lactic acid, causing a decrease in the patient's pH level (Credland, 2016).
The human body balances its pH in the range of 7.35–7.45 (Marieb and Hoehn, 2014) and the increase in cellular-produced lactic acid elevates the amount of hydrogen ions in the blood (Eberhard et al, 2000). This is exacerbated by the kidneys' ability to filter out the increase in hydrogen ions being impaired as a result of hypoperfusion. Bicarbonate reserves become exhausted owing to the body's compensatory mechanisms endeavouring to buffer the increase in hydrogen ions, and acidaemia occurs (White, 2013).
A decrease pH causes additional cellular damage and results in the activation of the inflammatory response and the release of negative inotropes. These negatively charged inotropes cause vasodilation in a patient who is already circulatory compromised, resulting in decompensated hypovolaemic and irreversible shock (Pearson et al, 2014).
Coagulation is less effective in acidic blood, with the activity of clotting factors reduced when the pH of blood falls below 7.3 (Sorensen and Fries, 2012). To measure coagulation time, Martini et al (2006) facilitated a study with the aid of two methods that quantify the time it takes for both the intrinsic and extrinsic coagulation cascades to activate. Partial thromboplastin time is a measure of the intrinsic coagulation pathway and prothrombin time is a measure of the extrinsic pathway; measuring both times showed coagulation time was longer at a lower pH (Martini et al, 2006). Furthermore, at a pH lower than 7.1, thrombin generation is impaired by almost 50%, prothrombin time was increased and fibrinogen was substantially depleted by 34%. The same study also found platelet count was reduced by 51% (Martini, 2016). Hess et al (2006) report the activity of coagulation factors Xa and Va is reduced by 50% at a pH of 7.2, 70% at pH 7.0 and 90% at pH 6.8, indicating the negative effect that acidosis has on coagulation cascade.
In contrast, Dirkmann et al (2008) studied the effects of metabolic acidosis and/or hypothermia on blood coagulation and found no significant coagulation changes were evident in the presence of acidosis. However, when metabolic acidosis was accompanied by hypothermia, clotting times were significantly increased within both the intrinsic and extrinsic coagulation pathways. This study was small, involving only 10 healthy volunteers, but it does highlight the negative effect of metabolic acidosis and hypothermia on blood coagulation when combined. Meng et al (2003) showed that, even if coagulopathy is treated via the administration of recumbent factor VIIa, bleeding time is still not arrested in the presence of metabolic acidosis. Further research by Darlington et al (2011) on pigs also found that, even if acidosis is corrected, the coagulation system remains impaired, which may suggest that irreversible damage to the clotting enzymes occur during this acidic state. This may highlight the need to ensure that the potential for metabolic acidosis is recognised early and treatment instigated to prevent it (Theusinger, 2015).
Treatment of metabolic acidosis from a prehospital perspective relies upon the prevention of respiratory acidosis via the application of high-flow oxygen therapy to maintain or increase oxygen delivery and subsequent cellular perfusion (Shere-Wolfe et al, 2012). As such, all critically ill patients and those who have received significant trauma should receive immediate supplementary oxygen, irrespective of their oxygen saturation (NICE, 2017). However in patients who are not critically injured or have experienced significant trauma, oxygen saturation should be targeted in the region of 94–98%, as hyperoxaemia has been shown to cause oxidative stress and can damage neurons that have been deprived of oxygen (Nolan, 2016).
The use of crystalloid infusion to control blood pressure (BP) and subsequently cellular perfusion pressure has been historically controversial (MacDonald, 2015). It has been suggested that, as crystalloids are acidic in nature (sodium chloride pH 5.0 and Ringer's lactate pH 6.5), their excessive use in the presence of metabolic acidosis can exacerbate the metabolic condition (Skellett, 2000).
The use of crystalloid fluid resuscitation needs to be carefully balanced against the negative effects of acidosis and the need for enough adequate vascular volume to maintain perfusion of cells. Current guidance advises that prehospital clinicians should limit crystalloid infusion to boluses of 250 ml to maintain a lower arterial BP than normal (NICE, 2017). This guidance is further endorsed by the findings of Haut et al (2011) and the European guideline on management of major trauma (Rossaint et al, 2016) and research undertaken by Dick et al (2013).
ATC management strategies
The aggressive use of 1500 ml of a crystalloid infusion in patients who have experienced trauma and reduced BP was once deemed beneficial (Simmons and Powell, 2016). However, numerous studies have now provided data that suggests that further injury results from the overuse of crystalloids (Brown et al, 2013; Credland, 2016; Rossaint et al, 2016). It is thought that the mechanism for this is an increase in hydrostatic pressures because of higher vascular volumes from fluid resuscitation causing disruption of clots, a dilution of coagulation factors, a subsequent reduction in the patient's body temperature and further disruption of the endothelial glycocalyx (Haut et al, 2011). Maegele et al (2007), who studied 1898 patients receiving high-volume crystalloid administration in the prehospital setting found they had a higher rate of coagulopathy, mortality and blood transfusion requirements on admission to hospital than patients who had lower volume crystalloids administered.
The rationale for permissive hypotension is to achieve a BP that is below normal values. Hussman et al (2013) performed a similar analysis with the German Trauma Registry database reviewing a total of 1826 patients with multiple injuries and a systolic BP>60 mmHg and concluded that those who received low-volume fluid administration prehospital (0–1500ml) had a better survival rate than those who received >1500 ml of intravenous crystalloids. The strategy of restricting fluid volume replacement was also highlighted by Morrison et al (2011) in a randomised controlled trial of 90 patients presenting with penetrating trauma, associated prehospital hypotension and hypovolaemic shock. Morrison et al concluded that coagulopathy was increased in patients with a higher mean systolic BP because of crystalloid administration when compared with those patients who did not receive fluid resuscitation.
Current UK paramedic guidance on the prehospital use of fluid resuscitation advocates that clinicians aim for a target systolic BP of no less that 60 mmHg in penetrating trauma to the torso. The guidance provides further detail in respect of blunt trauma and advises achieving a systolic BP close to 90 mmHg to avoid the potential effects of dilution coagulopathy (JRCALC, 2016).
Fibrinolysis occurs as part of the normal coagulation process and ensures that clot breakdown occurs following repair and that further clot formation is inhibited (Lippi et al, 2014). Tissue plasminogen activator (TPA) is activated following injury to vascular endothelial cells and its mechanism of action is to convert plasminogen to plasmin, which has the effect of breaking fibrin bonds (Cole et al, 2015). Plasminogen activator-inhibitor (PAI) inhibits TPA but, the activation of protein C, because of significant trauma and hypoperfusion, results in the depletion of PAI and TPA is able to convert plasminogen to plasmin at an accelerated rate; this is known as hyperfibrinolysis (Raza et al, 2013).
The Crash 2 trial by Roberts et al (2013) investigated 20 211 patient and found when patients were administered tranexamic acid they found a significant reduction of 9% in the risk of death and a subsequent 15% reduction in death caused by major haemorrhage. Moreover, Reade et al (2013) identified that the mechanism of action of tranexamic acid (TXA) prevented hyperfibrinolysis by binding with plasminogen and inactivating plasmin to ensure stable clot formation. The CRASH 2 trial also highlighted that the patients who had received the most significant trauma and had a systolic BP <75 mmHg benefited most from TXA administration (Roberts et al, 2013). Research by Morrison et al (2012) found an absolute risk reduction in mortality of 6.5% when patients received TXA, with the most significant survival rates observed in patients who had received TXA and packed red blood cells. It has also been suggested that overall mortality is further reduced if administration is undertaken within 3 hours of injury (Edwards and Smith, 2016).
Conclusion
ATC occurs as a result of significant trauma and is exacerbated by the effects of hypothermia and acidaemia. The intrinsic and extrinsic coagulation pathways are compromised in patients with significant trauma who are hypothermic and acidotic. The prehospital management of ATC requires paramedics to address the effects of hypothermia and acidosis to limit the effects of coagulopathy. Failure to manage ATC, hypothermia and acidosis results in high mortality rates.
Treatment regimens should include high-flow oxygen to address reduced blood pH and the prevention and correction of hypothermia to promote an environment where the coagulation cascade and platelet adhesion can thrive. Targeted use of fluids to maintain BP at the lowest required level to prevent further acidosis and dilution coagulopathy is essential as is the use of TXA to limit fibrinolysis.

