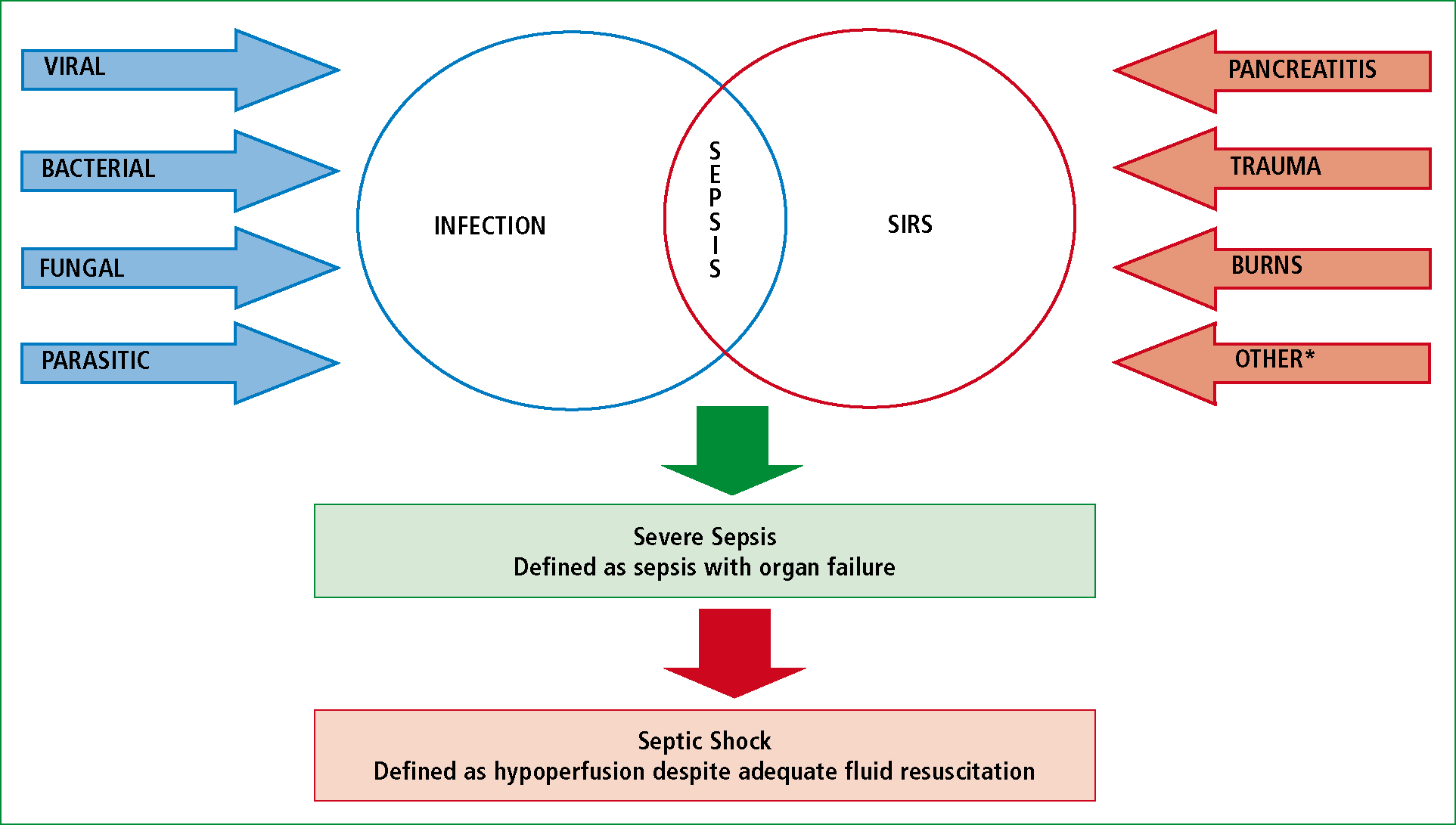
Sepsis may be defined as an overwhelming, uncontrolled, systemic inflammatory response, which is mediated by the immune system, the vascular endothelium and inflammatory pathways in response to an infective trigger. An alternative definition is that of a systemic inflammatory response syndrome, (SIRS) in response to a confirmed infectious process (Bone et al, 1992). SIRS may be defined as a systemic response to a variety of initiators, of which infection is one. SIRS alone is not sepsis and neither is it a diagnosis. As can be seen in Figure 1, SIRS can be caused without the presence of an infective agent, as in the case of trauma or burns for example. Also, many people develop infections without developing sepsis. Evidence suggests it to be a combination of the infective agent and the host response, or over-response, which leads to sepsis. It is currently hypothesised that there may be a genetic element, which predisposes some patients to developing sepsis, where others would develop infection without a systemic response (Villar et al, 2004). An aging and increasing population will only increase the occurrence of sepsis in the UK.
Pathophysiology
Sepsis occurs when a simple infection develops to cause an overwhelming, inappropriate infammatory response. The causative pathogen is identifed by the host's innate (non-specifc) immune system, which triggers cytokine release (infammatory proteins), neutrophil activation and helps to initiate the host's specifc adaptive immune response to that pathogen. Adaptive immune systems target specifc threats to the host through the amplifcation of cytokine release, synthesis of antibodies and phagocytosis (engulfng and destruction) of pathogens. This response, if it were to continue, gives rise to vasodilation through cytokine and nitrous oxide release, and endothelial cell damage from both cytokines and the release of exotoxins from phagocytosed pathogens. At this point, if the balance of harm outweighs the beneft to the host, the response becomes inappropriate, with relative hypovolaemia resulting from vasodilation, with resultant poor tissue perfusion and oxygen extraction. Capilliary leakage occurs, with extravasation of intravascular fuid causing tissue oedema and absolute hypovolaemia, with intravascular thrombus formation. The net result of overwhelmed immune responses is acidosis, myocardial impairment, interruption of the procoagulant/thrombolytic balance leading to disseminated intravascular coagulation (DIC) and microcirculatory collapse (Daniels and Nutbeam, 2010). Ultimately the hyper-infammatory response becomes blunted, apoptosis is triggered, with an irreversible death of immune, epithelial and endothelial cells (Jui, 2011). Worsening tissue perfusion causing anaerobic respiration accelerates the effects of sepsis creating a cycle of increasing damage and eventually organ dysfunction. Sepsis can thus manifest as organ failure of different systems through hypoperfusion (Bonner and Ryan, 2011): acute lung injury and acute respiratory distress syndrome within the respiratory system, acute renal failure, confusion and depressed level of consciousness, ileus, adrenal insufficiency, systolic and diastolic dysfunction, hypotension.
Lactate is created as a by-product of anaerobic metabolism, as a consequence there is always a low level of this chemical in the body. Lactate levels rising above normal show that the balance of lactate production and elimination has been overtaken by increased lactate production. This is an excellent indicator of reduced aerobic metabolism resulting from tissue hypoperfusion, which in turn gives rise to multi-organ dysfunction. A lactate level of greater than 2 mmol/L is a good diagnostic indicator of organ dysfunction, with levels greater than 4 mmol/L indicative of shock. Raised lactate levels can confirm the presence of cryptic shock as described by Nee (2006) in patients where signs and symptoms of shock, including hypotension and confusion, have yet to manifest themselves. As identified by Puskarich et al (2011), this carries a mortality rate that is not significantly different to overt septic shock. Lactate levels also give an indication of mortality, with higher levels predicting a poorer outcome (Nguyen et al, 2004).
Bacteria are responsible for the majority of cases. There is a roughly half-and-half split between gram-negative and gram-positive bacteria as causative agent, where bacteria are the culprits. Of the overall causes of sepsis, the most common sites are lung (around 50 % of cases), intra-abdominal (20–25 %) and urinary tract (around 10 %) (Nee, 2006; Daniels, 2010). Fungal infection is responsible for 5–10 % of sepsis overall, predominantly in the immunocompromised or neutropenic patient.
Prevelance
The Intensive Care National Audit and Research Centre (ICNARC) data estimates over 100 000 cases of sepsis occur annually in the UK, with almost 37 000 deaths as a result (Harrison et al, 2006). The UK Sepsis Report of 2011 shows that a patient with sepsis is six times more likely to die than a patient with acute coronary syndrome or stroke (Harrison et al, 2006). Severe sepsis kills more people in the UK than either lung cancer, or both colon and breast cancer combined each year. This translates to mortality as high as 30–40 % from severe sepsis and 50 % from septic shock. Such figures as these inevitably mean a huge burden on NHS resources. In England, Wales and Northern Ireland, around 27 % of all intensive care unit (ICU) admissions are as a result of severe sepsis. As per The Intensive Care Society report ‘Critical Insight’ (2006) each ICU bed is currently estimated to cost between £ 1000 and £ 1800 per patient/day (Bennett and Bion, 1999). This does not factor in time and cost relating to ambulance services, emergency department treatment, or medical and high-dependency beds, it also does not factor in the human cost to families and the patient themselves.
Early recognition and aggressive management with consistant patterns of cinical practice, has been found to improve patient outcome (Nguyen et al, 2007), also reducing cost by reducing length of time in intensive care settings, high-dependency settings and hospital overall. The better the quality of treatment and the sooner it is initiated, the better chance the patient has of returning to their pre-morbid functional status, the shorter the hospital stay and the lower the cost to the NHS. If this early recognition can be at first contact with any healthcare professional, there is a significant time saving in terms of treatment, as well as a smoother patient care pathway.
Recognition
As asserted, sepsis is the presence of SIRS with an infective trigger. There is a well-recognised criterion for the identification of SIRS in the hospital setting.
SIRS criteria: (any two of the following represents SIRS)
It is not possible to measure white cell levels pre-hospitally, and the stress of an emergent situation is often enough to increase heart rate and breathing rate. Pre-existing medical conditions may cause the patient's baseline observations to be outside the accepted normal parameters. Similarly, we recognise that it can be difficult to ascertain whether an altered mental state is acute or chronic in the field. However, a diagnosis of a SIRS picture is often made in emergency departments before white cell counts or definitive background mental state is known, therefore it is possible for pre-hospital clinicians to apply the criteria as they can and use a high degree of suspicion, justified by the figures related earlier.
Other markers are known as indicators of the severity of sepsis and can play a role in informing the clinical condition of the patient and aggressiveness of the response needed. These markers indicate organ function; dysfunction denotes severe sepsis and septic shock, which is severe sepsis with hypotension that fails to respond to fluid resuscitation. Perhaps the most understood marker for the pre-hospital professional is that of blood pressure. Identifying shock through simple parameters is something that pre-hospital practitioners become versed in from initial training. Within sepsis it relates to cardiovascular system failure, and is managed with familiar fluid resuscitation. It should be made clear at this point however, that the shocked patient is likely to need large amounts of fluid. Lactate is an indicator of tissue perfusion, with a raised lactate showing tissue hypoxia, even in the normotensive patient (Nee, 2006). This should be used to guide the relatively aggressive fluid resuscitation of a patient who may seem not to warrant it under other circumstances. Improvement in perfusion could be seen in a falling lactate if facilities to test this are available. Without this it may be necessary to rely on clinical indicators such as heart rate, breathing rate, peripheral perfusion, and mental status rather than simply on blood pressure response to fluid boluses. Recent oligouria or anuria may represent renal failure, which is often acute, or acute-on-chronic during the septic insult, so this aspect of history which is often neglected is also important in establishing a picture of severity.
Temperature should be measured on initial contact with any patient, and again with each set of observations if SIRS or sepsis is suspected. This seemingly simple observation should not be underestimated, as identified by Brun-Buisson et al (1995) hypothermia in particular is a poor prognostic indicator compared to hyperthermia, with mortality as high as 80 % in these patients. Data suggests this may be linked to the ferocity of the immune response. Alternatively, fever may be minimal or absent in elderly patients in particular, as well as the overtly immunocompromised, such as patients who have recently had chemotherapy or those with HIV/AIDS.
On the grounds of this, we would advocate a severe sepsis screening tool such as that proposed by Daniels and Nutbeam (2010) with some adjustments for current practice and equipment availability. At present, the majority of ambulances do not carry equipment to measure lactate, nor is it always easy to determine the patient's urine output in the preceding hours. Sepsis should be identified if there is:
Severe sepsis is defined as sepsis with organ dysfunction, hypoperfusion, or hypotension. Septic shock is the presence of severe sepsis with hypotension that is not reversed by fluid resuscitation. Clinically, hypoperfusion presents with a reduced level of consciousness, extended capillary refill time, cold and mottled skin (particularly at the peripheries), increased heart rate and increased ventilatory rate.
Treatment
The single most important factor in the management of sepsis is to recognise the condition early, or if in doubt, to maintain a high degree of suspicion, with goal-directed treatment (Rivers et al, 2001; Robson et al, 2009). As identified by Daniels and Nutbeam (2010), sepsis is a time critical disease process, in which prompt and aggressive initial resuscitation unequivocally reduces long-term morbidity and mortality. Primarily treatment must follow the standard ‘A, B, C, D, E' approach, it is important to observe and record the vital parameters for sepsis as well as a full set of basic observations including temperature and blood glucose molarity. This must be repeated so that any change in patient condition is noticed and recorded, as well as any initiation of treatment that caused the change in parameter. The sequence of events should be clearly documented so that hospital staff can review the progression of the patient before them and consider the need for further treatment in accordance with response and how the patient has been managed so far.
The airway becomes of particular importance if there is any degree of cognitive impairment. High flow oxygen is to be applied, as the septic patient is a critically ill patient requiring high flow oxygen, as per British Thoracic Society guideline for emergency oxygen use (O'Driscoll et al, 2008). A good primary check should be performed to look for signs of impaired breathing, both as a cause for sepsis and a confounding factor in those with preexisting respiratory disease, as well as increased breathing rate as a clinical indicator for sepsis and acidosis.
An active search must be made for signs of cryptic shock resulting in hypoperfusion of organs as described above, with early ECG monitoring due to an increased risk of arrhythmias. Large bore intravenous access should be obtained and fluid resuscitation commenced in an attempt to normalise physiological parameters such as cognition, ventilation and heart rate. Although it can be difficult to gain intravascular access to these patients, it is an important part of the resuscitation. Multiple attempts are not advocated if a delay in transport occurs, but standard procedures suggest two attempts and then resorting to intra-osseous access. Blood glucose measurements should be taken and any deficit replaced as the septic insult increases metabolic demand. It is not recommended to otherwise attempt tight glucose control in the pre-hospital environment. Fluid challenges are not to be confused with fluid administration; the former are large boluses administered over a very short time space under monitoring in order to assess physiological response, where as the latter are administered over a longer time in small amounts to maintain physiology (Dellinger et al, 2008). Crystalloids are currently the choice of fluid in pre-hospital settings due to ease of storage, low cost and low incidence of hypersensitivity reactions. Initial fluid boluses given to increase the intravascular volume and perfuse organs may need to be of the order of 20 mls/kg in resuscitation of the septic patient. If there is any doubt as to the patient's pre-morbid status or cardiac function, it is more advisable to give 250 ml aliquots, although overall large volumes may be required. In all patients after a fluid challenge has been given the patient should be reassessed in the same way that should occur after any intervention. Particular attention should be paid to the presence of any signs that are suggestive of fluid overload, particularly in the case of patients with coronary heart disease.
The Surviving Sepsis Campaign has identified primary goals that need to be achieved within one hour of commencing resuscitation. These are known as the ‘Sepsis Six' and should be cross-referenced with management initiated to ensure that goals are met. As asserted by Marik (2011) early antibiotics and haemodynamic resuscitation remain the cornerstones of successful treatment.
Sepsis Six (Daniels, Nutbeam, MacNamara and Galvin, 2011):
Another important factor in the patient journey is issuing a ‘pre-alert' to the receiving hospital (Robson et al, 2009). Historically these have been under-used pre-hospitally or under-rated at hospital unless part of a recognised protocol. However, these days they are met with a much better reception and awareness. The message should follow a set format, such as the ‘Situation, Background, Assessment, Recommendation’ (SBAR) format (Table 1), as it provides a frame for necessary information and will grab the receiving clinician's attention. It is useful to use phrases such as ‘I believe this patient has sepsis’, or alternatively ‘severe sepsis’ or ‘septic shock’ as appropriate. A delay in transporting the patient to definitive treatment must be avoided at all costs, as illustrated by Cronshaw et al (2011), as left untreated, each hour results in an average rise in mortality of 8 % per hour.
Future considerations
The understanding of the pathophysiology and management of sepsis are developing areas at present. There are areas where improvement can be made as outlined above. Perhaps the most obvious changes for the future are the introduction of ratified guidelines for pre-hospital management, with monitoring of their impact and honing of these guidelines as our understanding and skills increase. The Sepsis Six care bundle is implemented in hospitals countrywide for initial patient contact, while various ambulance Trusts are already becoming involved in a trial of guidelines adapted for pre-hospital use. The earlier recognition of sepsis has to be developed from training and education that highlights the issues involved, from initial clinical training through to post-basic training, on to extended skills courses such as critical care training with a view to higher education qualifications.
Other areas being looked at on a local level include trials of blood lactate monitoring equipment in order to help identify patients with sepsis and help direct fluid resuscitation. Alternative areas of focus include pre-hospital blood cultures with initial venous access in a sterile field and empirical antibiotic treatment for patients meeting severe sepsis or septic shock criteria. There are benefits and drawbacks to these ideas, and any trial would need close liaison between hospital and pre-hospital teams. However these ideas turn out, the debate opened can only lead to the fostering of stronger links, better communication, and shared understanding and education which would ultimately be of benefit to all, particularly our patients.
Pre-hospital lactate testing
Machines suitable for the pre-hospital measurement of lactate levels are now available and may be invaluable in assisting with early diagnosis and therefore treatment. These machines can measure lactate from venous samples easily obtained at initial access. Lactate levels can help to direct fluid management, indicating reperfusion and restoration of circulation by falling, although there may be an initial rise in levels as lactate is washed out of reperfused peripheries. Puskarich et al (2011) concluded that severe sepsis with cryptic shock carries a mortality rate not significantly different from that of overt septic shock, and suggested an elevated blood lactate of equal to, or greater than 4 mmol/L as the indicator for cryptic shock in the presence of otherwise normal physiology.
Pre-hospital blood sampling
Taking samples for later culture before any antibiotic therapy is commenced will enable the hospital microbiologists to identify the pathogen responsible and target future antibiotic therapy more precisely. These cultures are more likely to be positive if taken at any time when the patient has a temperature above 38.5°C or has overt sepsis. The risk here is the increased likelihood of contamination of samples, so care would need to be exercised when obtaining these samples, with procedures agreed by local hospitals.
Pre-hospital antibiotics
The need for urgent pre-hospital administration of antibiotics in suspected sepsis from meningococcal meningitis is already recognised, although waiting for a frank purpuric rash is argubly too late for ideal initiation. Early administration of pre-hospital antibiotics in the case of sepsis, which has been confirmed by the diagnostic criteria and lactate testing, can potentially save lives and reduce morbidity as well as reduce ultimate cost to the NHS. In the case of sepsis of unknown origin, a combination of antibiotics such as flucloxacillin, amoxicillin and gentamicin could be a suitable combination. These are drugs, which can be stored and used in an appropriate form for pre-hospital care, and provide a good spectrum of cover. Again, local discussion and agreement would be needed with microbiology teams.
