Some UK ambulance trusts have introduced an innovative paramedic role of critical care paramedic or advanced paramedic practitioner in critical care (APP). APPs are experienced paramedics who undergo additional training, including master's level education, which allows them to gain additional competencies in prehospital critical care (von Vopelius-Feldt and Benger, 2014). In the London Ambulance Service (LAS), APPs are targeted to the most seriously ill and injured patients, including those experiencing an out-of-hospital cardiac arrest (OHCA), with each APP attending on average 1.4 OHCAs per shift.
The primary focus of an APP is to ensure high standards in the delivery of resuscitation through on-scene leadership. APPs also provide enhanced decision-making and clinical interventions above those practised by paramedics. All APPs in the LAS are equipped with handheld ultrasound devices (HUDs).
Guidelines from the Resuscitation Council UK (2021) recognise the role of FoCUS in identifying futile resuscitations if used by skilled operators. However, it emphasises that assessing spontaneous cardiac motion (SCM) of the heart should not be used as the sole indicator.
There is a paucity of high-quality evidence to support the incorporation of FoCUS into prehospital guidelines (Quinn and Price, 2017). Moreover, a recent statement on the science from the International Liaison Committee on Resuscitation makes a weak recommendation, based on low-level evidence, against using point-of-care ultrasound in cardiac arrest (Reynolds et al, 2020).
It is increasingly acknowledged that intra-arrest ultrasound can detract from other essential elements of care, especially high-quality chest compressions (Gardner et al, 2018). Pauses in chest compressions are associated with a lower chance of survival (Deakin and Koster, 2016).
Recently, the European Society of Cardiology published a position statement on HUDs for FoCUS that acknowledges the potential for prehospital use, while outlining limitations to making quantifiable assertions with HUDs (Cardim et al, 2019). Training specifically in using these devices and in image acquisition and interpretation is also recommended.
The LAS deals with approximately 10 000 OHCAs per year, in which active resuscitation is attempted on just over 4000 patients. At the time of this study, 28 APPs working in the LAS receive one day of FoCUS training from an emergency physician, incorporating HUD practice. This is supplemented by further opportunities to refresh knowledge and practice during monthly training days.
LAS APPs have been using HUDs since May 2014, with the majority of use being in the context of pulseless electrical activity (PEA) OHCA. Local APP guidelines permit termination of a resuscitation in PEA and subsequent recognition of life extinct (ROLE) outside standard paramedic practice. A key element of this extended ROLE guidance is the absence of organised SCM on FoCUS.
APP guidance for termination of adult PEA cardiac arrest stipulates the following:
This study describes and evaluates APP use of FoCUS in OHCA and relates ultrasound findings with decisions to terminate resuscitation on scene or convey patients to an emergency department (ED). Additionally, the anatomical locations of the HUD probe are related to image findings.
Methods
Data collection
Patient characteristics collected were chosen a priori based on those widely reported in published literature on OHCA (Perkins et al, 2015; Cardiac Arrest Registry to Enhance Survival, 2017; Out-of-Hospital Cardiac Arrest Outcomes (OHCAO) Project Team, 2018).
The LAS maintains an electronic database that holds records of patients attended by APPs. The database was searched to identify all adult medical OHCA patients attended by any APP from 1 January 2018 to 31 December 2018, and results were tabulated. Patients obviously deceased on initial ambulance arrival were excluded.
Patients were divided into those conveyed to hospital and those for whom resuscitation was terminated (resulting in ROLE) on scene. All patients were identified as either having FoCUS or not, with reasons ascertained if a ROLE decision was made in the absence of FoCUS. For all those receiving FoCUS, probe positions and reported ultrasound findings were gathered.
In the database, FoCUS findings are recorded on a 1–5 scale by APPs: 1=no heart motion; 2=agonal uncoordinated movement; 3=hypokinetic; 4=normal; 5=hyperkinetic. To differentiate organised SCM from no SCM, only scores of 1 and 2 were recorded as no SCM during data analysis. SCM was assumed in patients who were recorded as 3, 4 or 5. This definition is in accordance with the local practice guidance and training.
Results
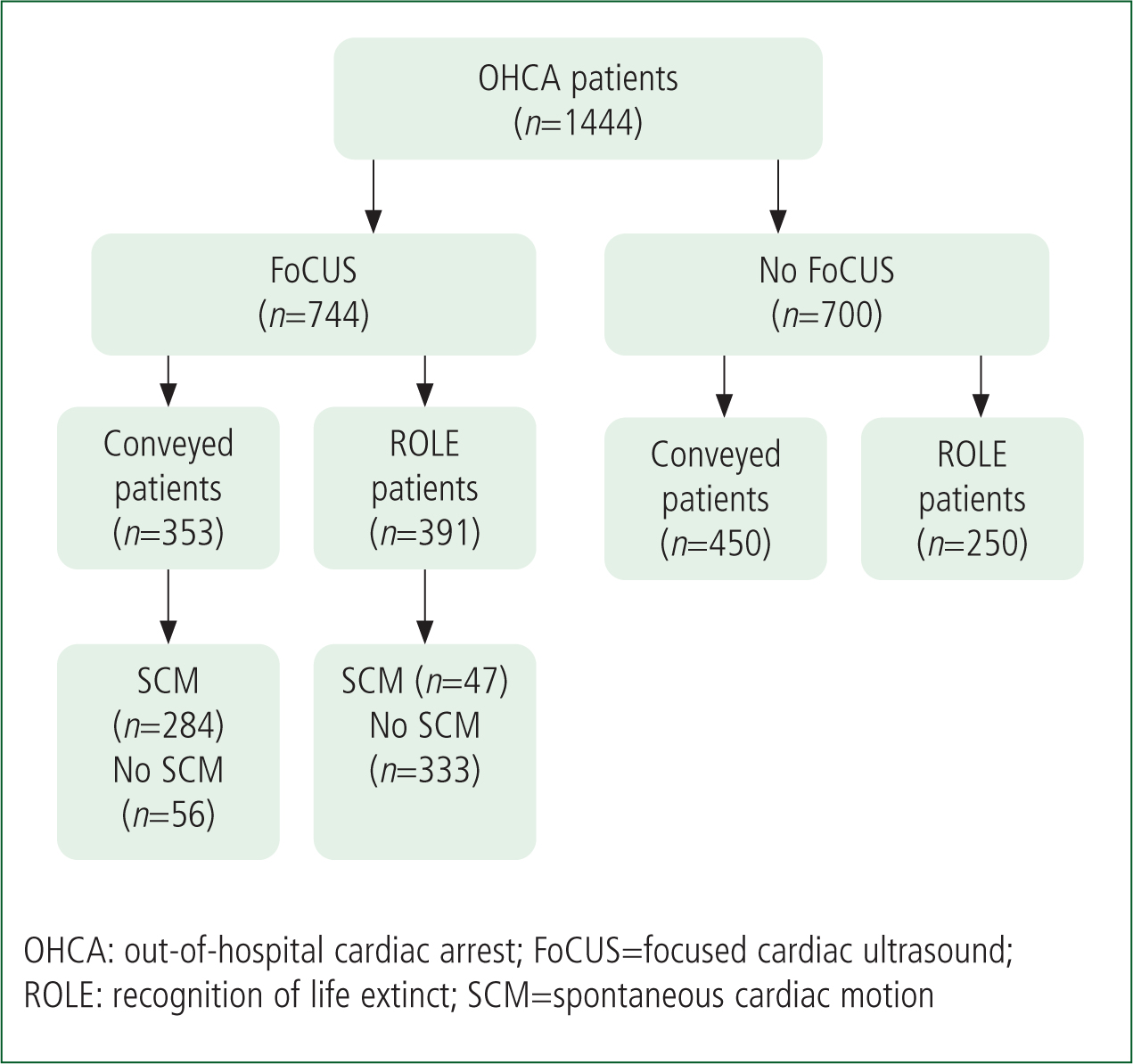
Of the total number of OHCA emergency calls attended by the LAS for 2018, 1444 were also attended by an APP. The numbers of patients who underwent FoCUS were similar to those who did not (744/1,444: 51%; and 700/1,444: 49% respectively). Patient flow is shown in Figure 1. An association was observed between conveyance and the identification of SCM, and ROLE and the absence of SCM. Characteristics of those who did and did not receive FoCUS are shown in Table 1.
| FoCUS | No FoCUS | ||
|---|---|---|---|
| Sex | Male | 507 (68.1%) | 481 (68.7%) |
| Female | 237 (31.9%) | 219 (31.2%) | |
| Age | Mean (SD) | 60.1 (16.78) | 56.5 (17.82) |
| Location | Public place | 233 (31.3%) | 282 (40.3%) |
| Private place | 511 (68.7%) | 418 (59.7%) | |
| Presenting rhythm | VF/VT | 237 (31.8%) | 214 (30.6%) |
| PEA | 239 (32.1%) | 170 (24.3%) | |
| Asystole | 266 (35.8%) | 279 (40%) | |
| Not known/recorded | 2 (<1%) | 37 (<1%) | |
| Disposition | ED | 353 (47.4%) | 450 (64.3%) |
| ROLE | 391 (52.6%) | 250 (35.7%) |
ED: emergency department; PEA: pulseless electrical activity; ROLE: recognition of life extinct; VF: ventricular fibrillation; VT: ventricular tachycardia
Probe position
Conveyed patients
FoCUS was used in 353 patients conveyed to hospital (Table 2). The most common finding in this group was SCM (284/353; 80.4%). No SCM was identified in 56/353 (15.9%) patients. On 13 (3.7%) occasions, the APP reported they were not able to ascertain any view.
| SC | PLAX | PSAX | Apical | Multiple | Total | |
|---|---|---|---|---|---|---|
| SCM | 213 (80.7%) | 53 (84.1%) | 4 (100%) | 5 (100%) | 9 (52.9%) | 284 (80.4%) |
| No SCM | 46 (17.4%) | 10 (15.9%) | 0 | 0 | 0 | 56 (15.9%) |
| No view | 5 (1.9%) | 0 | 0 | 0 | 8 (47.1%) | 13 (3.7%) |
Multiple=multiple probe positions; PLAX=parasternal long axis; PSAX=parasternal short axis; SC: subcostal; SCM=spontaneous cardiac motion
The view from the SC position was used most frequently (264/353; 74.8%) with 213/264 (80.7%) FoCUS attempts resulting in the identification of SCM. Using the subcostal (SC) view, 213/284 (75%) of SCM in the conveyed group as a whole were identified. Within the SC group, of the remaining 51 patients 46 (17.4%) were found to have no SCM; on five (<2%) occasions, no view was achieved.
The parasternal long axis view was the second most frequent probe position used, employed for 63/353 (17.8%) patients. Again, most attempts recorded in this group resulted in SCM being identified (n=53/63; 84.1%) with the remaining having no SCM (n=10/63; 15.9%).
Parasternal short axis and apical views were infrequent (four and five attempts respectively), and all were associated with SCM. Multiple views were recorded on 17 occasions and split between SCM (n=9) and no view (n=8).
Recognition of life extinct patients
Of 641 ROLE patients, 391 underwent a FoCUS attempt (Table 3). SCM was found to be absent in 333/391 (85.2%) patients. SCM was identified in 47/391 (12%) patients, leaving 11/391 (2.8%) where the APP reported being unable to gain a view. The absence of SCM was the most common finding for each of the four probe positions used.
| SC | PLAX | PSAX | Apical | Multiple | Total | |
|---|---|---|---|---|---|---|
| SCM | 36 (12.5%) | 8 (10.3%) | 3 (27.3%) | 0 | 0 | 47 (12%) |
| No SCM | 244 (85%) | 70 (89.7%) | 8 (72.7%) | 7 (100%) | 4 (50%) | 333 (85.2%) |
| No View | 7 (2.5%) | 0 | 0 | 0 | 4 (50%) | 11 (2.8%) |
Multiple=multiple probe positions; PLAX=parasternal long axis; PSAX=parasternal short axis; SC: subcostal; SCM=spontaneous cardiac motion
The SC view was used most frequently, in 287/391 (73.4%) procedures. Thirty-six of the 47 (77%) cases of SCM were recorded using the SC view. In 7/287 (2.5%) cases, no view was gained using the SC position.
The parasternal long-axis view was used less frequently than the SC view (in 78 versus 287 cases respectively). Absence of SCM was identified in 70/78 (89.7%) of FoCUS patients, representing 21% of the 333 no SCM cases recorded overall. All attempts made via this view resulted in a recordable image. The parasternal short-axis and apical views were used infrequently at 3% (n=11) and <2% (n=7), respectively, of all FoCUS attempts made in ROLE patients. SCM was identified using the parasternal short axis view on three occasions and all apical views returned findings of no SCM.
Multiple views were recorded in only eight out of the 391 (2%) patients. This category was used when an APP had used more than one view but not specified the most useful view.
Prognostication
Figure 2 shows that FoCUS was not performed on 250 (39%) of the 641 patients who had a ROLE decision. Nearly all (247; 98.8%) of these patients are recorded as having a valid documented reason for a ROLE decision. The most common reason was asystole, recorded in 186 (74.4%) patients. Late identification of signs unequivocally associated with death occurred in 26 (10.4%) patients. These occasions involved an APP arriving to support emergency medical services (EMS) crews who had already started resuscitation. In 22 (8.8%) cases, a doctor was on scene and made a ROLE decision. A senior on-call clinician (consultant paramedic/doctor) was consulted by telephone in eight (3.2%) of the 250 cases and approved a ROLE decision. Late identification of a valid DNA CPR (do not attempt cardiopulmonary resuscitation) was the documented reason in five patients. In three cases, records were incomplete.
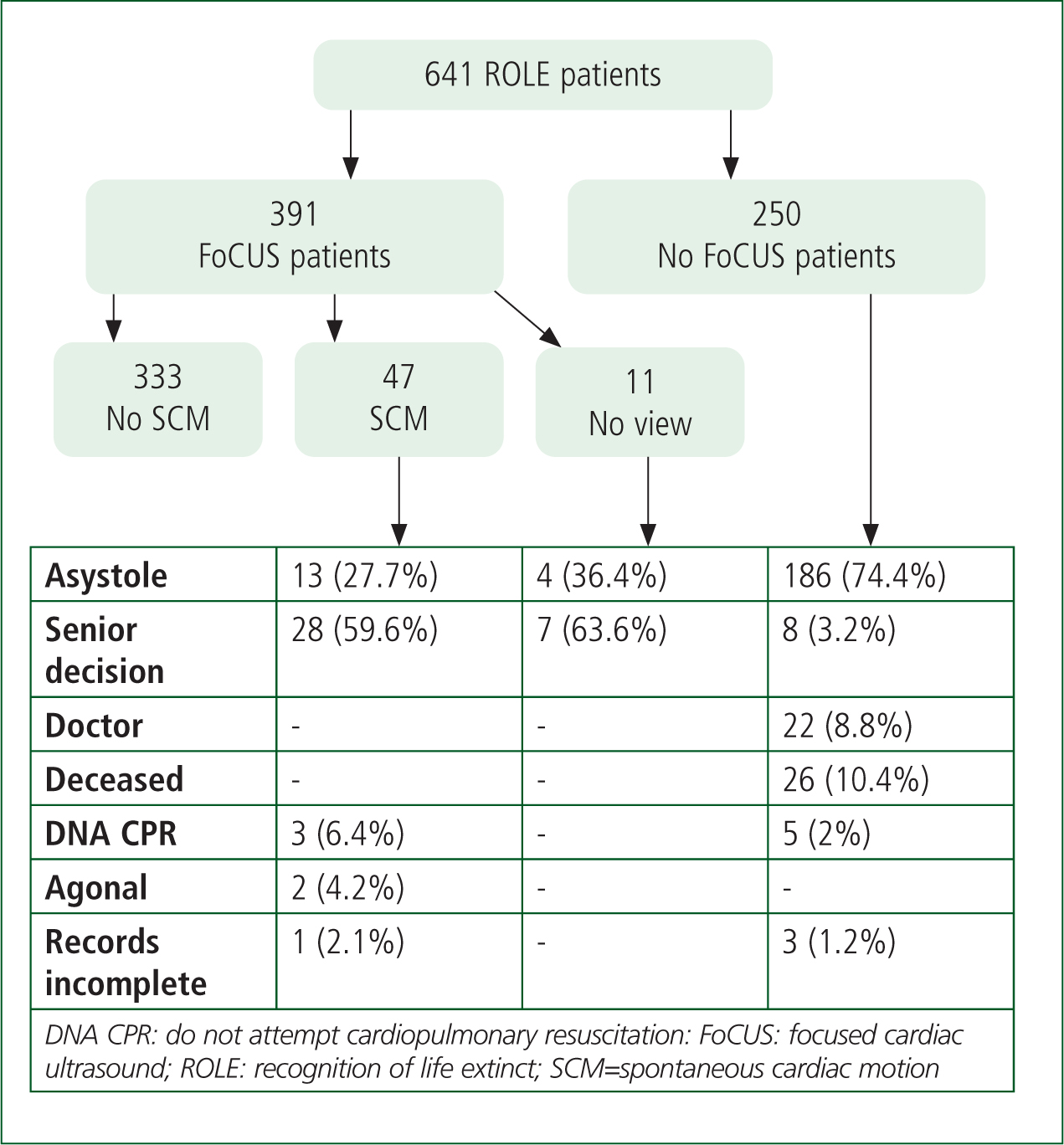
For patients who had a ROLE decision after a FoCUS attempt, 333/391 (85%) had no SCM, and the decision was accordant with guidelines. However, 47/391 (12%) of patients had SCM reported. Of these, 28 (59.6%), had a ROLE decision following consultation with the on-call senior clinician. Thirteen patients (27.7%) became asystolic after a FoCUS attempt, allowing a ROLE decision within standard guidance. In a further two cases, the APP had recorded ‘agonal’ heart activity, allowing for a ROLE because there was no organised SCM. In three cases, a DNA CPR became apparent after resuscitation had begun. In one case, records were not complete.
No view was achieved in 11 (2.8%) patients of the 391 for whom a FoCUS attempt was made before a ROLE decision. Seven of these were referred to the senior on-call clinician and four subsequently became asystole.
Discussion
The majority of patients presented in a private environment and were male, which is consistent with previous reports describing large UK OHCA populations (OHCAO Project Team, 2018; Perkins et al, 2018). However, the APP OHCA patient cohort is younger (with a mean age of 58.4 years) than those other populations (with a mean age of 63.5 years). As recognised in the literature, this may reflect the selective criteria employed to target critical care resources to patients thought to have a higher likelihood of survival (von Vopelius-Feldt and Benger, 2014). Greater age has been associated with poorer outcomes (OHCAO Project Team, 2018).
Because there is a dearth of literature describing the characteristics of patients receiving prehospital FoCUS, it is not possible to make meaningful comparisons. In our series, 10% more patients underwent FoCUS in private than public locations. FoCUS was primarily used in the context of ROLE decisions and it is possible that more patients were conveyed to hospital from a public place because of the problems of leaving deceased patients in more communal settings. Additionally, bystander CPR may be more frequent when OHCA occurs in a public rather than in a private location, generating more ROSC patients and conveyances. Survival from OHCA in public environments has been reported as higher (OHCAO Project Team, 2018).
According to LAS data for 2017–2018 (LAS NHS Trust, 2018), an APP is more likely to attend a patient who is in a shockable rhythm than most paramedics (31% versus 20.3%). This finding has implications for survival and therefore conveyance to an ED. Again, this difference might be because of preferential APP dispatch to witnessed OHCA.
FoCUS was performed most often in the PEA group in the present study. In a meta-analysis by Gaspari et al (2016), a similar proportion of patients presenting with PEA underwent FoCUS—225 out of 414 (54%)—with 38 out of 327 (12%) presenting asystole. This contrasts with a meta-analysis by Tsou et al (2017), who reported that asystole accounted for most FoCUS (n=819; 48%), followed by PEA (n=591; 35%), then shockable rhythm (n=196; 12%).
SC is the view used most frequently by APPs, accounting for 74%. SC view is the most easily accessible during cardiac arrests (Breitkreutz, 2018). Probe positions used for the parasternal long- and short-axis views inevitably interfere with chest compressions. Although images can be gained during chest compression pauses, the safe, effective and timely resumption of compressions may be hampered by the application of ultrasound gel to the chest. Furthermore, when mechanical CPR is performed using the LUCAS-2TM device by APPs, the device may form a physical barrier to the anterior chest wall. The apical view requires placing the patient in a left lateral position to optimise images (Sloan, 2018) and is not practical during resuscitation.
The parasternal long-axis view was preferred in 19% of patients, with parasternal short-axis and apical views used infrequently (3.6%). Given the nature of the dataset, the authors were unable to explore the rationale for decisions to use one probe position over another or why a view may have been gained with one probe position but not another.
Other than where an SC view produced no view, the appeal of the parasternal long axis may be that it provides more anatomical detail over the parasternal short axis. The parasternal short axis is predominantly concerned with imaging left ventricular contractility (Sloan, 2018). It is also worth considering that FoCUS may not have always been undertaken during periods of chest compressions, therefore allowing easier access to the anterior chest wall. Local guidance allows APPs to choose probe position.
No image was obtained in 24 out of 744 (3.2%) patients. This is a lower proportion than that reported by other studies exploring paramedic use of ultrasound (Heegaard et al, 2010; Rooney et al, 2016; Reed et al, 2017).
SCM was reported in the majority of conveyed patients, while an absence of SCM was reported in the majority of the ROLE group (85%). However, 16% of patients with no SCM were still transported to hospital. Gaspari et al (2016) reported that three patients in their cohort survived to hospital discharge having had no SCM. Decision-making in OHCA is multifactorial and decisions to convey may involve patient location, family wishes, reversible causes and ease of extrication so APPs are not making ROLE decisions based solely on the absence of SCM.
Despite the strategy of targeting APPs to OHCAs having been deemed more viable, the proportion of ROLE decisions made by APPs (44.3%) was fractionally higher than that for the ambulance service as a whole (43.8%), perhaps indicating that APPs enact ROLE in situations where standard paramedic practice does not. It is plausible that, without APP involvement, many futile resuscitation attempts might continue and result in unnecessary transportation of patients to hospital under emergency conditions. This might have implications for an otherwise dignified death at home, as well as regarding practical considerations around extrication while maintaining high-quality CPR. Increased risk to EMS personnel and other road uses during emergency journeys has been recognised (Grundgeiger et al, 2014); therefore, only essential blue light journeys should be undertaken.
Limitations
Limitations include the retrospective, observational nature of the study. All findings are descriptive, highlighting associations but not causation. Chronology is not explored and survival data are not reported.
Additionally, reporting bias is conceivable because of the lead author's status as an APP and investigator in the EMS system concerned. All image findings were reported and not subject to expert review.
Conclusion
The authors believe this is the largest prehospital study involving FoCUS in OHCA. In this cohort, an association was found between patients receiving ROLE decisions with FoCUS findings of no SCM, and an association between FoCUS findings of SCM and patients being conveyed to hospital.
The SC view was the most used view and ROLE decisions were deemed to be accordant with local guidance and practice. Further prospective study of prehospital FoCUS involving the independent verification of recorded images is recommended.

