The Association of Ambulance Chief Executives (AACE) (2013)Clinical Practice Guidelines provide a clear algorithm for practitioners when considering whether spinal immobilisation of a patient is warranted. However, they further state that ‘suspicion of thoracic and lumbar injury despite a cleared cervical spine warrants full immobilisation.’ Consequently, the onus of any clinical decision made is firmly based on the individual practitioner's judgement. Additionally, Connor et al (2013) assert in a consensus statement on behalf of the Faculty of Pre-hospital Care that ‘a change is needed from a policy of immobilising necks, as much for the protection of the clinician as for that of the patient.’ They also state thatlong spinal boards should only be used as an extrication device and that a clear algorithm should be adopted for identifying spinal cord injury (SCI).
Both AACE (2013) and Connor et al (2013) recognise that spinal immobilisation has a basis in history of logical principles as opposed to evidence-based practice. Although there is some historical literature supportive of spinal immobilisation (Chiles and Cooper, 1996), a key review of current literature on spinal immobilisation (Kwan et al, 2001) stated that there was a lack of high-quality primary research in the area, and that the effects of spinal immobilisation were unclear in relation to both reducing SCI and reducing mortality.
This review will endeavour to highlight the available research relating to current controversies in pre-hospital spinal immobilisation. It will also consider mortality rates between those who receive pre-hospital spinal immobilisation and those who do not.
Background
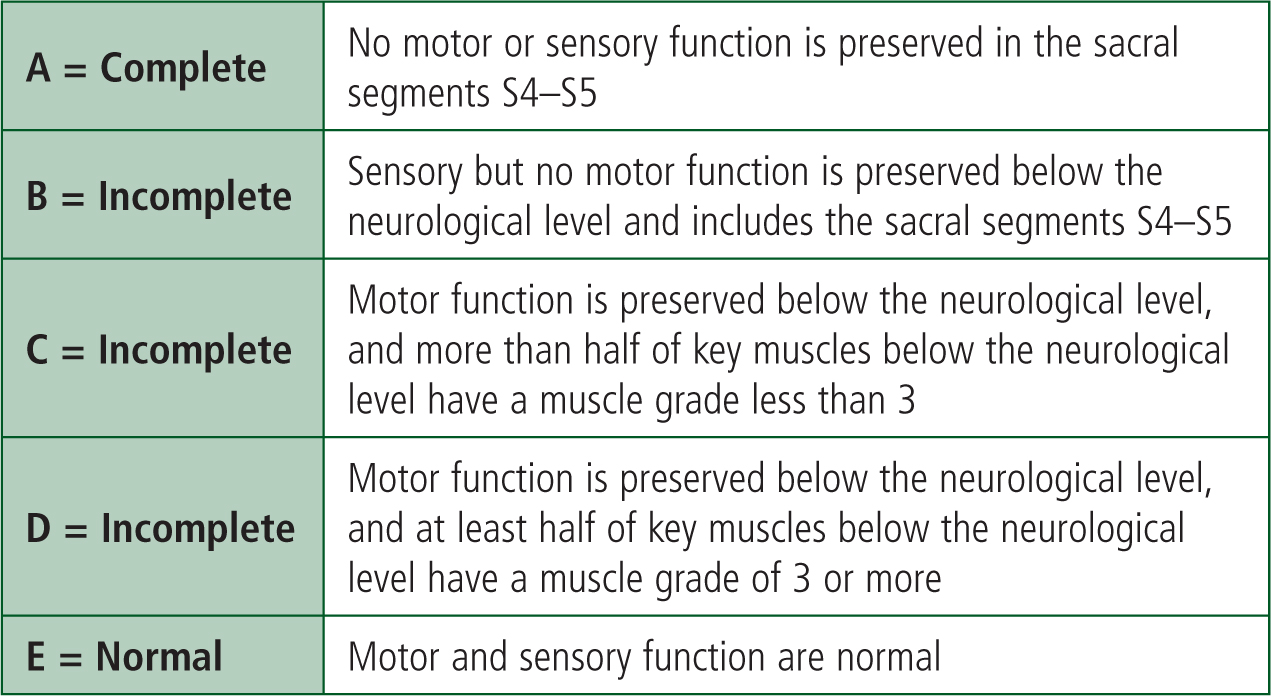
Porth and Matfin (2008) describe SCI as damage to the neural elements of the spinal cord. SCIs are commonly classified using the American Spinal Injury Association (ASIA) Impairment Scale (Figure 1) in order to give an indication of the level of neurological damage.
Wyndaele and Wyndaele (2006) reported that the incidence of SCI lies somewhere between 10.4 and 83 incidences per million inhabitants per year (between 10.4 and 29.7 per million per year in Europe). They did, however, acknowledge that SCIs are generally poorly reported throughout the world, with a lack of consistent classification criteria. They also acknowledged that it is likely that the true figures are higher than those reported.
In Western Europe the most common causes of traumatic SCIs are: land transport (46%), falls (35%), work-related accidents (18%), violence/self-harm (8%), and sports-related injuries (2%). There is also a prospective reported mortality rate of 18% in the first 10 years in Europe (Lee et al, 2013).
In a study of US Veterans, French et al (2007) reported the initial 1-year cost of SCI to be between $218 000 and $741 000 (£140 000 to £475 000) per patient (depending on the degree of injury), with long-term costs running at an average of $21 450 annually. Given the irreversible nature (at present) of SCI and the high treatment costs, effective prevention and treatment of SCI must be a priority.
Current spinal immobilisation techniques
Guidelines set out by AACE (2013) state that where spinal immobilisation is indicated the whole spine must be immobilised and the only two acceptable methods for spinal immobilisation are: ‘1. Manual immobilisation where the back is supported; 2. Collar, head blocks and back support.’
There are several techniques that can be used to immobilise the spine, these include, but are not limited to, long extrication boards, vacuum mattresses and scoop stretchers.
Literature review
Search methodology
A primary literature search was undertaken using the Cochrane Library, MEDLINE, CINAHL, Google Scholar and Science Direct databases. Following this a secondary search of systematic reviews, non-systematic reviews and meta-analyses found in the primary literature search was undertaken looking at any relevant primary research cited.
Main search terms used were ‘spinal immobilisation’, ‘spinal immobilization, and ‘spine board’. Initially these were the only terms used; however, when there was a large volume of research, further relevant search terms were added to reduce the volume of research presented. These included: ‘pre-hospital’, ‘paramedic’ and ‘ambulance’ AND/OR Boolean phrases were used to further limit terms, as well as including date ranges from circa 2005–present.
Inclusion criteria
A hierarchical approach based around quality of methodology (Hamer et al, 2005) was taken when deciding upon the inclusion of primary research. Randomised control trials (RCTs) were given preference followed by Cohort studies, and finally, retrospective studies and opinion-based/qualitative research.
As the aim of this review is to look at SCI and mortality from a global perspective, it was decided to include studies looking at a broad range of issues relating to spinal immobilisation. By increasing the scope of the literature search this study should provide a more holistic view of spinal immobilisation as a concept, as opposed to focusing on an isolated issue.
Primary research results
Following a comprehensive literature search (Appendix 1), 13 pieces of primary research were selected for inclusion (Table 1). Despite a stated preference for RCTs, it proved difficult to find RCTs undertaken with anyone other than healthy volunteers. It is likely that this is due to the difficulties, both practically and ethically, of undertaking studies on real patients with potential SCIs.
| Authors | Article name | Type of study | Participants | Intervention | Outcome measures | Results | Limitations |
|---|---|---|---|---|---|---|---|
| Cooke, 1998 | use of the spinal board within the accident and emergency department | Questionnaire | 50 questionnaires sent to A & E consultants and specialist trainees in the West Midlands with 35 (70%) respondees | NA | Percentage who had a spinal board in department, time at which consultants would remove a spinal board, preferred method of immobilisation, preferred method of patient transfer, perceived problems of spinal immobilisation | 88% had a spinal board in department. 91% would wait until after a primary survey, initial resus and a primary X-ray. 20 respondees listed pressure sores as a potential complication along with 20 stating boards were uncomfortable | All qualitative therefore entirely opinion based. Small sample. Age of research (although still relevant as Advanced Trauma Life Support guidelines are still similar) |
| Hauswald et al, 1998 | Out-of-hospital spinal immobilization: its effect on neurologic injury | Retrospective patient analysis | 120 Malaysian trauma patients WITHOUT spinal immobilisation and 334 American trauma patients WITH spinal immobilisation | NA | Incidence of disabling and non-disabling neurologic injury | Unimmobilised Malaysian patients were less likely to experience neurologic injuries than those in America who were immobilised. | Differences in demographic cause of injury (RTC versus falls). Small sample sizes |
| Jin et al, 2007 | A retrospective study of five clinical criteria and one age criterion for selective prehospital spinal immobilization | Retrospective patient analysis and application of criteria | 238 blunt trauma victims with spinal injury | Five clinical criteria were applied retrospectively:
|
Sensitivity of the immobilisation criteria to previous patients | 99.2% of patients would have been immobilised had the selective criteria been applied | Did not account for over immobilisation of patients |
| Peery et al, 2007 | Prehospital spinal immobilisation and the backboard quality assessment study | Immobilised non-critically ill patients | 50 Subjects | NA | Number of straps missing, too much slack 2cm | 30% had at least one unattached strap with 80% having more than 2cm of slack between them and the board | No indication of quality of immobilisation for more seriously injured patients. No certainty that poor immobilisation affects outcome |
| Sheerin and De Frain, 2007 | The occipital and sacral pressures experienced by healthy volunteers under spinal immobilization: a trial of three surfaces | Randomised control trial | Convenience sample of twp healthy volunteers | Subjects were fitted with a rigid cervical collar and then were sequentially placed on |
Pressure (mmHg) experienced at occiput and sacrum | Pressures with a long spinal board were higher than with a raft device or full body vacuum device | Very small sample size. No statistical analysis. Does not comment on the efficacy of each method at its primary purpose (spinal immobilisation) |
| Brown et al, 2009 | Prehospital spinal immobilization does not appear to be beneficial and may complicate care following gunshot injury to the torso | Retrospective patient analysis | 75 567 from National Trauma Data Bank and Strong Memorial Hospital | NA | Clinical outcome for patients | No subjects with SCI improved or deteriorated. Pre-hospital spinal immobilisation would not benefit subjects, as where SCI occurs in gunshot injuries to the torso, it is due to direct insult to the cord | Retrospective analysis, therefore no cause and effect. Does not state whether subjects immobilised had better overall outcome or worse |
| Ramasamy et al, 2009 | Learning the lessons from conflict: pre-hospital cervical spine stabilisation following ballistic neck trauma | Retrospective patient analysis | 90 British military casualties with penetrating neck injury | NA | Number of patients with a penetrating neck injury who had cervical spine injury and number who survived to discharge | Of the 90 patients, 20 (22%) had cervical spine injuries, none of which survived to discharge | Spinal immobilisation of subjects did not occur, therefore it is difficult to say whether spinal immobilisation would have altered outcome |
| Vanderlan et al, 2009 | Increased risk of death with cervical spine immobilisation in penetrating cervical trauma | Retrospective patient analysis | 159 Patients | NA | Patients with penetrating cervical trauma had their charts retrospectively analysed and mortality rates were compared between patients who were and were not C-spine immobilised | C-spine immobilisation was associated with an increased risk of death (p=0.0016), with most patients dying in the emergency department presenting with pulseless electrical activity associated with exsanguination or hypoxia. | Large numbers of charts destroyed by Hurricane Katrina. Unable to determine causality |
| Stone et al, 2010 | The effect of rigid cervical collars on internal jugular vein dimensions | Prospective volunteer study | 42 healthy volunteers | A rigid cervical collar was applied | Internal jugular vein measurement were obtained pre and post rigid cervical collar immobilisation | The mean cross-sectional area of the right internal jugular vein was 0.70cm2 without the rigid cervical collar and 0.89cm2 after placement of the collar: the cross-sectional area of the internal jugular vein increased significantly (p<0.0001) after application of the cervical collar | Healthy volunteers and only one cuff size used. No definitive proof that internal jugular vein pressure is directly linked to intracranial pressure |
| Lin et al, 2011 | Neck collar used in treatment of victims of urban motorcycle accidents: over or under protection? | Retrospective patient analysis | 5 139 Patients admitted to a Taiwanese hospital following motorcycle accidents | NA | Comparison of outcome for those who were and were not immobilised in the pre-hospital setting | 0.73% had spinal injuries. There was no significant difference in likelihood of SCI between the two groups. Average length of stay in ICU was slightly longer in the group who had a collar applied but total length of stay was no different | Sample taken from only one hospital therefore could not be representative. A retrospective study with large amounts of incomplete data (50%) |
| Leonard et al, 2012 | Potential adverse effect of spinal immobilization in children | Retrospective patient analysis | 285 Children (173 immobilised and 112 not immobilised but met guidelines) | NA | Median pain score, cervical radiography undertaken, admission to hospital | Immobilised children had a higher median pain score (3 versus 2) and were more likely to be admitted to hospital | Some differences between the two patient groups. No way of telling if the higher pain score was related to immobilisation |
| Dixon et al, 2015 | Confirmation of suboptimal protocols in spinal immobilisation? | Biomechanical analysis | Four trained firefighters, two paramedics | Six different methods of extrication were used, three involved long spinal board, one used a short extrication jacket and two self-extrication protocols (C-spine collar and no collar) | Volunteer movements were captured using 3D motion analysis cameras and reflective markers to calculate total patient movement | Self-extrication led to a mean movement of 13.33°, in comparison to long board techniques, which ranged from 13.56–18.84° | Some findings were not statistically significant with relation to the degrees of movement found |
| Paterek et al, 2015 | Characteristics of trauma patients over immobilized by prehospital providers | Retrospective patient analysis | 76 patients in an 18–month period | NA | Analysis of patients deemed ‘over immobilised’ and the rationale behind their immobilisation by pre-hospital providers. | 12 patients were deemed over immobilised. In conversation with the practitioners who overimmoblised, it became clear there was too much focus on mechanism of injury and practitioners' fears of ‘missing something’ were apparent | No patient outcome data recorded, no way of knowing if there was an adverse effect on patient outcome |
Despite a lack of good quality RCTs, there was, however, a large volume of research available (Table 1).
Secondary research results
Further to the primary research, four pieces of secondary research were also selected for inclusion (Table 2). These focused on the efficacy of immobilisation in healthy subjects as well as the effects of immobilisation in trauma patients. All the reviews drew on a wide range of research and where possible attempted to draw conclusions and give recommendations for further research.
| Authors | Article name | Research questions | Search strategy | Number of papers | Conclusions | Recommendations |
|---|---|---|---|---|---|---|
| Kwan et al, 2001 Spinal | immobilisation for trauma patients (Review) | To quantify the effect of different methods of spinal immobilisation on mortality, neurological disability, spinal stability and adverse effects in trauma patients | Search of CENTRAL, MEDLINE, Embase, CINAHL, PubMed, National Research Register and Zetoc looking for RTCs | Not stated | No suitable research was found for inclusion | Large scale RCTs are required to establish the relative effectiveness of spinal immobilisation in trauma patients |
| Kwann and Bun, 2005 | Effects of prehospital spinal immobilization: a systematic review of randomized trials on healthy subjects | To evaluate research on different spinal immobilisation methods tested on healthy subjects | MEDLINE, EMBASE, CINAHL and Cochrane Library searched for RCTs that met specific inclusion criteria | 17 | The devices tested were relatively effective at immobilising the spine; however, there were a number of adverse side effects including increased ventilatory effort, pain and ischaemia | Immobilisation devices are effective in reducing spinal mobility; however, they are also associated with adverse effects. RCTS in trauma patients need to be considered to establish their practical efficacy |
| Abram and Bulstrode, 2010 | Routine spinal immobilisation in trauma patients: what are the advantages and disadvantages? | To critically discuss the evidence surrounding routine spinal immobilisation | Search of MEDLINE | 0 | Pros: some patients with missed SCIs have further deteriorated due to missed diagnosis. Cons: ankylosing spondylitis, delayed resuscitation, raised intracranial pressure, increased difficulty of airway management | There are high volumes of patients being unnecessarily immobilised, immobilisation may increase mortality and more effective criteria for selective immobilisation need to be looked into |
| Ahn et al, 2011 | Pre-hospital care management of a potential spinal cord injured patient: a systematic review of the literature and evidence-based guidelines |
|
Search of Embase, MEDLINE, CINAHL and Cochrane databases, with eligible studies rated on the Downs and Black checklist | 47 |
|
SCI Immobilisation should involve a collar, head immobilisation and a spinal board; however, patients should be removed from the board as soon as possible. Intubation methods should still be used; however, indirect methods may be preferable. Pre-hospital care providers can effectively use algorithms to clear patients with suspected C-spine injuries. There are, however, problems with real worldapplication |
Discussion
The research selected for this study falls into three broad areas: principal effectiveness of spinal immobilisation at its primary purpose, secondary side effects, and overall patient outcome.
Principal effectiveness
The most fundamental consideration with regards to spinal immobilisation should be whether it is principally effective at immobilising the spine and preventing movement. On investigation, however, there was limited recent research into their principal effectiveness, with many studies using dated methodologies to quantify effectiveness. Kwann and Bunn (2005) reported that immobilisation devices were largely effective at reducing cervical spine movement. A major flaw, however, was that they only looked at cervical spine movement in situ on a board and did not reference any studies that looked at the degree of movement required to effectively place someone onto an immobilisation device. This was investigated by Dixon et al (2015), who undertook a biomechanical investigation looking at the degrees of movement required to remove a subject from a car using six different techniques, including self-extrication. They found that self-extrication led to a mean of 13.33° of movement in comparison to means of between 13.56° and 18.84° using manual extrication techniques. There were limitations to the study, however. With only 16 participants in each category, the study was insufficiently powered to demonstrate any statistically significant findings; participants had a narrow age range (18–40 years) meaning it is unclear how this information could be applied to other populations (e.g. the elderly).
A secondary consideration with regards to whether spinal immobilisation reduces cervical spine movement is that devices are used and applied correctly. This may, however, not always be the case. Peery et al (2007) investigated the quality of spinal board immobilisation of 50 non-critically ill patients at an American hospital. They found that 80% of patients had more than 2cm of slack on their straps with 30% having at least one unattached strap. As this study only investigated non-critically ill patients, it is impossible to say whether patients who were critically ill were immobilised to a greater degree due to more care been taken, or a lesser degree given the perceived need for rapid extrication.
Potential side effects
There are a number of well documented side effects of spinal immobilisation, particularly in relation to pain experienced while immobilised (Leonard et al, 2012). A further side effect is pressure ulcers. With pressure ulcers leading to a potential 7–8% increase in mortality (Byrne and Salzberg, 1996), they are an important consideration when deciding whether to immobilise a patient and what device to use. In a small sample study, Sheerin and de Frein (2007) found that occipital and sacral pressures were lower when flotation devices or vacuum mattresses were used. A broader review of the current literature by Ahn et al (2011) also supported these findings, reporting scoop stretchers as more comfortable for patients and recommending that patients be kept fully immobilised for the least amount of time possible. This is complimented by the Faculty of Pre-Hospital Care of the Royal College of Surgeons of Edinburgh (Connor et al, 2013) and AACE (2013), who both state that traditional long spinal boards should only be used as extrication devices and not immobilisation tools. It would appear, therefore, that with further research, flotation devices and vacuum mattresses could become a valuable method of reducing pressure sores associated with immobilisation.
A further less well documented but potentially more severe side effect of spinal immobilisation is raised intracranial pressure (ICP). This can be caused by a number of factors including localised lesions (e.g. traumatic haematomas), disturbance of cerebrospinal fluid circulation, obstruction of major venous sinuses (e.g. depressed fractures), or diffuse brain oedema/swelling (Dunn, 2002). Miller et al (1981) identified that raised ICP was the leading cause of death in patients suffering traumatic brain injuries. As patients suffering traumatic brain injuries in the pre-hospital setting are likely to be immobilised, it is important that spinal immobilisation does not increase ICP and put patients at further risk.
Stone et al (2010) investigated the effect of cervical collars on internal jugular vein dimensions (used as an indicator of ICP) and found that internal jugular vein dimensions increased a significant amount after collar placement. They speculated that this demonstrated cervical collars increased ICP. However, there is no definitive proof that internal jugular vein dimensions are directly linked to intracranial pressure.
Overall patient outcome
Having considered different measures of efficacy for the use of spinal boards, consideration must be given in relation to the overall outcome for patients who are immobilised versus those who are not. There is a dearth of good-quality research in this area for a variety of reasons, not least the ethical difficulties of conducting RCTs in this field. Consequently, the majority of research undertaken has been retrospective patient analysis.
In a seminal piece of work, Hauswald et al (1998) compared patients presenting at two hospitals, one in Malaysia, where spinal immobilisation was not practised, and one in New Mexico, America, where spinal immobilisation was practised as a standard procedure. After a comparison of 120 Malaysian patients and 334 American patients, somewhat surprisingly, Hauswald et al found that patients who were not immobilised were less likely to suffer a neurological injury than those who had been immobilised. This was further supported by Lin et al (2010), who reported that there was no significant difference in outcome between those who were and were not immobilised following motorcycle accidents inTaiwan.
Further to this, research by Brown et al (2009) reported that in cases of gunshot injury to the torso, spinal immobilisation was not beneficial, as it delayed treatment for those without SCI. For those with SCI, neurological damage was done on impact and did not worsen without immobilisation. Similarly, Ramasamy et al (2009) reported that in ballistic trauma to the neck SCI was unlikely, and that the risk reward ratio of spinal immobilisation was unfavourable.
‘There is a plethora of research available on spinal immobilisation looking at a broad range of topics. However, with limited high-quality research available, it is difficult to draw definitive wide-ranging conclusions from the research available’
Summary of current controversies
There is a plethora of research available on spinal immobilisation looking at a broad range of topics. However, with limited high-quality research available, it is difficult to draw definitive wide-ranging conclusions from the research available. What is clear, however, is that there are notable areas on controversy in relation to the current practice of full spinal immobilisation.
With this in mind the key controversies appear to centre on the following areas:
One of the most important premises of spinal immobilisation is that it is more effective than no intervention and that it is fundamentally effective in its primary role of reducing spinal movement. However, as of yet, there is insufficient research to support this position. This is an area of primary importance and although there is a large volume of research available on the secondary complications of spinal immobilisation, further research needs to be carried out to investigate the efficacy of spinal immobilisation in its fundamental role of immobilising the spine.
Further to research into the fundamental effectiveness of spinal immobilisation, high-quality RCTs are required to determine cause and effect. Lack of clarity regarding the circumstances in which spinal immobilisation constitutes best practice will hopefully trigger further research.
Implications for practice
Key Points
Conflict of interest: none declared

