Tourniquets are one of the earliest medical devices to stop active haemorrhage, dating back approximately three millennia (Richey, 2007; Taylor et al, 2011). The device rapidly stops arterial and venous blood flow distally to the application site. Historically, tourniquets were primarily used by military personnel, who shaped their initial development (Mabry, 2006). Despite this, in 1962, Klenerman (1962) supported their discontinuation because studies suggested ‘ineffectiveness’ or ‘harmful’ side effects. This subsequently became a part of international guidelines on haemorrhage control (Giannou and Baldman, 2009). This shift in opinion was in part because research and data confirming a benefit to mortality were limited, and anecdotal evidence suggested possible ischaemic and neurovascular complications.
Two pieces of epidemiological research led by Bellamy (Bellamy, 1984; Bellamy et al, 1986) sparked the reissuing of tourniquets for military use. The studies evaluated data from the Vietnam war to ascertain causes of death. The data showed that many deaths were from exsanguination. As a result, Butler et al (1996) promoted rapid application of tourniquets during combat.
Extremity trauma and subsequent haemorrhage continued to be the leading cause of death during the Iraq and Afghanistan wars. This encouraged further development in primary haemorrhage control (Butler et al, 1996; Holcomb et al, 1998; 2007; Calkins et al, 2000; Mabry et al, 2000; Beekley et al, 2008; Kragh et al, 2008), which led to the issuing of tourniquets to all frontline US military staff (Walters and Mabry, 2005; Wenke et al, 2005; Mabry, 2006).
Further research confirmed the benefit of this protocol change (Kragh et al, 2009; 2011; Kragh, 2010). Beekley et al (2008) reported that 57% of military deaths in Iraq were potentially preventable with tourniquet use. One of the largest studies was that by Lakstein et al (2003), who retrospectively reviewed 550 patients requiring tourniquet application and concluded that application was highly effective at managing haemorrhage.
Because of the tourniquet's apparent success, the American College of Surgeons Committee on Trauma now recommends the use of tourniquet devices for civilian application. Current UK guidelines mirror this, suggesting a step-wise approach to haemorrhage control, with the tourniquet being a last resort (Wolff and Adkins, 1945; King et al, 2006; Joint Royal Colleges Ambulance Liaison Committee (JRCALC), 2016; National Institute for Health and Care Excellence (NICE), 2017). This recommendation, however, is arguably based on the assumption that military research is directly transferrable to the civilian setting, where training, injury patterns and logistical pressures are all different from those seen in the military. The benefits of tourniquet use in the civilian setting are under-reported, with limited civilian research assessing its utility, and little originating in the UK.
The aim of this systematic review is to assess whether tourniquets are a beneficial intervention to manage extremity haemorrhage in the civilian prehospital setting. The specific objectives are to:
It is hypothesised that tourniquet use by UK paramedics in the management of non-compressible prehospital catastrophic haemorrhage is associated with improved outcome.
Methodology
Ethical approval
Ethical approval was not required for the completion of this systematic review.
Search strategy
The US National Library of Medicine was used to ascertain MeSH terms for inclusion in the literature search. The following search terms were included:
After the initial OR searches, results were combined with AND.
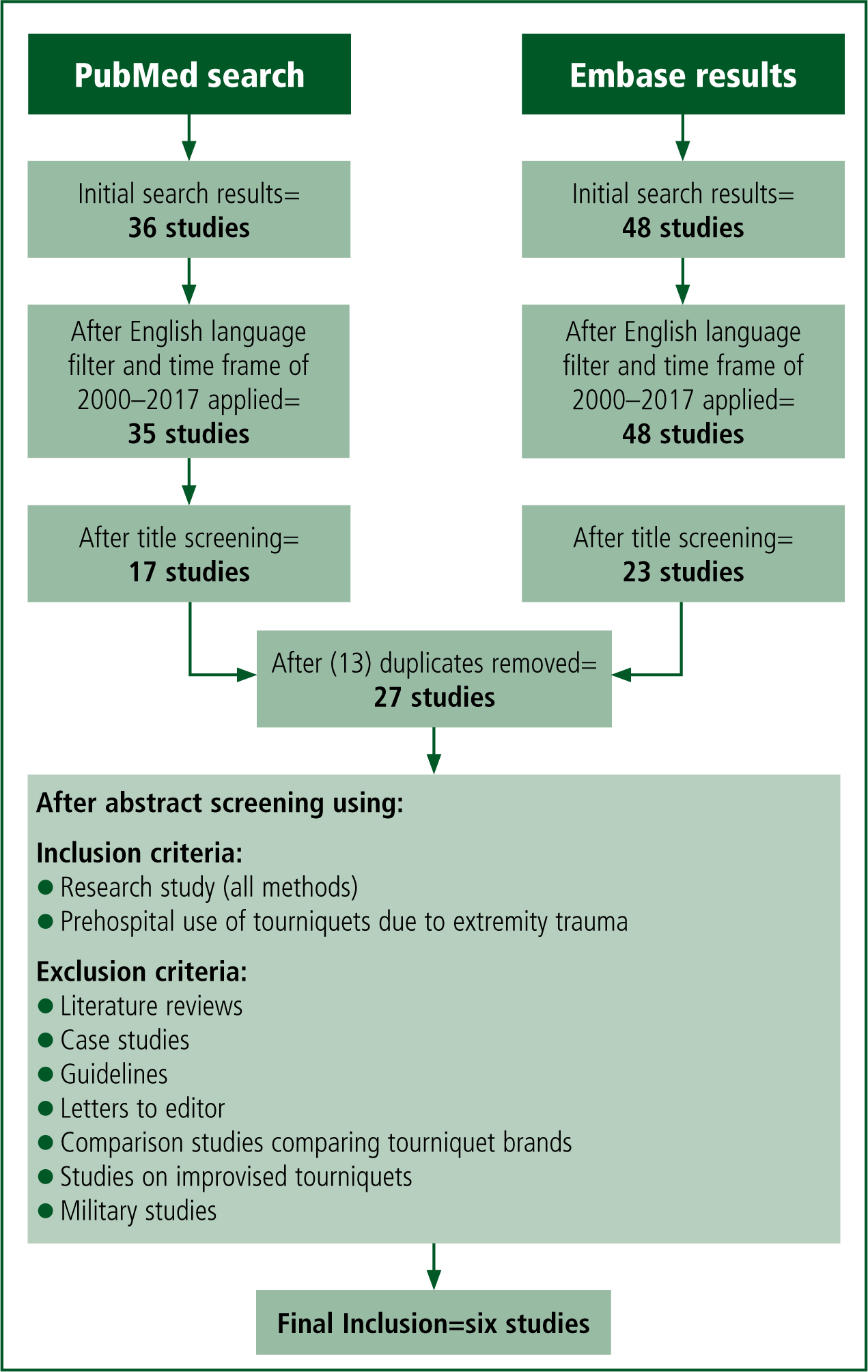
The literature searches were carried out using the PubMed and Embase databases. An English language filter was applied as there was no funding for translation, as well as a publication time frame of 2000–2017 to ensure inclusion of relevant and contemporary research.
Selection criteria
Abstracts of the resulting research were screened for relevance based on the following criteria.
Inclusion criteria
Exclusion criteria
The full, final six studies were then reviewed to confirm relevance (Table 1). The reference lists of the final selected studies were then examined to ascertain if any pertinent studies that met the inclusion criteria had been overlooked.
| Study | Study design | Levels of evidence | Country | Period | Participants | Mortality | Complication rate | Complications | Effective application | Patients indicated | Unindicated but applied | Treatment | Timings |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Schroll R et al. A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg. 2015; 79(1):10–14 | Retrospective analysis | 4 | US | 01/2010–12/2013 | 197 | 3% (6/197) | 32.4% | Nerve palsy: 6.1% |
88.8% | n/a | n/a | n/a | Total tourniquet time: 48 minutes (mean) |
| 2. Inaba K et al. Tourniquet use for civilian extremity trauma. J Trauma Acute Care Surg. 2015; 79(2):232–237 | Retrospective review | 4 | US | 01/2007–06/2014 | 87 | n/a | 8% (Excluding 15 amputations) | Compartment syndrome: 2.3% |
n/a | n/a | 78.2% had an operation remainder local wound management | Duration of application mean: 103.2 mins (5–606 minutes) Pre-hospital transportation time: 35 minutes (9–90) | |
| 3. Scerbo et al. Safety and appropriateness of tourniquets in 105 civilians. Prehosp Emerg Care. 2016; 20(6):712–22 | Retrospective cohort study | 4 | US | 10/2008–05/2013 | 105 | 14% | 19% of indicated patients. 18% of total population (excluding amputation: 30 patients/29%) | Compartment syndrome: 1.9% |
96.2% | 94 (90%) | 11 (10%) | 71% underwent operative procedure(s) | Scene arrival–hospital time: 21 minutes average |
| 4. Kue RC et al. Tourniquet use in a civilian emergency medical services setting: a descriptive analysis of the Boston EMS experience. Prehosp Emerg Care. 2015; 19(3):399–404 | Retrospective review | 4 | US | 01/2005–12/2012 | 98 | 10.5% | 2.1% (excluding four amputations) | Numbness: 1.1% |
91.6% | 54.6% removed in ED 30 patients required surgery | n/a | 30/95 (31.6%) requires operative procedure | Mean pre-hospital placement time: 19.9 minutes (2–38–minute range) |
| 5. Zietlow et al. Prehospital use of hemostatic bandages and tourniquets: translation from military experience to implementation in civilian trauma care. J Spec Oper Med. 2015;15(2):48–53 | Retrospective review | 4 | US | 06/2009–01/2014 | 73 | n/a | n/a | n/a | 98.7% | n/a | n/a | n/a | Median injury to intervention time: 8 (2–95) minutes |
| 6. Ode G et al. Emergency tourniquets for civilians: Can military lessons in extremity hemorrhage be translated? J Trauma Acute Care Surg. 2015; 79(4):586–91 | Retrospective review | 4 | US | 09/2012–11/2013 | 56 | 7.1% | n/a | No complications due to tourniquet use. Other complications not listed. | n/a | 27 | 5 | 76.4% of tourniquet patients required emergent surgery for extremity haemorrhage vs 26.7% of non-tourniquet patients. Overall 53.1% of patients received some surgical intervention. | Mean duration of tourniquet use: 72 (16–241) minutes |
This process from literature search to study selection was completed by a second researcher (CP) to confirm accuracy and completeness. No further studies were added and agreement on the final lists was reached. Figure 1 shows the search process.
Data extraction
Data were extracted and formatted into tables. This included any data on the following:
Data analysis
A quality assessment was performed using the Oxford 2011 Levels of Evidence (Oxford Centre for Evidence-Based Medicine (OCEBM), 2011). The heterogeneity of the studies was also assessed. Because there were no randomised controlled trials and heterogeneity in the studies' methods and outcomes, a descriptive analysis was performed.
Quality analysis
The studies were analysed against the Oxford 2011 Levels of Evidence (OCEBM, 2011). Because of the lack of randomisation and the case control and cohort series nature of the studies' design, all studies were deemed to provide level 4 evidence.
The patients included in the studies were all in civilian settings and had similar characteristics in terms of age, sex, severity of injury and injury type. Table 2 outlines the patient characteristics for each study.
| Study 1 | Study 2 | Study 3 | Study 4 | Study 5 | Study 6 | |
|---|---|---|---|---|---|---|
| Age | 39.3 (mean) | 35.3 (mean) | 34 (mean) | 38.9 (mean) | 42 | |
| Male | 85.8% | 90.8% | 88% | 83.7% | 82% | |
| ISS | 11.3 (mean) | 6 (median) | 9 (median) | n/a | n/a | |
| MOI | Blunt: 36% |
Blunt: 33.33% |
Blunt: 49.5% |
Blunt: 9.2% |
Blunt: 37% |
Gunshot: 16.7% |
The tourniquets were applied predominantly by prehospital emergency medical personnel. However, in studies 4 and 5, tourniquets applied by what can be assumed to be non-medical bystanders were also included. Levels of training may vary because of variation in prehospital emergency roles and grades and state requirements for training. The Combat Application Tourniquet (CAT) was the most frequently used tourniquet in the studies.
Study 1 does not provide information on the tourniquet brand but does state it was ‘commercial’. Studies 1, 2, 3 and 5 all referred to ‘improvised’ tourniquets, which can be any device used to provide the effect of a tourniquet. Study 2 also included pneumatic tourniquets, which have a manual or automatic air pump to vary the tension applied.
Indication
Only two studies sought to ascertain the percentage of patients who had been indicated for tourniquet application as per local guidelines. The remaining studies appeared to assume application was because of the indication.
In study 3, 100% of patients had tourniquets applied, of whom 90% were indicated. The remaining 10% had wounds that did not meet application guidelines and could have been managed with alternative measures.
Study 6 has the lowest indication rate. However, this was a comparative study unlike the others included in this review.
Of the attempted tourniquets, 79% were indicated for use and 88% of indicated patients received a tourniquet, with one listed fatality resulting from failure to apply.
With the remaining studies, it is not possible to ascertain if all patients met indication requirements for tourniquet use as this was not assessed.
Application duration
Only three studies collected data on mean tourniquet application duration. This ranged from 48 minutes (±47.5 SD) (study 1) to 103.2 minutes (±11.6 SD) (study 2). Study 2 noted a mean prehospital transportation time of 35 minutes (range 9–90 minutes), which may indicate why the mean application duration was highest. Study 5 also recorded data on transportation time with a median of 9 minutes (range 1–74 minutes).
Effective application
Effective tourniquet application was high in the studies in the range of 88.8–98.7% (Figure 2).
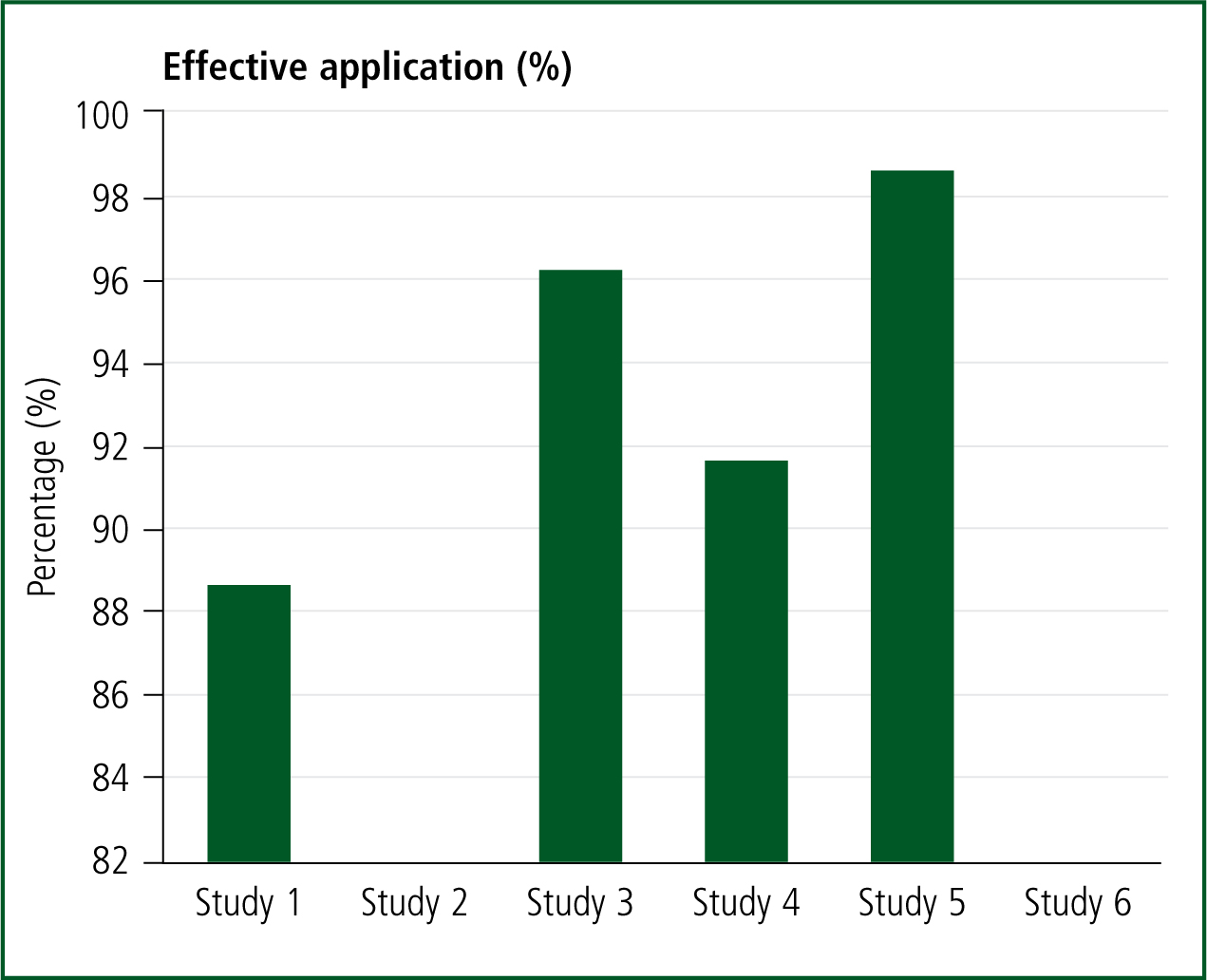
Study 3: Nine patients in total had additional tourniquets placed while in the emergency department (ED). Of these, four were because prehospital tourniquets had failed and the remainder were because an improvised tourniquet was replaced or for reasons that cannot be ascertained from the papers.
Study 4: Unsuccessful applications failed to stop arterial blood flow. Only one of the unsuccessful application patients appears to have received a second tourniquet, which successfully managed the haemorrhage. It is unclear what further interventions the other patients received.
Study 5: Seventy-seven tourniquets were applied to 73 patients. The failed application required another tourniquet to stem blood flow. The remaining patients required multiple tourniquets on different limbs. The study notes that all three of the improvised tourniquets were unsuccessful. However, these were not included in the application success calculations.
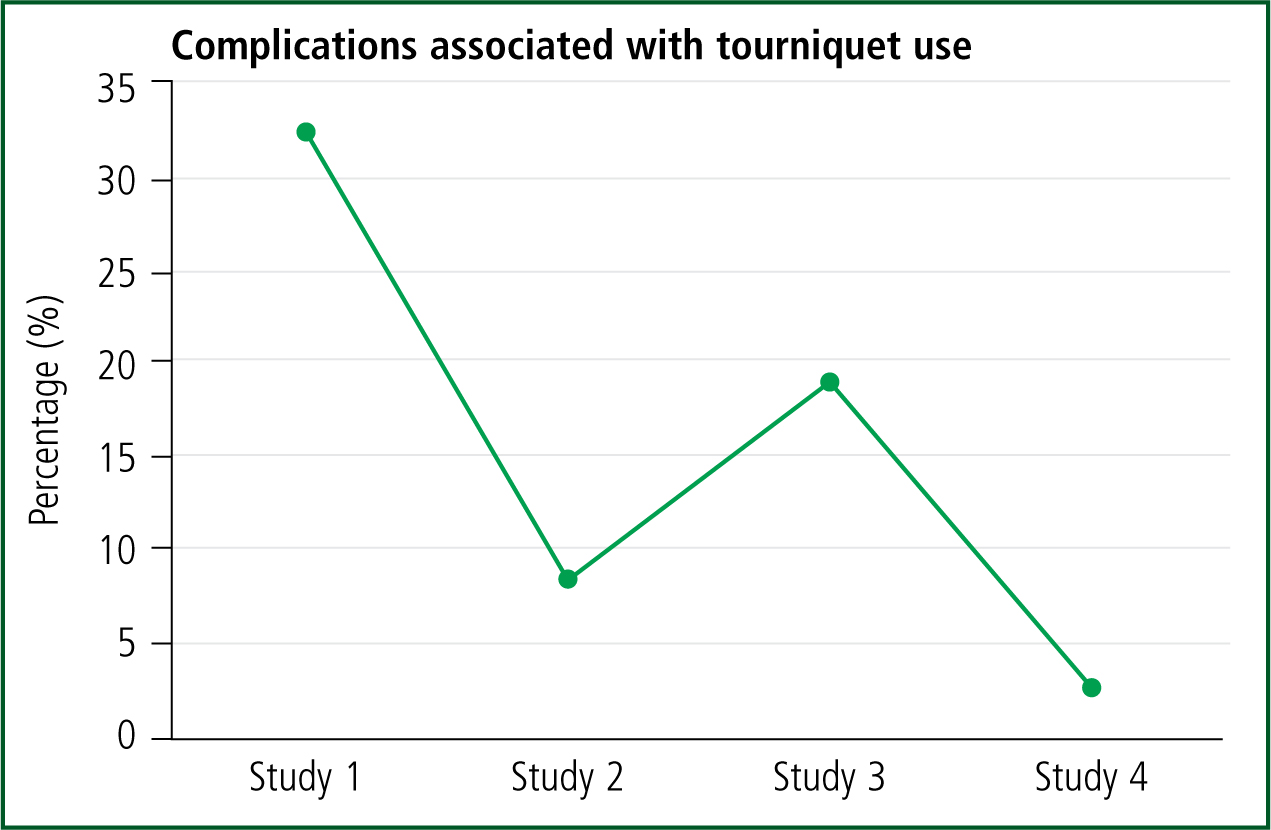
Complications associated with tourniquet use
Complication rates were in the 2.1–32.4% range. Study 1 had the highest complication rate at 32.4% and was the only study to include amputation in the complication rate calculation. Although amputations were completed in studies 2, 3 and 4, these were not included as complications, which may explain their lower complication rate.
Study 1 found that the average tourniquet time was lower in patients with ischaemia/reperfusion injuries (38.2±8.7 minutes vs. no ischaemia/reperfusion injury at 48.4±3.6 minutes, P<0.0001) and compartment syndrome (35.5±4.8 vs. no compartment syndrome at 49.2±3.8, P<0.0001), which would support the conclusion that the complications did not result from tourniquet use.
Study 2 suggested that no other complications can be attributed to tourniquet application. Study 3 noted one case of compartment syndrome that may be attributable to tourniquet application, but all other complications were not associated with the device's use. Study 4 had a low complication rate of 2.1% with only two complications recorded. Both were reported to have the potential to be caused by tourniquet use. The first was an intimal wall tear. The second was a persistent forearm numbness.
Table 3 shows the complications reported in the studies. The most common is amputation, which appears in all studies, closely followed by compartment syndrome, which appears in three of the studies. Figure 3 shows complication rates as a percentage of study populations.
| Study 1 | Study 2 | Study 3 | Study 4 | Study 5 | Study 6 |
|---|---|---|---|---|---|
| Amputation: 36% | Amputation: 17% | Amputation: 29% | Amputation: 4% | N/A | N/A |
| Compartment syndrome: 17% | Compartment syndrome: 2.3% | Compartment syndrome: 2.1% | Intimal wall tear: 1% | ||
| Secondary infection: 17% | Acute renal failure: 2.3% | Nerve palsy: 5.3% | Nerve palsy: 1% | ||
| Nerve palsy: 12% | Bleeding: 1.1% | Acute renal failure: 3.2% | |||
| Ischaemia/reperfusion injury: 7% | Coagulopathy: 2.3% | Venous thromboembolism: 8.5% | |||
| Adult respiratory distress syndrome: 1.1% | |||||
| Hepatic failure: 1.1% | |||||
| Shock: 1.1% | |||||
| Wound infection: 2.3% |
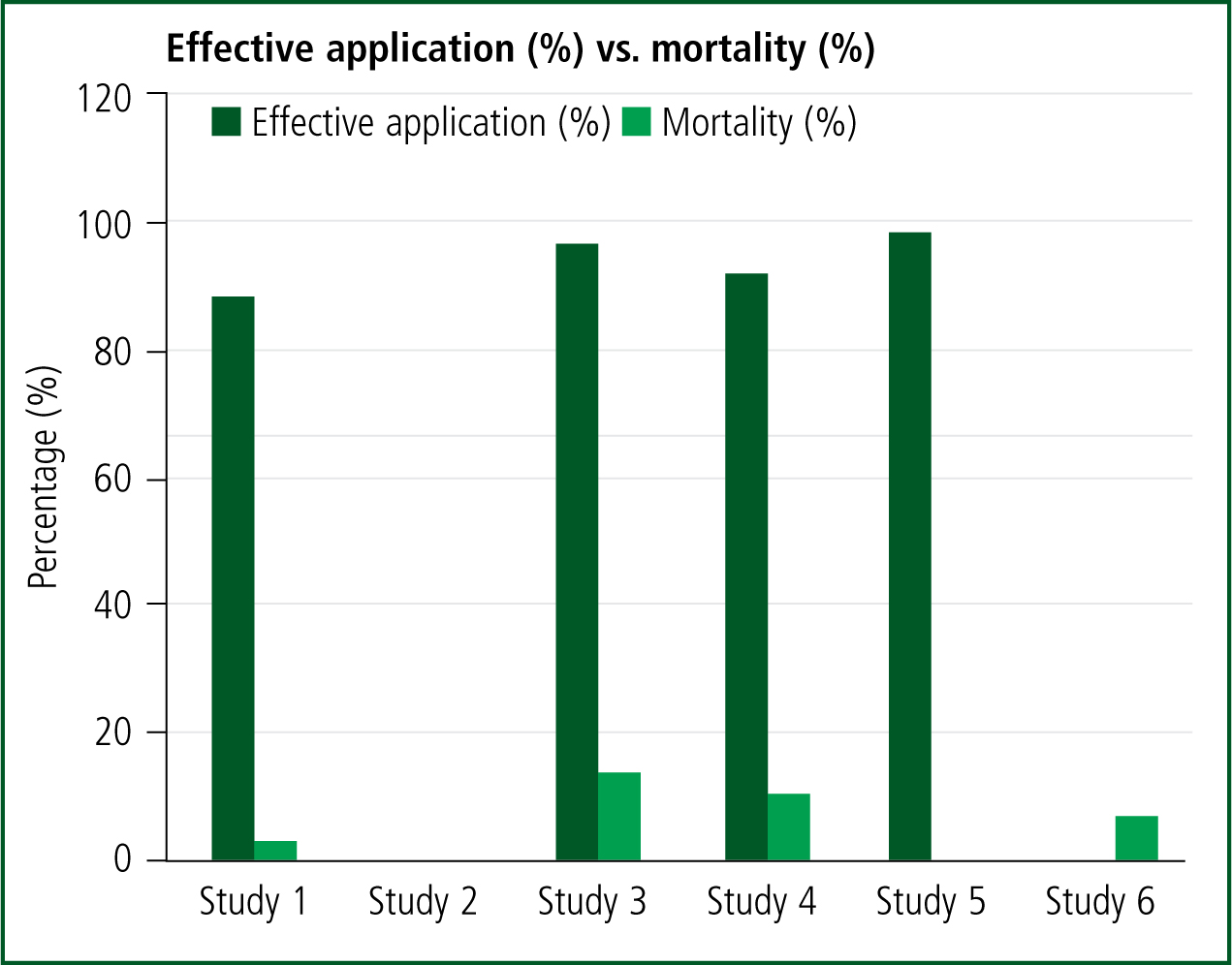
Mortality
Mortality rates across the included studies were in the 3–14% range (Figure 4). When comparing mortality rate and effective application, there does not appear to be a correlation between a lower rate of effective application and a higher mortality rate. Study 3 has the second highest successful application rate and the highest mortality rate. The lowest mortality rate is seen in study 1. However, this saw the lowest successful application rate at 88%.
Discussion
Indication
It is not clear from the data whether all patients were indicated for tourniquet application with only study 3 (Scerbo et al, 2016) assessing whether the patients' injuries warranted use (90% of applications were indicated).
Other studies noted outcomes that may provide some indication as to whether a tourniquet was appropriate. Of the participants in study 2 (Inaba et al, 2015), 78.2% required operative procedures, the remaining requiring local wound management. Similar results can be seen in studies 3 and 6 where 71% and 76.4% required surgery (Ode et al, 2015; Scerbo et al, 2016). Study 4 had the lowest surgical intervention rate with only 31.6% of patients requiring surgery. However, it is also noted that 54.6% of tourniquets were removed in the ED (Kue et al, 2015). This may provide some explanation for the low surgical intervention rate. However, this is comparable to study 3 where 48% of indicated tourniquets were removed in the ED, yet a higher surgical intervention rate was seen.
It could be argued, with tourniquets being a last resort tool for the use in catastrophic haemorrhage, that it may seem unorthodox for such a large number of them to be removed in the ED in comparison to during surgery. There may be some expectation for catastrophic wounds to require operative procedures, which may suggest tourniquet application was either not indicated or not the most appropriate haemorrhage management tool, a conclusion also drawn by study 4 (Kue et al, 2015). Despite this, such management may not have been possible in the prehospital setting so a tourniquet may have been the most appropriate available tool. Removal in the ED may also be a testament to modern trauma systems and such removal in a trauma centre may not be due to inappropriate application but simply that the appropriate physicians are available to immediately manage the needs of the patient.
Although inferences on tourniquet appropriateness based on subsequent treatment are broad and largely unsubstantiated, this does highlight the potential need for further research on the number of patients who are indicated, as some wounds may be better managed with alternative, less invasive methods. All bar one of the research studies seem to largely accept that application was indicated. However, this may be crucial when considering a risk-benefit analysis of tourniquet use, when alternative methods may have achieved haemostasis. Military research has concluded there are a variety of non-indicated applications.
Kragh et al (2011) reported a 2.5% non-indicated use rate, with a nerve palsy rate of less 2% and a 0.4% amputation rate caused by tourniquet use. Lakstein et al (2003) had a high non-indicated use rate of 47%, yet had a 0% complication rate, similar to Beekley et al (2008), who reported a non-indicated use rate of 18% with no complications found. Non-indicated use rates vary greatly across the research.
However, the theme, despite potentially inappropriate use, is a low to zero complication rate. This may suggest there is little detriment from applying tourniquets to patients not indicated. Despite this, the current step-wise approach within UK guidelines (JRCALC, 2016; NICE, 2018) may help to avoid inappropriate application.
The studies reviewed here provide no data on alternative haemorrhage control methods attempted to justify the application of a tourniquet.
Effective application
The effectiveness of prehospital application is high with some degree of failure expected. The lower results may be because of a higher use of improvised tourniquets in some of the research; however, there is evidence supporting their success (Beekley et al, 2008; Schroll et al, 2015).
Limited data are provided on the measures taken to correct the failures. Some studies note that further tourniquets were applied, and haemorrhage was then stopped. However, in some cases, this was not done until the patient was in the ED (Kue et al, 2015; Zietlow et al, 2015; Scerbo et al, 2016). The UK guidelines (JRCALC, 2016; NICE, 2018) recommend the use of further tourniquets when one fails to stem the flow of blood. Bandaging and haemostatic gauze may be combined to improve performance.
The effective application results are concurrent with the military research, with Kragh et al (2011) noting an effective application rate of 79% for the CAT device and Lakstein et al (2003) reporting a 78% effectiveness rate. Because data are limited, it is not possible to say whether these measures were attempted in the included studies and may have improved success rates. The high success rate does indicate that prehospital practitioners are proficient in tourniquet application.
As the included studies are all US-based, they are not easily generalised to the UK as guidelines and training for paramedics differ. However, the fundamentals of haemorrhage management remain the same.
Application duration
There appears to be great variance in application duration with little information on the reasons for these differences. Transportation time may provide some explanation as this may vary, depending on the geography of the study location. Study 2 had a transport time range of 9–90 minutes, which was slightly higher than the range for study 5 (1–74), which may suggest why study 2 had longer application durations (Inaba et al, 2015; Zietlow et al, 2015).
It is not possible to conclude whether longer application durations increased instances of complications; these would be assumed to be caused by higher rates of limb ischaemia. Research by Kragh et al (2008), however, looked at this area and concluded that duration of application does not affect morbidity.
In the UK, the trauma network is designed to ensure rapid transportation of patients to a major trauma centre via land or air. Studies have highlighted that tourniquets can be applied in elective surgery for 1–3 hours with few or no complications (Klenerman, 1980; Kam et al, 2001; Blaisdell, 2002). Within the UK, patients should be received at a major trauma centre well within that time frame, suggesting that application duration will pose little morbidity risk to patients.
Complications
From the studies that examined complications, no definitive link between the tourniquet and any specific complication can be made. Study 2 suggested that the tourniquet may have contributed to compartment syndrome in one patient; however, complete arterial dissection with distal ischaemia was visible before the tourniquet was applied, so injuries may have caused this (Inaba et al, 2015).
Study 3 found similar results to study 2, with the suggestion that the tourniquet may have contributed to one of the cases of compartment syndrome. However, this was believed to be likely caused by the cardiac arrest from exsanguination and delay in transfer and restoration of vascular flow to the limb rather than the tourniquet. All other complications were not attributed to tourniquet use (Inaba et al, 2015; Scerbo et al, 2016).
Study 4, like the other studies, suggests a difficulty in discerning the cause of complications (Kue et al, 2015). The comparatively low complication rate in study 4 may be explained by the high removal rate of tourniquets in the ED (54.6%) and low surgical intervention rate (31.6%). These figures suggest the patients had less severe injuries, so were less likely to experience complications.
What is apparent from the research is that no deaths resulted from complications. Under the assumption that all patients were indicated for tourniquet use so were experiencing catastrophic haemorrhage, without the use of the tourniquet, death would have been highly likely. Even if the complications reported in the included studies were all attributable to the use of the tourniquet, the risk-benefit debate sways in favour of use. Figure 4 shows effective tourniquet application as a percentage of the study population alongside mortality rates.
Those who were not indicated, however, may have been exposed to unnecessary risk, although this appears minimal. This conclusion supports findings from military research, which reports the benefit of tourniquets in reducing mortality, with few or no complications (Kragh et al, 2008; 2009; Tien et al, 2008; Ode et al, 2015).
Mortality
Within the included studies, it is difficult to compare mortality results as patient populations may vary in terms of injury patterns and severity; these data are not available from all of the studies. The studies that did record mortality report similar findings to the military research, with overall mortality being low.
Perhaps one of the more reliable military studies, because of its scale, is that by Kragh et al (2009), who found a strong association between tourniquet use and survival, with survival being 89% with the use of a tourniquet vs. 0% without—the pertinent factor in this being ‘time of application’. Early application dramatically improved outcomes with prehospital application survival being 89% vs. hospital use of 78%. Study 6 (Ode et al, 2015) saw similar results, with a trend towards worsening outcomes, with higher instances of shock and blood product requirements in patients who did not receive a prehospital tourniquet. Study 4 also noted delayed application but no comparisons were available on the outcomes of these patients (Kue et al, 2015).
The study by Kragh et al (2009) played a large part in changing global attitudes towards tourniquet use. One of its main limitations, however, was its focus on the combat setting. This may reduce its generalisability to the civilian setting because of the type of injuries and hospital facilities. Despite this, the indication of catastrophic haemorrhage remains the same. It can therefore be assumed that some of the indicated patients included in the studies in this review may have died from exsanguination if the tourniquet had not been applied.
Dorlac et al's (2005) research highlights the need for tourniquet use in civilian settings, suggesting that, although deaths from extremity haemorrhage are low in number, 57% of the cases assessed were amenable to control methods such as tourniquet use. Therefore, allowing prehospital paramedics to apply a tourniquet early will prevent prehospital exsanguination and possibly improve overall outcomes. Further retrospective research comparing patient outcomes with prehospital application of tourniquets vs. delayed application, such as in the ED, may be advisable to confirm this. However, evidence on such comparisons can be largely assumed from current research.
Limitations
The limitations of this review come largely from the studies included. The studies have no element of randomisation, which increases the chances of confounding bias and variables affecting the results. Randomisation, however, would be difficult when assessing tourniquet use and such a study would arguably breach ethics.
Likely areas of bias include the different tourniquets used within the studies. Although the most commonly used tourniquet was the CAT, alternative brands or designs such as windlass or improvised tourniquets were included, which may affect application success rate. None of the studies declared any bias in their tourniquet selection, and were largely based on what was used in their organisations.
There may have been other confounding injuries affecting mortality, which were not always discussed; these may affect overall mortality rates and death may not have been directly attributable to the tourniquet itself.
The exclusion criteria may have induced an element of risk by providing a narrow field for study selection, which could have excluded some studies that may have given a wider range or differing results in the examined areas, such as unpredicted complications. This review focuses on UK use of tourniquets. However, none of the studies included originate in the UK and differences in trauma services and training among prehospital medical practitioners reduce the generalisability of the results to UK settings.
Conclusion
It is clear from the included studies that prehospital medical practitioners can accurately apply tourniquets with a high level of success. This was reflected in the low mortality rates across the studies, in line with military research.
Application on non-indicated patients appears to be higher than in military research. However, complications of tourniquet use appear minimal, with no studies directly attributing any complications to the tourniquet device itself. As such, the reported cases of over-triage have caused little detriment to patients.
The step-wise haemorrhage management approach suggested by the UK guidelines (JRCALC, 2016; NICE, 2018) may reduce the number of non-indicated patients receiving tourniquet treatment. As all included studies originated from the US, UK-based research is recommended to evaluate the utility of prehospital tourniquet application by UK paramedics.
This review concludes from research that there is an apparent benefit to tourniquet use in the UK prehospital setting, so guidelines should continue to include the device in the management of non-compressible, catastrophic haemorrhage.

