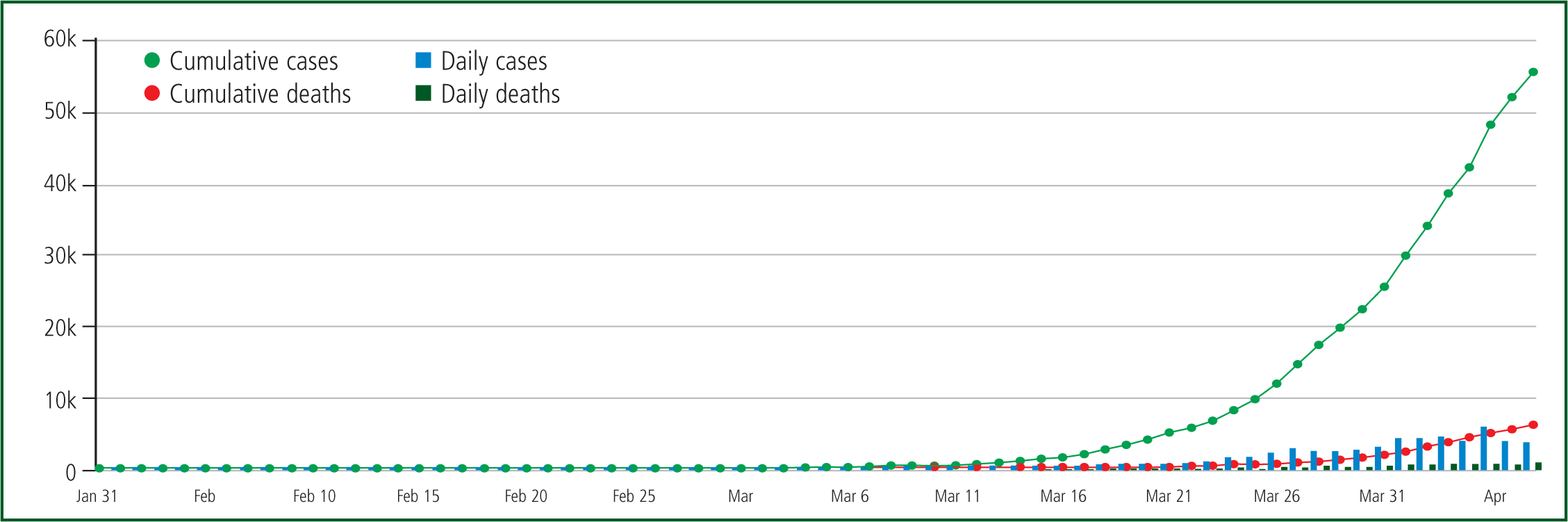
In late December 2019, a novel coronavirus was identified in the Chinese city of Wuhan, causing severe respiratory disease including pneumonia (Public Health England (PHE), 2020a). In January 2020, the World Health Organization (WHO) named this novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated disease as COVID-19 (Chen et al, 2020a; PHE, 2020a; WHO, 2020a). The first confirmed case of COVID-19 in the UK was recorded on 31 January 2020 (Razai et al, 2019) and the number of cases has continued to rise since then (Figure 1).
Similar to other coronaviruses that have infected humans, SARS-CoV-2 are enveloped, positive-sense, single-stranded RNA viruses that cause respiratory infections (Chan et al, 2020; Xu et al, 2020). As with most human coronavirus infections, most SARS-CoV-2 infections induce mild respiratory disease and symptoms (Chen et al, 2020b; Huang et al, 2020).
Epidemiology
As of 7 April 2020, there were more than 1 270 000 diagnosed cases of COVID-19 worldwide and over 68 000 confirmed fatalities (WHO, 2020b). At the same time, in the UK, there was a cumulative total of over 60 000 confirmed cases that resulted in 7097 COVID-19 related deaths (Department of Health and Social Care (DHSC) and PHE, 2020).
It is estimated that around 5–10% of patients admitted to hospital will become critically unwell and may require respiratory support in intensive care/therapy units (Guan et al, 2020; Remuzzi and Remuzzi, 2020).
Furthermore, the global estimated basic reproduction number (R0) was around 2–2.5 in early April (Kucharski et al, 2020; Li et al, 2020), which means a COVID-19 case could infect an average of 2–2.5 people in a population where everyone is susceptible and no one is specifically immune to it (Rothman et al, 2008).
COVID-19 has an estimated median incubation period of 4–6 days. Of those who develop symptoms, 97.5% will do so within 11.5 days (Chan et al, 2020; Chen et al, 2020a; Guan et al, 2020; Kucharski et al, 2020; Lauer et al, 2020; Li et al, 2020). Most patients will not be infectious until the onset of symptoms and their infectiousness depends on the severity of their symptoms and stage of their illness. However, due to the inter-individual variations in the length of incubation period, some infected individuals could be infectious before symptoms are developed and there are reported cases of asymptomatic transmission (Bai et al, 2020; Chan et al, 2020).
Infection prevention and control
Standard infection-control precautions (SIPCs) and transmission-based precautions (TBPs) must be used when managing patients with suspected or confirmed COVID-19. SICPs are the universal precautions that should be applied by paramedics routinely to minimise the risks related to the transmission of infections from all human body fluids, secretions and excretions. TBPs are additional infection-control precautions as SIPCs alone are inefficient in preventing the cross-transmission of COVID-19 (PHE, 2020b).
From the information available regarding SARS-CoV-2 viruses, it is believed that they have a similar route of transmission to SARS-CoV-1 and MERS-CoV, which is through respiratory droplets (>5 µm) produced when an infected person coughs or sneezes. These droplets can be inhaled into the lungs of people nearby or land on surfaces where the viruses can survive for a period of hours to days depending on the surface (van Doremalen et al, 2020), and then infect others in contact with those contaminated surfaces (PHE, 2020b). However, as SARS-CoV-2 can be isolated from the gastrointestinal tract, saliva and urine, these routes of potential transmission cannot be ruled out at this time (Guan et al, 2020; Wang et al, 2020).
In addition, some medical and care procedures known as aerosol-generating procedures (AGPs) could generate airborne particles contaminated by known infectious substances (aerosols) which are less than 5 µm in size (Health Protection Scotland and NHS National Services Scotland, 2019). These aerosols can remain suspended in the air, travel over a distance (which varies as a result of the ventilation in the environment), and may cause infection if they are inhaled. AGPs could be linked to healthcare workers' significantly increased risk of contracting SARS-CoV-1 during the previous SARS outbreak in 2003 (Gamage et al, 2005). Furthermore, recent evidence demonstrates that SARS-CoV-2 has similar properties to SARS-CoV-1, which is viable in aerosol form (≤5 μm) (van Doremalen et al, 2020). This would suggest SARS-CoV-2 could be airborne during AGPs.
A systematic review by Tran et al (2012) summarised the risks of SARS transmission in healthcare workers when carrying out different AGPs. This informed the New and Emerging Respiratory Virus Threats Advisory Group's (NERVTAG) decision on which procedures are included on the list of AGPs for the UK. Common AGPs conducted in prehospital care settings include some procedures related to cardiopulmonary resuscitation (CPR), such as advanced airway procedures, i.e. laryngoscopy, intubation, extubation and surgical airway; manual ventilation; suctioning; management of choking; and foreign body airway obstruction removal (PHE, 2020c).
It is worth noting that, even though nebulisation itself is an AGP, the evidence suggests that the aerosol from this does not contain viruses and minimal viable bacteria have been recovered (Li et al, 2017). During nebulisation, the aerosol is derived from a non-patient source (the fluid in the nebuliser chamber) and does not carry patient-derived viral particles. If a particle in the aerosol coalesces with a contaminated mucous membrane, it will cease to be airborne and therefore will not be part of an aerosol. Staff should observe hand hygiene when helping patients to remove nebulisers and oxygen masks.
A Canadian study recommended using a metered-dose inhaler of bronchodilators if available to minimise the theoretical risk of viral aerosolisation from nebulisation (Wax et al, 2020).
Personal protective equipment
With an increased level of COVID-19 in the community and the UK entering the sustained transmission phase of the pandemic in early April, PHE (2020c) has recommended two levels of personal protective equipment (PPE) for the ambulance sector (Figures 2 and 3).
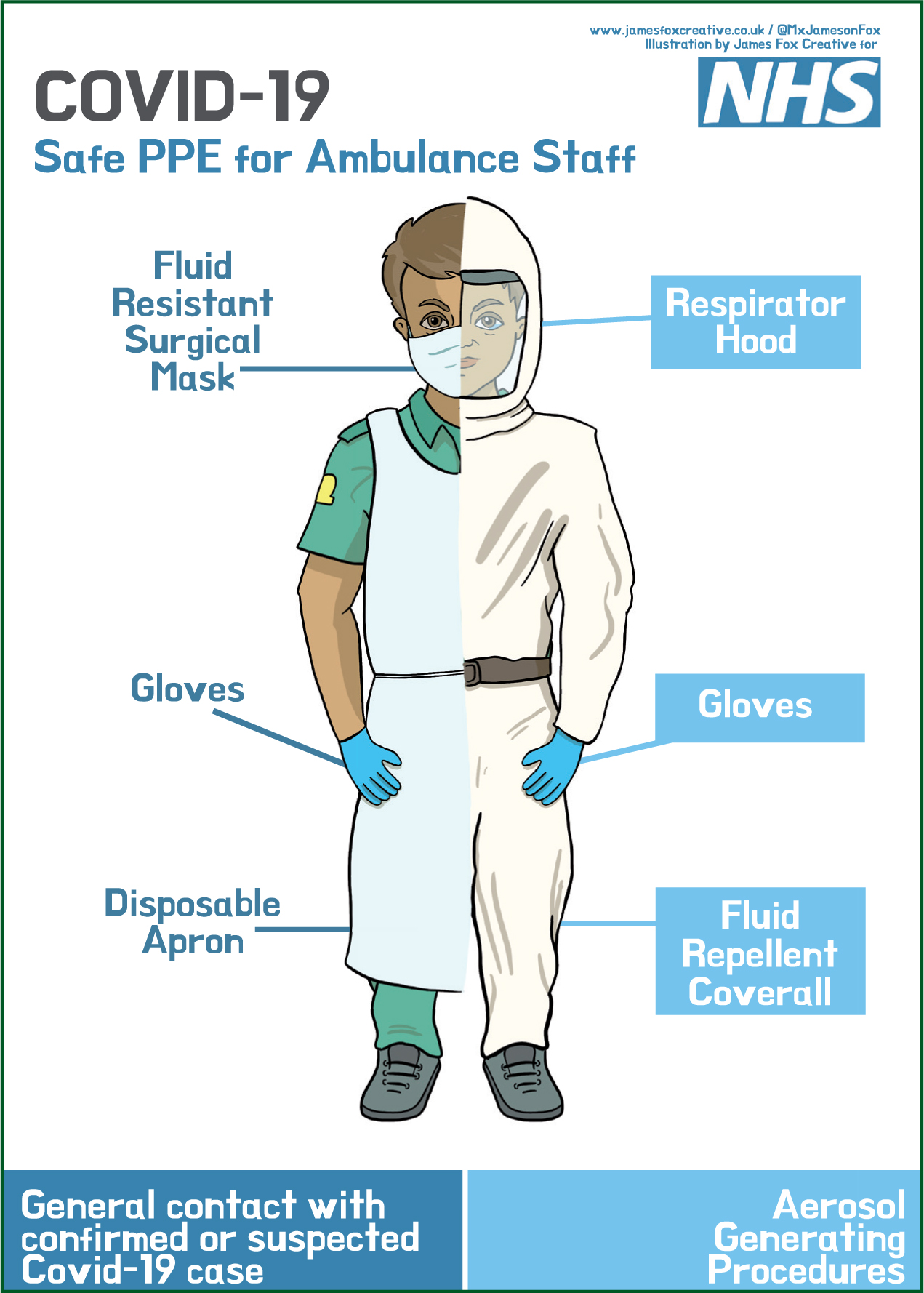
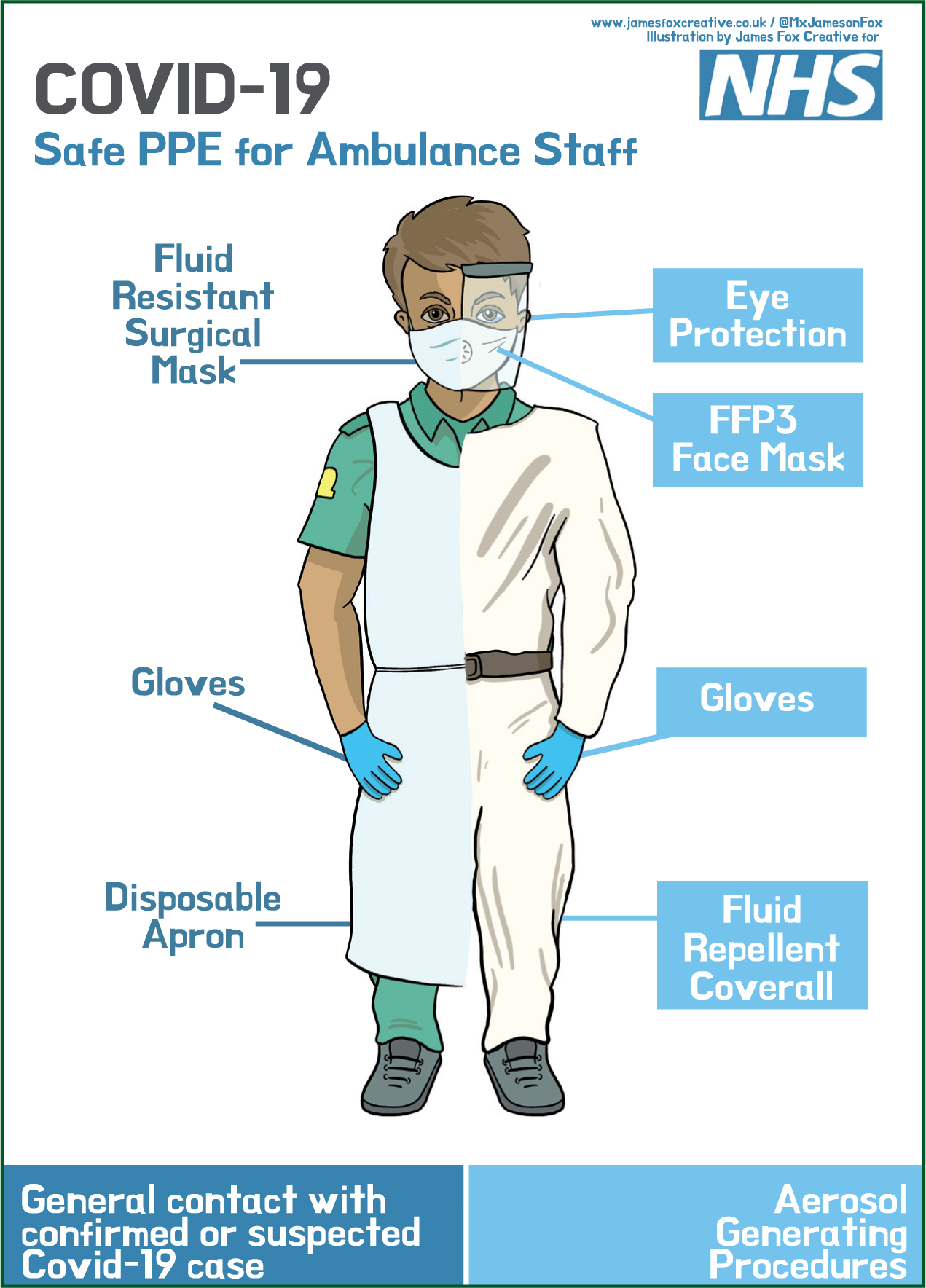
Level 2. All ambulance attendances regardless of patient symptoms
Level 3. Where aerosol-generating procedures are to be carried out
Clinical assessment of suspected/confirmed COVID-19 patients
Fever (>37.8°C), cough and myalgia or fatigue are the three most common symptoms present in patients who are infected with SARS-CoV-2 (Chan et al, 2020; Chen et al, 2020a; 2020b; Guan et al, 2020; Huang et al, 2020). Other, less common symptoms include sputum production, sore throat, headache, haemoptysis and diarrhoea (Chen et al, 2020b; Huang et al, 2020.
A current possible case definition of COVID-19 in the UK (as of 13 March 2020) (PHE, 2020d) is that:
In addition, paramedics are advised that COVID-19 should be considered in all cases of respiratory infection in prehospital emergency care settings (PHE, 2020e).
If patients meet the criteria below, they are to be classified as a possible or confirmed case:
Older people (aged over 60 years), men, patients with underlying long-term conditions (such as respiratory diseases, hypertension or diabetes) or comorbidities resulting in weaker immune functions have increased risks of developing severe illness from COVID-19 (Chan et al, 2020; Chen et al, 2020b; Guan et al, 2020).
Paramedics should use existing thresholds for vital signs and early warning scores (such as NEWS2 and paediatric observation priority scores (POPS)) to guide their management of patients with suspected or confirmed COVID-19, as abnormal vital signs such as increased respiratory rate, increased pulse rate and low oxygen saturation (<93%) on air have been linked to higher morbidity and mortality rates in reported cases (Chen et al, 2020a).
In addition, paramedics should be mindful that both adult and child deaths are increasing from conditions that are not related to COVID-19. This could be related to delayed presentation to healthcare because people fear and perceive a higher risk of contracting COVID-19 if they attend healthcare facilities.
Patients who present with a new continuous cough and/or fever (>37.8°C) and are well enough to remain in the community should be advised to stay at home and self-isolate. Their families should be advised to self-isolate for 14 days as per government advice (PHE, 2020e). Additional advice for those who are in self-isolation includes:
Telephone clinical assessment of suspected/confirmed COVID-19
At a time where much of the world is having to adapt to working remotely and using technology more, so are paramedics in their professional lives. Telephone triage, also known as remote clinical decision making (RCDM), has long been a well-recognised and is an increasingly used method of managing a growing demand on the ambulance and primary care services (Brady et al, 2018). Such services, along with advice and referral-based services (such as NHS 111, NHS 24, and NHS Direct), have seen rapid, significant increases in call volumes in response to COVID-19 (NHS England, 2020).
Guidance released by NHS England and NHS Improvement (2020) suggests that, in response to COVID-19, healthcare providers should implement remote consultations using video, telephone, email and text message services for all important routine activity as soon as possible. In addition, they should also ask clinical staff to work from home where possible and consider how they can provide telephone, digital or video-based consultations and advice for patients.
RCDM is fast becoming a recognised specialty in clinical practice and multiple professional career frameworks. This practice is normally underpinned by significant postregistration experience, bespoke training and, more recently, specific RCDM higher education (Brady et al, 2018). The impact of the significant increase in COVID-19 call volume when coupled with guidelines such as those mentioned earlier has meant that RCDM has become something upon which a range of clinicians have had little choice but to rely on entirely to carry out an increasing amount of their practice; with a lack of experience, training, and specialist education, and in home office environments away from traditional support mechanisms.
Staff already working in telephone triage will be adept in practising remotely, and pandemic flu algorithms in various clinical decision support software tools have been activated to support these practitioners more in assessment, as well as to adapt to changing demand management processes. Experienced RCDM staff are maintaining capacity and following public health guidance by using home-working packages with the use of digital phone systems and remote, computer-aided dispatch modules. Additional video-based platforms have been rapidly rolled out to augment this method of remote practice further and reduce some risk. Increased surge capacity can also be realised from these home working triage staff through the use of ad-hoc overtime in response to spikes in call demand and by freeing up space in clinical hub estates for newer staff who require more intensive support and guidance.
Many clinicians, however, prefer not to practise over the phone and, for some, it will not be possible at all. While there is evidence suggesting that telephone triage is generally safe in a normal cohort of general medical patients (Lake et al, 2017), the risks associated with clinical practice that is not carried out face to face are also well known and have been explored (Wheeler and Mahlmeister, 2016).
Telephone triage clinicians can assess and manage an estimated 3–4 patients per hour. In contrast, ambulance-based clinicians may see only one patient during this time. Many services are looking to redeploy clinical staff, recruit temporary staff, use military medical support and more readily use agency staff to provide remote assessment of patients to help with managing an overwhelming demand based on COVID-19.
To support clinicians new to working in this specialised area of clinical practice, the Royal College of General Practitioners (2020) has released guidance on conducting telephone consultations which, while helpful, provides little more than generic assessment and communication types adapted somewhat for remote practice. Greenhalgh et al (2020), however, provide a more robust case study approach to the remote management of patients with COVID-19 in an article entitled COVID-19: a Remote Assessment in Primary Care. This article presents the guiding principles to remote assessment by phone or video and provides a call structure consistent with other widely recognised tools. Clinicians who are new to remote practice should review this piece and other relevant articles.
While telephone triage was once an additional method of managing demand, it has, in response to COVID-19, become a method of managing the majority of demand and its use will rise as call volume increases. As a result, it must now be asked if the response to COVID-19 has created a context in which the face-to-face clinical consultation model has irrevocably been questioned and telephone/remote triage and assessment become the primary method of future clinical practice.
Medication for COVID-19
Supportive management is key, with no medicines as yet approved for the treatment of COVID-19. However, a number are undergoing clinical trials including within the UK (McCreary and Pogue, 2020).
It has been suggested that the use of angiotensin-converting enzymes inhibitors (ACEIs) and angiotensin-receptor blockers (ARBs) may increase the likelihood of contracting COVID-19 or its severity (Fang et al, 2020). This hypothesis is based on the theories that ACE2 facilitates the entry of SARS-CoV-2 and that ACEIs/ARBs have the potential to upregulate ACE2; this has been observed in animal studies but there is no consistent evidence from human data (Tignanelli et al, 2020).
There is no evidence available to support the routine discontinuation of ACEIs or ARBs. Paramedics should encourage patients to continue taking their prescribed medications unless specifically advised to stop by their medical team.
Paramedics with prescribing responsibilities should consider whether ACEIs or ARBs are being prescribed for current or long-term benefits. If they are being prescribed for current benefits (such as severe uncontrolled hypertension or heart failure), stopping these medications may lead to rapid deterioration. For patients who are taking ACEIs/ARBs for long-term benefits, precautionary principles should be applied, including withholding ACEIs/ARBs during acute infection, which could reduce the theoretical short-term risks during acute infection (Aronson and Ferner, 2020). It may be beneficial to ask the patient to contact the original prescriber or their GP for further information.
Paramedics are advised to continue with their existing prehospital emergency care drug interventions as indicated, as there is no current evidence to suggest that the appropriate use of intravenous fluids or glyceryl trinitrate is linked to worsening conditions in patients with COVID-19.
The media has reported that the use of non-steroidal anti-inflammatory drugs (NSAIDs) could worsen COVID-19 because of the theoretical risk of ibuprofen increasing the expression of ACE2, although this has been shown only in animal studies as noted (Qiao et al, 2015; Fang et al, 2020). Known NSAID effects, including reduced inflammation or fluid retention, may also contribute to the pneumonia seen in severe cases (PHE, 2020d). A recent systematic review found no published evidence for or against the use of NSAIDs in COVID-19 patients (PHE, 2020d).
Paramedics should take a cautionary approach by avoiding NSAIDs as the firstline option for managing symptoms of COVID-19, as recommended by UK guidance (Medicines and Healthcare products Regulatory Agency (MHRA) and the Commission on Human Medicines (CHM), 2020). However, if patients have been prescribed NSAIDs for existing conditions, they should continue to take these as directed by their health professional (MHRA and CHM, 2020; Royal Pharmaceutical Society, 2020).
While NSAIDs, ACEIs or ARBs should not be discontinued routinely because of COVID-19, this may be recommended in patients who become acutely unwell because of the risk of acute kidney injury (NHS, 2020).
Resuscitations in cases of suspected or confirmed COVID-19
The Resuscitation Council (UK) (RCUK) (2020a) has published resuscitation guidelines for health professionals managing patients who have or are suspected to have COVID-19. The current guidelines for advanced life support for COVID-19 patients are shown in Figure 4.
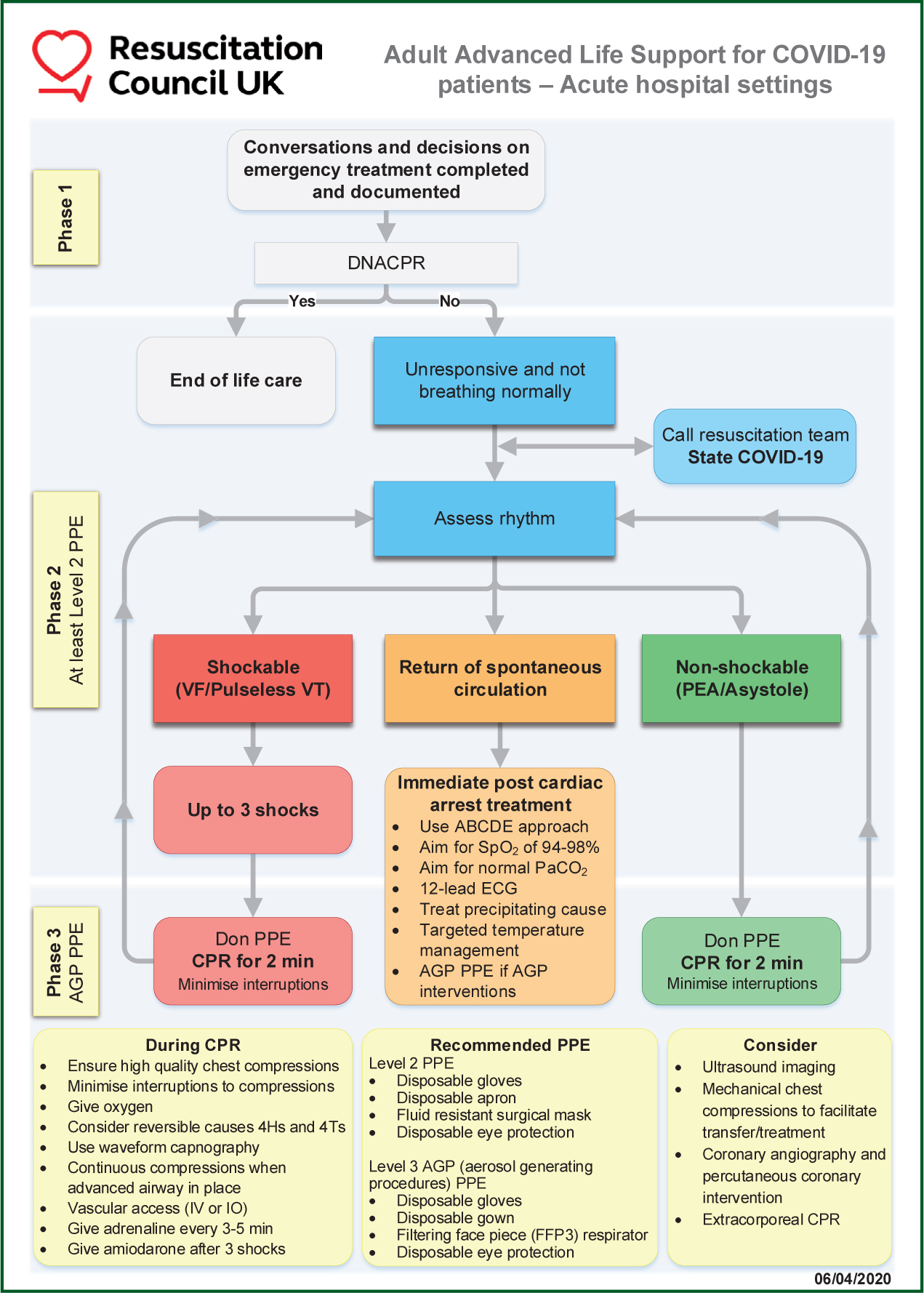
The RCUK guidelines are not specific to prehospital care; they can be adapted and are applicable within the remit of the healthcare provider (RCUK, 2020a). The RCUK (2020a) suggests that defibrillator pads can be applied during a cardiac arrest without PPE as ‘it may negate the need for chest compressions’; once the defibrillator has been attached and used, the rest of the team, where applicable, can put on level 3 PPE as per the advice given in the PPE section of the current article. The RCUK (2020a) emphasises the importance of following decision-making processes before the time of cardiac arrest and regarding whether to start CPR; however, this is not always possible in the prehospital environment.
Once the initial assessment has been made and, if the patient has a shockable rhythm, up to three shocks are recommended (RCUK, 2020b). This is specifically for the use of manual defibrillators. The RCUK recommends giving the first shock as usual, and reassessing the rhythm after this (RCUK, 2020b). If the patient remains in a shockable rhythm, a further shock should be applied. If there is a potential perfusing rhythm, the paramedic should check for a pulse. If the patient has moved to a non-shockable rhythm, chest compressions should be started with the appropriate PPE (RCUK, 2020b).
The RCUK's guidelines state that rhythm assessment and defibrillation are not AGPs; however, cardiopulmonary resuscitation is considered to be an AGP. Paramedics should also note that, for post-resuscitation care, an oxygen saturation level of 94–98% is recommended, because of acute lung injury and aspiration-induced lung injury caused by COVID-19 (RCUK, 2020b).
One of the biggest concerns lies around AGPs during resuscitation. The position of RCUK (2020b) is that chest compressions alone are an AGP and staff should wear level 3 PPE for AGPs, while the PHE (2020c) guidance explicitly states that chest compression and defibrillation are not AGPs. International guidelines (Couper et al, 2020) list CPR as an AGP but do not universally make clear which steps of the CPR process (e.g. defibrillation, chest compression, airway and ventilation) are AGPs.
With the continued escalation of COVID-19, guidelines and protocols will continue to be updated in response to ever-growing research, experience and clinical trials. During such uncertain times, it remains the clinician's responsibility to deliver the best care within their remit and to do so within personal safety parameters.
Stress management and wellbeing
As this article notes, the pandemic brings new clinical challenges and requires ambulance clinicians to work and think differently about their practice.
Combined with a potential increase in attendance to seriously unwell, dying and deceased patients, paramedics are likely to find themselves having to make critical clinical decisions that are ethically and morally challenging to their professional practice (Greenberg et al, 2020), and which may conflict with their personally held values and beliefs. This may result in ‘moral injury’ (Murray, 2019), where individuals experience thoughts relating to themselves and/or others that are negative and critical (such as thinking that they have failed a patient or not provided the care that they know a patient would have received under ‘normal’ circumstances). This may lead to feelings of intense guilt, shame and/or blame (Williamson et al, 2019). These thoughts may become injurious because they have a longer-term impact upon an individual's mental wellbeing in terms of the development of distress, anxiety, depression, post-traumatic stress and potentially suicidal ideation (Williamson et al, 2018).
The uncertainty and severity of the epidemiological progression of the disease will, naturally, result in paramedics feeling conflicted in their roles as health professionals, as well as in their roles in their personal lives such as son, daughter, husband or wife. The psychological impact of this can be profound. In particular, it will likely include heightened emotional and behavioural responses to potential pathogenic exposure including extreme fear and anxiety over the risk of infecting the self and others, and intense feelings relating to a perceived elevated risk of mortality.
Shift working, exhaustion and fatigue, limited time in which to rest and eat nutritious meals, along with the challenges of physical distancing and social isolation that may be impacting upon family life potentially make for a distressing and psychologically traumatic time.
Feeling scared and fearful at the risk of uncertainty is difficult to live with; people usually like some kind of order and normality in their lives, and this is being challenged. To feel this way, however, is a normal human response to a situation that is far from normal (WHO, 2020c).
While many people are likely to experience distress at some point (if not throughout the pandemic), some individuals may also experience a hopeful outlook with an increased sense of personal strength that enhances feelings of resilience (Tedeschi and Calhoun, 2004). As they appraise the impact of this viral disease in terms of their own beliefs and values, it brings with it existential considerations and thoughts that lead to a changed perception of life with new priorities and more meaningful personal relationships, potentially leading to enhanced psychological wellbeing (Joseph and Linley, 2008).
Connecting and talking with others can help to offload distressing and overwhelming thoughts, normalise feelings and, as research studies have highlighted, are key to the healing process. Feeling supported and cared for, and experiencing kindness and compassion, enhances wellbeing, promotes recovery and protects mental health (Mental Health Foundation, 2020).
As we move through the pandemic to the peak of contagion and in the days and months afterwards, it is human connectivity and the support of each other that will enable all to come through this time of adversity, and adapt to the new normality of life, work, and the better times to come.
Limitation and conclusion
While the information and advice within this article is up to date as of 7 April 2020, this is a rapidly changing field with the evidence base being added to daily. It is therefore important that paramedics keep up to date with the latest clinical guidance from their employers.

