In the UK, major trauma affects 20 000 people each year, with approximately 500–600 people sustaining injuries to the spinal cord (National Institute for Health and Care Excellence (NICE) (2016). This costs the NHS £0.3–0.4 billion annually (National Audit Office, 2010).
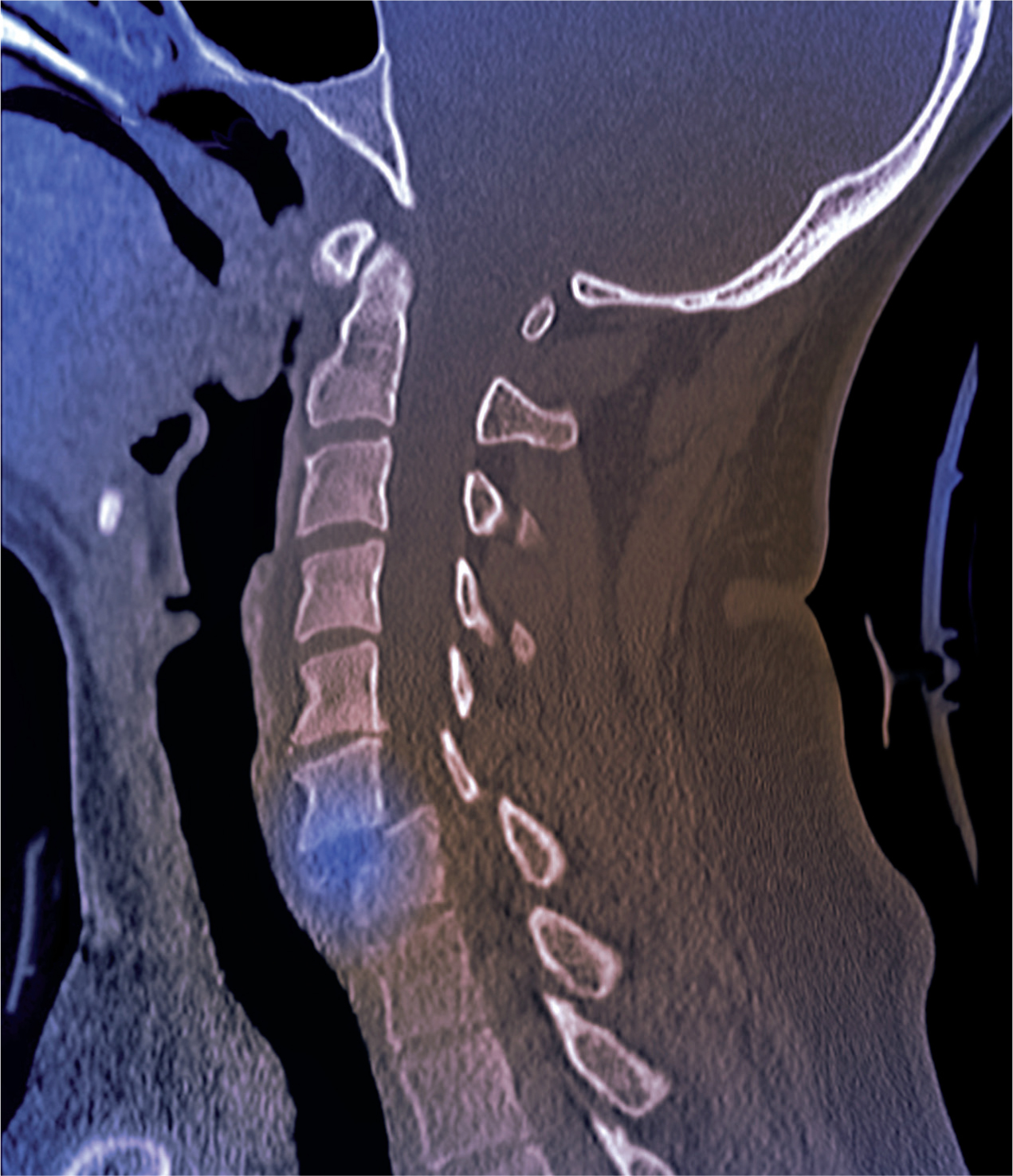
A spinal cord injury (SCI) is damage to the spinal cord; half of the fractures that cause SCI involve the cervical spine (Spinal Injuries Association, 2009) (Figure 1). SCIs generally affect young adults and commonly result from road traffic collisions, falls, sports and domestic violence (Casey, 2017). Mortality is highest during the first year after the injury and is correlated with injury site and severity (World Health Organization, 2013). Secondary conditions, such as respiratory dysfunction and pulmonary infections, as well as suicide, can result from SCI in the long term (Hagen et al, 2010).
Current UK ambulance guidelines follow an immobilisation algorithm (Figure 2). These stipulate that if immobilisation is indicated, the whole spine should be immobilised using an orthopaedic scoop stretcher, head restraints and a rigid cervical collar, and that this provides the best possible outcome (Brown et al, 2016). Emphasis on cervical immobilisation was established in the 1960s as it was estimated during this time that cervical spine injuries caused 40% of neurological deficits; collar placement was subsequently included in teaching objectives for paramedics and other ambulance staff (Poldolsky et al, 1983).
The use of cervical collars is however debated in the paramedic profession. Although they were originally considered harmless and used as a precautionary measure, an increasing amount of evidence suggests otherwise (Rogers, 2017), with arguments in the literature that collars cause more harm than good and should not be used (Sundstrøm et al, 2014). Therefore, it can be debated whether the practice of using them is consistent with the principles of patient safety and evidence-based practice as stipulated within the Health and Care Professions Council (HCPC) (2014) standards of proficiency for paramedics.
The current literature review will aim to comprehensively examine research surrounding the adverse effects of cervical collars, and the range of movement they enable, to gain a comprehensive understanding of their efficacy.
Methods
A literature review was chosen to source up-to-date research and knowledge, in order to identify areas for further investigation and, ultimately, to gain more knowledge regarding a topic that is of interest (Mooney, 2012).
EBSCHOhost was searched in June and July 2017 to obtain the literature (Table 1) and five key search terms were identified. Synonyms, variations in spelling, Boolean search terms and truncation symbols were used to identify relevant literature surrounding the topic (Table 2) (Aveyard, 2014).
| Academic Search Premier |
| Business Source Premier |
| CINAHL Plus with Full Text |
| Education Research Complete |
| Green FILE |
| Humanities International Complete |
| LISTA (Library, Information Science and Technology Abstracts) |
| Medline |
| PsycARTICLES |
| Psychology and Behavoural Sciences Collection |
| PsycINFO |
| Regional Business News |
| SPORTDiscus |
| Teacher Reference Center |
| 1 | a | Cervical spine | b | C Spine | ||||
| 2 | a | Immobili?ation | b | Immobilization or | c | Immobilsation | ||
| 3 | a | Cervical collars | b | Collars or | c | Collars | ||
| 4 | a | Spinal | b | Spine | ||||
| 5 | a | Prehospital | b | Paramedic | c | Ambulance | c | Emergency |
Search parameters included peer reviewed and full text. Inclusion criteria were studies based on adults aged 19+ years, prehospital settings for relevance to paramedic practice, written in English with key terms discussed in academic journals and abstracts of the articles. Exclusion criteria were: studies based on paediatric patients as paediatric literature around this subject is limited because of a low incidence (Domeier, 1999); non-traumatic incidences of SCI as outcomes vary (DeVivo, 2012); and interventions in which cervical collars are already being used. Evidence published before 1997 was not used in the present review.
Results
The searches yielded 1184 articles, of which 1164 were excluded for not meeting the inclusion criteria. The database search terms and results are shown in Table 3. The 20 remaining articles were scrutinised, and articles that were not primary research removed. A final seven articles were subjected for critical appraisal using the Critical Appraisal Skills Programme (CASP) (2018) tools, and Garrard's (2007) grid method was adapted (Table 4) to assess their validity, results and relevance to practice (Public Health Resource Unit, 2006).
| Database | Search | Results | Extracted | |
|---|---|---|---|---|
| 1 | EBSCOhost | 1 and 2 | 87 | 5 |
| 2 | 1 or 2 and 3 | 201 | 2 | |
| 3 | 2 and 3 | 479 | 3 | |
| 4 | 2a and 2b and 3b and 3c | 116 | 2 | |
| 5 | 4 and 2a and 2b | 198 | 3 | |
| 6 | 4 and 5 | 3 | ||
| 7 | 1a and 2b and c and 5 | 103 | 2 | |
| Total | 1184 | 20 | ||
| Research title, authors, date, country | Aims and objectives | Research focus | Research methods and ethical issues | Population and sample size | Strengths and weaknesses of methodology | Main findings | Themes |
|---|---|---|---|---|---|---|---|
|
Cervical immobilisation—are we achieving it?
|
Clear, focused question to investigate the immobilising effects of collars with and without head blocks | Immobilisation with and without head blocks |
|
|
|
|
Range of motion |
|
Changes in physical examination caused by use of spinal immobilization
|
Clear, focused question to determine whether spinal immobilization causes changes in physical examination findings over time | Doesimmobilisation cause physical changes? |
|
|
|
|
Adverse effects |
|
Assessing range of motion to evaluate the adverse effects of ill-fitting cervical collars
|
Clear, focused question to address how ill-fitting collars affect range of motion by measuring effectiveness of cervical orthoses in less than optimal settings | Analysing effect of ill-fitting cervical collars |
|
Twelve men aged 21-35 with no history of cervical injury |
|
A patient wearing a too small or too big collar could experience further cervical damage, highlighting the importance of applying a correctly fitting collar in a clinical setting | Range of motion |
|
Cervical collars are insufficient for immobilizing an unstable cervical spine injury
|
Clear, focused question to determine the extent to which orthoses immobilise in a cadaveric model with and without spinal instability | Analysing effect of cervical collars |
|
Five lightly embalmed cadavers with no history of cervical injury imitating unconscious patients |
|
|
Range of motion |
|
Value of a rigid collar in addition to head blocks: a proof in principle study
|
Clear, focused question to analyse the effects on the range of motion when a rigid collar is added to head blocks when a patient is strapped to a backboard | Analysing effect of cervical collars |
|
10 healthy subjects with different body types |
|
|
Range of motion |
|
Pressure ulcers, indentation marks and pain from cervical spine
immobilization with extrication collars and head blocks: an observational study
|
Occurrence and severity of pressure ulcers, indentation marks and pain from the extrication collar combined with head blocks. The influence of time, injury severity and patientcharacteristics on thedevelopment of pressure ulcers, indentation marks and pain were explored | Influence of time, injury severity and patientcharacteristics on adverse effects |
|
623 patients with suspected SCI were admitted. 57 had collars and boards removed quickly, 10 died within 24 hours, 51 refused to participate, 6 were excluded, 13 were transferred, 144 had collars removed before admission to the emergency department or care was prioritised over data collection, leaving 342 patients to be included |
|
|
|
|
The characteristics and pre-hospital management of blunt trauma patients with suspected spinal column injuries: a retrospective observational study
|
Clear, focused question to: determine the prehospital characteristics of patients; assess clinicians' choicesregarding spinal immobilisation; and identify possible adverse effects of spinal immobilisation | Characteristics of patients who areimmobilised and adverse effect |
|
1082 patients were included, with 96.3% having spinalimmobilisation based on prehospital criteria |
|
|
Adverse effects |
The final selected articles included three quantitative repeated measure studies, one quantitative retrospective study, two quantitative observational studies and one quantitative prospective study. Two themes were identified:
Adverse effects
Clinical decision making must incorporate ethical considerations to act in the patient's best interest and do no harm (Willis and Mehmet, 2015). Evidence suggests that cervical collars have adverse effects (Rogers, 2017). The first theme identified in the current literature review is that it is a clinician's responsibility to recognise the limiting effects of interventions (HCPC, 2014).
Despite the assumed beneficial effect of spinal immobilisation, evidence suggests that the practice is associated with dangerous adverse effects (Duncan, 2016). Using a retrospective study design over 5 years where spinal immobilisation was applied to 96.3% of 1082 patients, Oosterwold et al (2016) researched the incidence of possible adverse effects of spinal immobilisation in the prehospital setting. This time frame afforded a large sample of trauma patients which is therefore considered representative of the population (Ellis, 2016).
Although Oosterwold et al (2016) expected to see results comparable to those in Kwan et al's study (2005), where 55% of healthy volunteers complained of moderate-to-severe pain within 30 minutes of spinal immobilisation, they documented pain in 0.9% of patients. Possible explanations for this discrepancy were that on-scene times were less than 30 minutes (Oosterwold et al 2016), despite the mean total time from initial contact to hospital arrival being 49.13 minutes. However, the standard deviation was determined to be 16.25, so individual times could have been much longer or shorter than the mean, which lessens the validity of the study (Aveyard, 2014). Another explanation for the discrepancy is that adverse effects were not documented (Oosterwold et al, 2016). In addition, 75 (6.9%) patients showed signs of increased intracranial pressure, conceivably produced by venous compression in the neck causing brain swelling (Hunt et al, 2001). However, despite prehospital trauma life support (PHTLS) (National Association of Emergency Medical Technicians (NAEMT), 2018) guideline recommendations, the rigid cervical spine collar was not removed (Oosterwold et at. 2016). A lack of awareness and non-explicit documentation of removal could account for this, further decreasing the validity of the study (Oosterwold et al (2016). Oosterwold et al (2016) added that clearance needs to be a priority to minimise time in the collar in order to prevent adverse effects.
While Oosterwold et al (2016)'s research design studied the incidence of adverse effects, Ham et al's (2016) study outcome focused on pressure ulcers (PUs) and associated pain. Although collars protect the possibly injured spine, the risk of PU development and pain increased as a result of short-term pressure on the skin, as was identified by Ham et al's (2016) study.
PUs and pain were dependent variables, and independent variables, including Glasgow Coma Score (GCS), age and sex, were used to explore associations (Ham et al, 2016). Investigating the independent variables or exposure on the dependent variable or outcome provides a basis for discussion of what causes an effect (Ellis, 2016).
Ham et al (2016) used a sample of 342 patients following emergency department (ED) admission with a suspected SCI, although this was smaller than that in Oosterwold et al's (2016) study. However, a sizeable proportion of patients in the sample were excluded from Ham et al's (2016) study, possibly distorting the results and consequently decreasing the validity of the study (Aveyard, 2014).
PUs were present in 78.4% of patients after the cervical collar and head blocks had been removed. Grade 1 PUs (non-blanchable erythema of intact skin) were found in 75.4% of patients and 2.9% had developed grade 2 PUs (partial-thickness skin loss with exposed dermis). At least one severe indentation mark was observed in 28.1% of patients. PUs were categorised using the National Pressure Ulcer Advisory Panel (NPUAP) (2014) guidelines. Values were all within the 95% confidence levels, indicating that these results did not result from chance, strengthening the validity of the study (Aveyard, 2014).
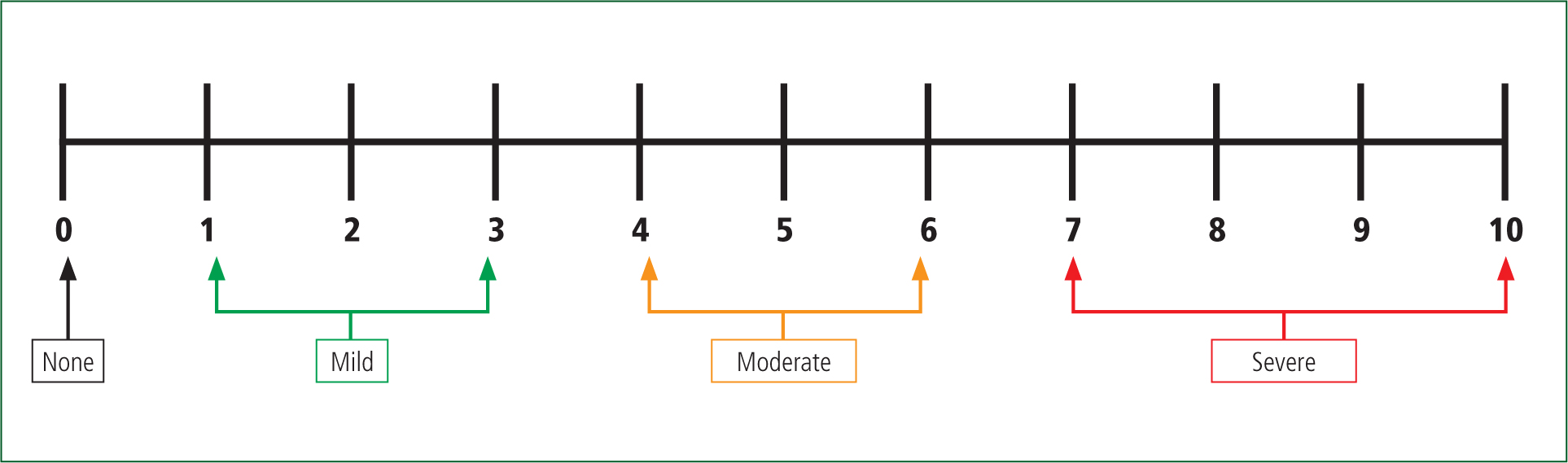
PUs cause pain and affect physical, social, psychological and financial aspects of living, depending on their severity (Gorecki, 2009). While grade 1 PUs are reversible, there is a risk they can become more severe (NPUAP et al, 2014), making prevention vital. To evaluate pain, Ham et al (2016) used the numerical rating scale (NRS) (Figure 2). The NRS can be used to document a subjective feeling of intensity of pain while measuring discomfort and grading the impact of pain on function (Breivik et al, 2009). Pain was experienced in 63.2% of patients, while 38.5% experienced severe pain.
It is assumed that pressure causing severe pain results in distress, necessitating movement to relieve pain, so high pain scores resulting from pressure potentially impede the main purpose of the cervical collar (Ham et al, 2016).
Protecting the spine from further injury must be a priority to minimise adverse outcomes and further complications (Ham et al, 2016). While prioritising clearance of the spine minimises the time in a cervical collar, safer alternatives to the cervical collar need to be found, taking into consideration various morphological aspects (Ham et al, 2016).
March et al (2002) used a single-blinded prospective study including 20 healthy volunteers to take account of the placebo effect, where healthy participants experience a variance in theoretical expectations (Booth et al, 2012). The study used convenience sampling—the least time-intensive and least expensive type of sampling—which lends itself to a small sample size. It typically underrepresents certain sociodemographic groups as participants are chosen based on accessibility (Bornstein et al, 2013) and so provides a false representation of the general population (Aveyard, 2014).
Subjects were fully immobilised for 60 minutes using a cervical collar, wooden backboard and straps. They subjectively rated their back pain every 5 minutes using the NRS pain scale (Figure 3). Subjects were rolled, had their vertebrae palpated to elicit midline tenderness, and were asked if they had any pain on palpation every 10 minutes (March et al, 2002).
While this research aimed to understand individual experience to establish a participant viewpoint, making it qualitative in nature (Williams, 2012), it also included the variable of time to answer the question, which involves the use of statistics to analyse data, making it quantitative as well (Booth et al, 2012). The outcome demonstrated a statistically significant increase (P=0.0001 over 60 minutes). However, analysis showed a significant statistical change in the first 30 minutes (P=0.0001) while the latter half showed no significant change (P=0–1294).
This suggests that pain is time-dependent and immobilised patients need immediate assessment on admission to the ED to prevent pain (March et al, 2002). The backboard was the presumed cause of iatrogenically induced midline vertebrae pain (March et al, 2002). Conner et al (2013) say that backboards should be used exclusively as an extrication device and not for conveying. Therefore, an orthopaedic scoop could have prevented the iatrogenically produced midline-point tenderness (March et al, 2002).
While this study found a significant increase in pain during the first 30 minutes and therefore identifies clearance as a priority, it also has limitations. Routine use of backboards during conveyance of patients with suspected SCI—an outdated practice—could distort the conclusions and relevance to practice, lessening the strength of the study. While protecting the spine is the priority, adverse effects can be detrimental to a patient's outcome (Ham et al, 2016).
Spending time in a collar was identified as a cause of pain (March et al, 2002; Ham et al, 2016; Oosterwold et al, 2016), and clearance needs to be a priority to minimise time spent in the collar. Pain was most prevalent in the initial 30 minutes in a cervical collar (March et al, 2002) and, while this study uses out-of-date techniques, it does carry an important consideration.
Vincent-Lambert and Mottershaw (2018) substantiate that lengthy on-scene times need to be addressed, and conclude that prolonged on-scene time could negatively affect patient outcome. Ultimately, practice needs to be challenged to minimise adverse outcomes becoming detrimental with an emphasis on finding safer alternatives (Ham et al, 2016). Clinicians need to recognise that full immobilisation may not be suited to a generic guideline to avoid adverse effects and not all patients with suspected SCI need to be fully immobilised (Theodore et al, 2013).
Range of movement
As discussed, spinal immobilisation comprises three elements (Brown et al, 2016):
Owing to the uncertainty of how much movement is permissible when an SCI is suspected, immobilisation should inhibit movement (Houghton and Driscoll, 1999). This raises the discussion of the range of movement when a cervical collar is in place.
Aiming to study the efficacy of collars by evaluating the effect of head blocks with and without collars and the effect of incorrectly sized collars, Houghton and Driscoll (1999) used 24 healthy subjects—a sample size comparable to that used in the adverse effect study by March et al (2017). However, using a small sample of healthy volunteers does not provide a true representation of the population, decreasing the validity of the study (Aveyard, 2014). Of the 24 participants recruited from a hospital, 15 were men, which is a representative sample of the general population as 81% of those with SCI are men (Casey, 2017).
Subjects were immobilised on a long spinal board in addition to the cervical collar, and asked to actively move their head as far as possible in flexion, extension, left and right lateral flexion, and both left and right rotation (Houghton and Driscoll, 1999). A repeated-measures design was used to assess the range of movement (ROM) when in a collar alone and with the addition of head blocks; this was repeated with ill-fitting collars in the same order each time (Houghton and Driscoll, 1999), thus maintaining consistency.
Two subjects were unable to have larger ill-fitting collars applied as they were already at the maximum size. In these cases, values obtained were reproduced using the technique known as last value carried forward, filling in data based on existing data. Using this technique can lead to bias; however, Houghton and Driscoll (1999) felt that if these results were omitted, the findings would be less significant and it was therefore considered acceptable.
Results indicated that collars alone restrict movement by 30–40%; head blocks increase restriction by 20–30%; and collars alone restrict movement but do not achieve total immobilisation (Houghton and Driscoll, 1999). The study's age means that some practices are outdated as the long board is no longer used in practice and has been replaced by the orthopaedic stretcher (Brown et al, 2016). However, the hard collars used in this study are still being used, which demonstrates its relevance to current practice.
As immobilisation is essential in extrication and prehospital transport, poorly fitting cervical collars can be detrimental, allowing movement and reducing immobilisation (Houghton and Driscoll, 1999). Therefore, Houghton and Driscoll (1999) recommended that the use of collars be supported with head blocks to increase immobilisation—a statement supported by Theodore et al (2013), who state that a combination of a cervical collar and head blocks is effective for spinal immobilisation.
Holla (2012) carried out a similar study to Houghton and Driscoll (1999), measuring the ROM when a cervical collar was used with head blocks over four planes to carry out a proof-of-principle study observing the active ROM. Using 10 healthy volunteers—a smaller sample size than Houghton and Driscoll (1999)—Holla (2012) determined that increasing the number of participants in this study would not affect the outcome as the best cervical immobiliser can be identified through the ROM it allows. However, the outcome of this study cannot be transferred generally across the population as no obese or short participants were used, which lessens the study's validity (Aveyard, 2014).
Statistically, the difference in ROM with the collar was significantly lower than with no collar (P<0.005). There was also significantly less ROM when head blocks were used compared with the rigid collar (P=0.005), but no significant decrease when the rigid collar and head blocks were combined (P>0.05) (Holla, 2012).
Research by Poldolsky (1983) suggested using sand bags with tape, as head blocks were more effective than any collar. Holla (2012), using modern accurate testing, supports Poldolsky's (1983) study and quashes the assumption that using a combination of head blocks and cervical collars results in the best immobilisation.
Furthermore, while the aim of a cervical collar is to restrict movement, Holla (2012) found that it significantly reduced the range of mouth opening, thus compromising the airway, making the use of adjuncts and maintaining a patent airway difficult (Kwan et al, 2001). PHTLS guidance states that continuous oxygenation in trauma patients is paramount, putting emphasis on the importance of keeping the airway patent while maintaining a neutral cervical spine, so a clinician must exercise vigilance under these conditions (NAEMT, 2018).
Holla (2012) concluded that rigid cervical collars did not provide any significant additional immobilisation to head blocks, whereas using a collar could create adverse effects, as discussed. Therefore, combining hard collars and head blocks should be reconsidered.
While Houghton and Driscoll (1999), Bell et al (2009) and Holla (2012) used healthy participants, Horodyski et al (2011) used cadaver models to determine the extent to which cervical collars immobilise the spine with and without stability, using no collar as the control. Cadavers limit the study by negating the natural ability of an alert patient to splint their neck with muscle tone (Horodyski et al, 2011), so ROM had to be induced by a third party. Testing was carried out on an intact spine before instability was created at C5–C6. Like other studies, a repeated-measures design was used, with all movements repeated twice on each cadaver. As multiple comparisons were included, the Bonferroni adjustment was used; this reduces the likelihood of obtaining false positives when multiple pair tests are carried out, as more hypotheses are being tested, limiting the probability of identifying at least one significant result that is down to chance (Napierala, 2012).
The results showed that there was significantly more motion when the spine was unstable in all measures except extension where, although the extension measurement was greater in the unstable spine, it was not statistically different (P=0.59). In the unstable spine, there was no significant difference between using collars and no collars although the collars did restrict motion (Horodyski et al, 2011). Flexion with the collars in place was 17–41% of the control range and, while flexion did occur, the collars reduced it by 30–40° in comparison to no collar; this was similar among all collars and each plane of movement. Horodyski et al (2011) concluded that conscious, alert patients deliver internal stability using normal muscle tone and strength through pain, inducing a stabilising effect. This was supported by Benger and Blackham (2009), who concluded that an alert, stable and cooperative patient does not need to be immobilised. However, for those with a reduced level of consciousness and who are unable to protect their own cervical spine, immobilisation is an appropriate level of protection (Benger and Blackham, 2009).
Ultimately, the cervical collar cannot be expected to implicitly immobilise a cervical spine but should be used alongside other spinal immobilisation techniques for effective stabilisation to take place (Horodyski et al, 2011).
While Houghton and Driscoll (1999), Horodyski et al (2011) and Holla (2012) all looked at the effectiveness of correctly fitted cervical collars, Bell et al (2009) looked at the ROM in poorly fitted collars. The rationale behind this study was that the optimal testing conditions seen in other studies do not offer a realistic representation in the emergency clinical setting (Bell et al, 2009). Sundstrøm et al (2014) support this, suggesting that many collars are not fitted correctly prehospitally. To carry out the study, Bell et al (2009) used 12 healthy men with no history of spinal injury and mean age of 29.44 (SD 6.598 years), comparable to Houghton and Driscoll's (1999) study where the average age was 27; these ages reflect the patient population, as almost half of those with SCI are aged 16–30 years (Casey, 2017). While men are more likely to sustain a traumatic SCI (Casey, 2017), an all-male study does not represent the population.
As with previous studies, a repeated-measures design was used, with a correctly sized collar applied, as well as one size too big and one size too small. The motion resembled everyday life with movements as far as possible without pain and discomfort, and the Student's t-test was used where P=<0.05 to determine significant difference (Bell et al, 2009). Results showed that less movement was allowed in all primary motions in the correctly sized collar than in the incorrectly sized collars (Bell et al, 2009). Significant differences were seen in axial rotation and right lateral bending as well as in extension using the collar that was too big and left lateral bending in the one that was too small.
While even a correctly fitted collar can allow up to 30o of motion (Benger and Blackham, 2009), a patient wearing an incorrectly sized cervical collar could experience added cervical impairment because of a lack of restriction and under-restrained motion of the neck, giving rise to significant clinical implications (Bell et al, 2009). An estimated 3–25% of SCIs occur following the initial trauma through secondary injuries (Askins and Eismont, 1997), although it is not known how many secondary SCIs have been prevented by cervical immobilisation (Sundstrøm et al, 2014). The healthy subjects in this study are not representative of the injured population, as movement is discouraged. However, this model of maximum exertion could represent conditions experienced through involuntary motions leading to secondary injury (Bell et al, 2009). Horodyski et al (2011) discusses that maximum ROM is never established on a patient in a hospital or prehospital setting; the study tested the effect of collars on ROM as a source of protection.
While immobilisation is essential in preventing secondary injury (Houghton and Driscoll, 1999), it is debated whether cervical collars achieve this. Additionally, Bell et al's (2009) study includes a sound discussion that cervical collars applied prehospitally may be incorrectly sized, creating substantial clinical implications and detrimental effects for unconscious patients, while conscious patients are able to deliver internal stability using normal muscle tone and strength (Horodyski et al, 2011).
Nevertheless, all studies corroborate that cervical collars restrict movement but do not implicitly immobilise a cervical spine. Horodyski et al (2011) suggest using collars alongside other immobilisation techniques. In contrast, Holla (2012) suggests that rigid cervical collars do not provide any significant additional immobilisation to head blocks and have adverse effects so should be reconsidered, and that a more appropriate technique to immobilise the cervical spine is required.
Conclusion
Cervical collars are an accepted form of cervical immobilisation, and are prominent in the prehospital management of suspected SCI in the UK. However, recent evidence suggests that cervical collars can do more harm than good, contradicting current UK ambulance guidelines for spinal immobilisation.
The first theme arising from this review is that time in a cervical collar needs to be minimised to prevent adverse effects. However, the studies can be questioned because inaccuracies and the use of outdated practice potentially skew the results. Importantly, the studies failed to discuss the more severe adverse effects that can affect patient outcome. However, they included the need to identify worsening signs and symptoms when a cervical collar is in place.
The second theme, on ROM, discussed whether a cervical collar achieves immobilisation using a combination of living participants and cadavers but no real patients. An immediate weakness of the studies included were sample sizes; however, it was determined in one study that increasing the number of participants would not affect the outcome as using the best cervical immobiliser can be identified through the ROM it allows. Nevertheless, all studies agreed that cervical collars restrict movement but do not implicitly immobilise a cervical spine.
Limitations
The articles comprised quantitative studies only, which suggests a lack of comprehensive and varied research, weakening the conclusions. Therefore, further research, preferably randomised controlled trials, to compare alternative immobilisation techniques, as well as qualitative studies, are required to overcome this and provide the basis for further evidence-based guidelines for the prehospital setting. However, the range of locations, sample sizes, time frames and methodologies strengthen the conclusions.
A limitation in some of the studies is a weakness of evidence in documentation, which is highlighted throughout. Moreover, as a systematic literature review was not undertaken, evidence may have been omitted; for example, that on more severe adverse effects such as aspiration and respiratory compromise.
Implications and recommendations
Given that cervical collars do not provide any significantly increased additional immobilisation and the adverse effects of a cervical collar can be detrimental to patients, the UK Ambulance Service guidelines need to be re-examined in light of the evidence presented within this review and, specifically, removing cervical collars from prehospital practice should be considered.

