Out-of-hospital cardiac arrest survival is improved by bystander cardiopulmonary resuscitation (CPR) as a bridge to the arrival of trained resuscitators (usually from emergency medical services; EMS). Chi et al (2010) concluded that chest compressions to the standard 2-inch (5.1 cm) depth required about 500 Newtons of force (112 pounds of force or 51 kg of mass on Earth). This suggests that the minimum weight of a resuscitator, EMS or otherwise, must be around 51 kg. Other studies have reported a significant difference in the quality of chest compressions between light and heavy rescuers CPR (Hasegawa et al, 2014; Contri et al, 2017). Heavier rescuers can perform and sustain high-quality chest compressions because they can use their body weight to provide chest compressions without becoming rapidly exhausted, making the weight of the rescuer critical to effective chest compressions (Hasegawa et al, 2014).
There is a weight below which achieving effective chest compressions is impossible. While Hasegawa et a's study (2014) suggested this minimum weight is roughly 51 kg, another study found 70.5 kg to be the body weight threshold for adequate chest compression depth (Oh et al, 2016). Many health professionals are below these weights, yet are required to maintain CPR certification and must demonstrate competency as a requirement for employment.
The primary purpose of this study is to determine the minimum weight required to perform sufficient chest compressions. For resuscitators below the determined minimum weight and incapable of performing sufficient conventional chest compressions, this study also explores the efficacy of alternate chest compression techniques.
Aims
In a cardiac arrest, a 911 dispatcher can often coach a bystander to perform chest compressions if CPR has not been initiated. In the case that a lightweight resuscitator such as a child has made the 911 call, coaching the child to perform chest compressions may be the patient's only chance of maintaining blood circulation until the emergency medical service (EMS) arrives.
As the weight of a resuscitator plays a role in the effectiveness of chest compressions, this study serves to determine the minimum weight required to perform sufficient chest compressions.
When a child or similarly lightweight resuscitator is below the critical weight required for this, a 911 dispatcher has limited options while the EMS is en route. Therefore, the secondary purpose of this study is to investigate the efficacy of alternate chest compression techniques performed by children below the critical weight required to perform chest compressions in the conventional fashion.
Research design
An exploratory research design was used as there was no literature provided an accurate minimum weight for resuscitators and many health professionals are under the minimum weights that have been previously suggested.
Lightweight resuscitators enrolled in the study, many of whom were children, were instructed by CPR-certified individuals on how to perform adequate chest compressions. The participants were first taught the conventional method; if the participant failed to employ effective chest compressions, they were trained in the alternative modalities, which were evaluated.
Chest compressions were performed on a manikin under rhythm assistance. A semi-quantitative approach was used to evaluate a resuscitator's chest compression efficacy for both conventional and alternative modalities.
Methods and methodology
We enrolled small adults and children aged 8 years and above as subject volunteers for this study of chest compression efficacy. Consenting adults and assenting minors (under 18 years of age) were informed of the study through written announcements and word of mouth.
Those interested in taking part contacted the investigators, and arrangements were made for the volunteers to participate at their convenience. There were no reimbursements or payment in exchange for being involved in this study. Written informed consent was obtained for adult volunteers. Parental written informed consent and study subject written informed assent were obtained for all minor volunteers. For all volunteers, investigators went over the consent form in lay language, which included exhaustion and injury from performing chest compressions, and risk to privacy as a participant's face or other identifying features may be inadvertently recorded. Methods to mitigate risk, and that the subject could withdraw from the study at any time were also discussed.
Volunteers were asked to sign only if they were comfortable with participating. Subjects with neuromuscular or musculoskeletal disorders were excluded. If a subject had previously taken a CPR course, this was recorded in the data but was not used as an inclusion or exclusion criterion.
Upon enrolment, study subjects viewed the Hands Only CPR video on the American Heart Association's (AHA) website (https://cpr.heart.org/en/cpr-courses-and-kits/hands-only-cpr). Their height and weight were measured.
Subjects were then asked to perform hands only CPR on a standard manikin (Laerdal Little Anne) on the floor (no tables or gurneys). A padded comfort mat was placed next to the manikin. Their chest compression efficacy and technique were assessed by one of the study investigators. Music was played to facilitate the compression rate.
Initially (for the first eight subjects), we played the song Stayin' Alive by the Bee Gees. However, we learned that the AHA had advocated the use of Uptown Funk by Mark Ronson and Bruno Mars, which has a slightly faster beat. Once this modification was approved by the institutional review board (IRB), Uptown Funk was used for all subsequent subjects. Study investigators gave subjects specific feedback on their efficacy and technique to improve their chest compression efficacy and stamina/endurance. Once the subject and the investigator were satisfied that chest compression technique had been optimised, the subject was given a 5-minute rest period before proceeding to the measured chest compression efficacy portion of the study.
After the rest period, subjects began phase 1 of the study, performing two minutes of music-facilitated video and audio-recorded chest compressions.
While we had access to electronic manikins that could have been used for more accurate scoring, we decided to use older manual manikins because the second phase of this study required that the subjects jump on the chest, which might have damaged electronic manikins. The manual CPR manikins produced an audible click when the 2-inch compression depth was reached. The authors set the spring/click depth to consistently click at the 2-inch requirement. A microphone was placed inside the manikin and wired into the video camera to audibly record the clicks that confirmed chest compression depth. Study investigators made a live estimate of whether the compressions had been performed adequately. If not or if the investigator was uncertain, the study subject proceeded on to phase 2 of the study.
In Phase 2, the study subject performed chest compressions by standing on the manikin's chest with both feet centred on the lower sternum (Figure 1). A horizontal bar connected to a step stool was provided for support. Subjects were instructed to hold the bar with both hands while jumping up and down on the chest. This was practised under the guidance of one of the study investigators.

Once the subject and the study investigator were satisfied that chest compression efficacy had been optimised, the study subject was given a 5-minute rest before proceeding to the measured chest compression efficacy portion of phase 2.
The subject then performed 2 minutes of music-facilitated chest compressions, which was video and audio recorded in the same manner as in phase 1. Subjects were advised that this is not an approved method of chest compressions.
We added phase 3 to the study when we noticed one of the children performing chest compressions using a squat-bouncing method. Once the IRB had approved this protocol addition, we initiated the phase 3 portion for all the subjects who failed phase 1. Phase 1 failures completed both phase 2 and phase 3.
In phase 3, subjects sat on the manikin's chest with their buttocks centred over the lower sternum. They had the option of placing both feet on one side of the manikin or straddling the manikin (forward or backward) with one foot on each side of the manikin (Figure 2). Subjects tried each method and settled on the method that they felt most comfortable with. Once the subject and the study investigator were satisfied that chest compression efficacy had been optimised, the study subject was given a 5 minute rest before proceeding to the measured chest compression efficacy portion of phase 3. The subject performed 2 minutes of music-facilitated chest compressions, which were video and audio recorded in the same manner as in Phase 2.

Videos were later reviewed by the study investigators. The total number of compressions for 2 minutes was determined. Chest compression depth was confirmed by the audible click from the manikin. Chest compression location and chest compression recoil were confirmed visually on the video. For a chest compression to be considered efficacious, all parameters (depth, location and recoil) had to be met. All data values were recorded in a spreadsheet along with comments about the chest compressions.
The initial protocol 2018-00844 which included phases 1 and 2 was approved by the IRB in March; the revised protocol to use ‘Uptown Funk’ instead of ‘Stayin’ Alive’ was approved in July; and the revised protocol to include phase 3 was approved by the IRB in November (all in 2019).
Results
The demographics and mean successful chest compressions of the 57 subjects are summarised in Table 1. In March 2020, during the early COVID-19 restrictions, enrolment had to stop because of mandated social distancing measures. Since it appeared that the authors would not be able to resume enrolment soon, they closed the study.
| Age group | 8–10 years | 11–17 years | 18 and above | All |
|---|---|---|---|---|
| All | 23 | 11 | 23 | 57 |
| Male | 12 | 2 | 5 | 19 |
| Female | 11 | 9 | 18 | 38 |
| Mean age±SD (years) | 8.6±0.7 | 12.5±1.6 | 33.0±10.9 | 19.2±13.5 |
| Mean weight±SD (kg) | 31.0±6.8 | 39.7±9.8 | 55.8±8.4 | 42.7±13.8 |
| Weight range (kg) | 20.0–45.3 | 28.0–63.5 | 44.6 to 76.1 | 20.0 to 76.1 |
| Mean height±SD (cm) | 133.6±8.3 | 150.8±7.6 | 160.9±6.9 | 147.9±14.6 |
| Height range (cm) | 120–150 | 142–168 | 151–175 | 120–175 |
| Took a CPR course | 0 | 2 | 20 | 22 |
| Mean successful chest compressions±SD | 59±77 | 166±92 | 221±16 | 145±97 |
After initial scoring of total successful compressions during the 2-minute period, the scores of three subjects were modified as described in Table 2. Since the purpose of this study is to determine physical capability of performing chest compressions and not factors such as frustration, anxiety and cooperation, the authors felt these scoring modifications were justified and more accurately represented the subjects' physical potential to perform compressions effectively.
| Age/weight | Data modification |
|---|---|
| 19 (52 kg) | Originally scored as 131 compressions. Subject completed 86 of 92 successful compressions in the first 45 seconds; did 13 of 44 successful compressions for the next 23 seconds; then stopped for 17 seconds; then did 40 of 50 successful compressions from 80–104 seconds; then stopped and gave up. In reviewing the video, it was evident she is capable of performing at a rate of 86–92 successful compressions for the 120-second time period. We adjusted her score to 229 compressions (86x120/45). |
| 10 (45kg) | Originally scored as 93 compressions. She completed 93 of 139 successful compressions, then stopped at 1:08. She claimed to be fatigued but stopping appeared to be owing to a lack of cooperation rather than a physical incapability. We adjusted her score to 164 compressions (93x120/68). |
| 11 (39kg) | Originally scored as 24; she did not succeed but we asked her to stop at 1:04. She was clearly tiring so correcting her score would not double her score. Scoring her at 24 would be unfair since we asked her to stop once we knew she would not succeed as she was getting fatigued. We chose to adjust her score to 36. |
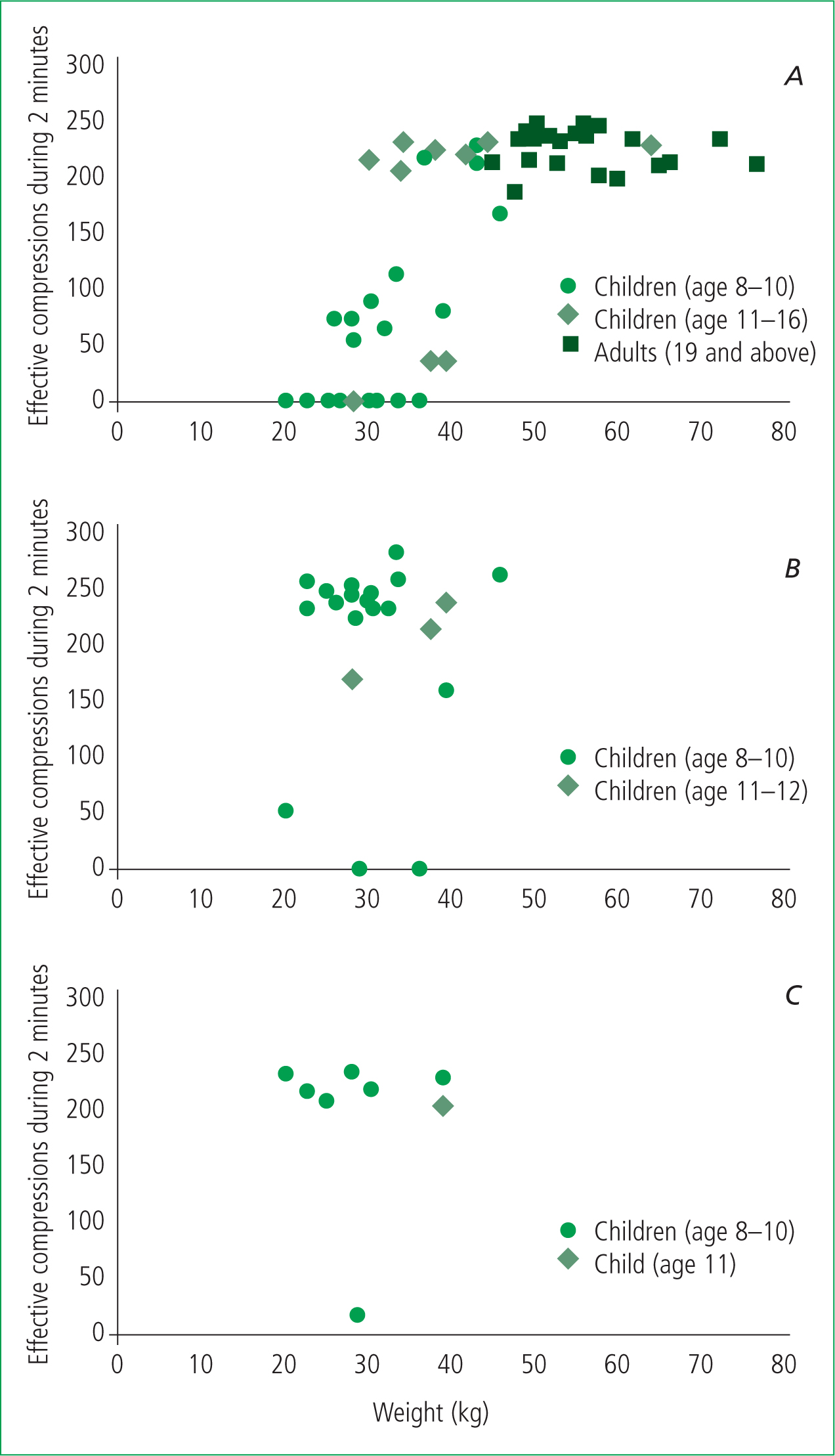
Figure 3 plots successful chest compressions using the three methods (A: conventional; B jumping; C: squat-bouncing) by weight among the three age groups. Subjects were able to complete nearly 200 conventional compressions in 2 minutes if their weight was above 40 kg. Some subjects in the 30–40 kg weight range were able to achieve 200 compressions or more, but many were not. In subjects below 30 kg, the success rate was very low. The successful subjects in the 30–40 kg weight range were taller (148 cm versus 138 cm) and older (11.0 versus 9.2 years) but not heavier (34.5 kg versus 35.5 kg).
Twenty-three subjects who failed phase 1 went to on to phase 2. Using the jumping method, 20 of 23 achieved at least 150 successful compressions. One person nearly fell when they started, at which point, phase 2 of the trial was terminated. One person performed the compressions but did not permit the chest to sufficiently recoil despite counselling. One person performed 88 successful compressions but frequently stopped. These two subjects failed because of developmental non-cooperation issues, not because of physical incapability. In the authors' assessment, all subjects had the physical potential to successfully deliver sufficient compressions for two minutes.
Eight subjects who failed phase 1 completed phase 3. Seven of the eight subjects were able to complete nearly 200 effective compressions. The only failure occurred in a child who stopped, claiming to be tired, which was a developmental non-cooperation issue rather than a physical incapability.
Discussion
The data in this study suggest that a weight below 30 kg is insufficient to provide effective standard chest compressions. Some people in the intermediate 30–40 kg weight range can do chest compressions sufficiently, but some cannot. A weight above 40kg is sufficient to perform effective chest compressions.
In the event of a cardiac arrest and only a child bystander is available to perform chest compressions, if the child weighs at least 40 kg, performing sufficient chest compressions may be possible and considered by a 911 dispatcher.
The critical resuscitator weight of 40 kg found in this study (or greater in other studies), is fairly low for an adult. The critical weight of a resuscitator found also assumes normal neurological and musculoskeletal strength (Chi et al, 2010; Oh et al, 2016; Mpotos et al, 2017). Weaker resuscitators weighing >40 kg may still have difficulty in performing sufficient chest compressions, which this study does not thoroughly assess as individuals with neuromuscular or musculoskeletal disorders were excluded from the study.
Furthermore, larger victims will require greater weights and forces to compress their chests. The ability to perform chest compressions on those of larger body habitus has become increasingly important as obesity has become more prevalent. Thus, an alternative means of chest compressions might have greater applicability when considering factors such as resuscitator endurance and victim body habitus.
Small subjects who were not able to perform conventional effective chest compressions were usually able to achieve effective chest compressions using the jumping and squat-bouncing methods. In reviewing the jumping method phase 2 videos, there were three basic patterns of jumping: keeping the feet in constant contact with the chest, but not jumping high enough to achieve optimal chest recoil or effective chest compressions (three subjects); keeping the anterior soles in constant contact with the chest but jumping so that the heels, which are used to achieve chest compressions, are raised off the chest, which maintains a more constant position on the lower sternum (10 subjects); and the feet lose contact with the chest to generate enough downward force to achieve effective chest compressions, with some movement of the chest impact site (nine subjects).
Most of the time, chest compressions were effective, not excessive, and appropriately located. However, two subject videos demonstrated that jumping can render a significant downward force and some compressions appeared to be excessively deep. An additional seven subject videos demonstrated that, since the resuscitator is jumping with two feet, if the feet lose contact with the chest, one foot might be in the ideal place, but the other foot could be on the upper sternum, the xiphoid, the lower ribs or on the abdomen (Figure 4). While the heart would have been compressed effectively, the misplacement of the other foot puts the victim at risk of chest fracture or organ injury. The benefit of a sufficient cardiac compression must be weighed against the risk of chest fracture and/or organ injury.

In a study comparing manual human chest compressions and automated mechanical load-distributing band chest compressions, the automated mechanical compressions resulted in more posterior rib fractures, sternal fractures, vertebral fractures and pneumothoraces, but a lower risk of liver and spleen injuries (Sonnemans et al, 2020). These automated mechanical chest compression machines are considered to be an acceptable alternative to manual chest compressions. There is therefore an accepted precedent chest compression efficacy can be traded off with injury risk.
In reviewing these jumping videos, the second method of maintaining chest contact with the anterior feet while jumping has the best chance of maintaining the proper position on the chest. Additionally, the feet need to be together (not apart) to more accurately target the lower sternum for the chest compression. However, lighter children might need to jump off the chest to generate sufficient downward force for a sufficient chest compression.
In contrast, the squat-bouncing method had less potential to for chest compressions to be provided in the wrong place. We also noticed that the straddling method resulted in better stamina and better chest recoil than the non-straddling method (with both feet on the same side of the manikin). Overall, given a 911 dispatcher's potentially limited options for resuscitator, alternate chest compression techniques such as jumping and squat-bouncing may be considered.
Height plays a significant role in the biomechanics of chest compression performance, but this was more difficult to assess since weight was the dominant factor (Edelson et al, 2012). One of the subjects, who weighed 37.3 kg, should have been heavy enough to perform the chest compressions but could not because he was not tall enough for his body to be directly over the mid chest. He had to compress at an angle, which was more difficult and less effective. If a thick couch cushion had been placed under his knees, this would have improved his compression angle favouring his ability to generate a sufficient downward force.
This study focused on the physical ability to perform chest compressions. However, small weight is associated with young age and its obligate developmental neurocognitive immaturity, resulting in the developmental potential for periods of non-cooperation resulting in children quitting or not performing the jumping or squat-bouncing chest compressions correctly.
Furthermore, the jumping technique theoretically poses a risk for the rescuer of falling secondary to imbalance. In this study, a folding step stool was used for balance since it was easier to transport. An emergency dispatcher could have to specifically recommended that the resuscitator locates a chair or other support structure to start chest compressions.
These are all realistic limitations in these alternate methods that 911 dispatchers would have to manage in their coaching attempts for young resuscitators. However, if a child has called 911 and this child is the only available resuscitator, the 911 dispatcher has limited options. Coaching an initially non-cooperative child or asking a child what other furniture is available to be used for stabilisation would likely be a better course of action than doing nothing for the individual who requires resuscitation.
The development of alternate methods of chest compressions for small resuscitators could provide an additional option for 911 dispatchers. Even adults with sufficient weight to perform chest compressions might become too tired to continue them. An alternate chest compression technique could provide fatigued adults with another option for continuing chest compressions until EMS arrives.
Limitations
A limitation of this study was its small sample size. This could easily have been increased this by enrolling more adults, but would not have addressed the objective of this study. In addition, the COVID-19 pandemic forced the authors to close the study early. Fortunately, there were enough study subjects around the transition point sought.
This study gave study subject resuscitators immediate and constant feedback confirming sufficient compression depth with an audible click. This is artificial since in reality this kind of feedback is not available. Resuscitators must know how far to compress and child resuscitators must know how high to jump or squat-bounce.
Other studies have determined other minimum weights greater than our 40 kg weight are required to perform chest compressions (Chi et al, 2010; Oh et al, 2016; Mpotos et al, 2017). This could be because of the manikin model used. Although the authors adjusted and confirmed the clicking of the manikin to be slightly greater than 2 inches, they could not adjust or replace the spring. The force required to compress the spring could be lower as the steel spring fatigues with use.
Without doing sophisticated measurements, all four study investigators have attempted chest compressions on different manikins including the manual manikin, a computer-automated manikin, and the AHA CPR Anytime inflatable manikin. All three require a different level of force. Different manikins have varying requirements for successful chest compressions (Baubin, 1995). Additionally, human victims have different chest characteristics, so different forces are required for chest compression. Thus, in reality, our study's minimum weight requirement was determined for a specific manikin and cannot necessarily be extrapolated to all patients.
Regardless of what the critical weight is, if the only bystander weighs less than this, the present study suggests that there might be other options to perform chest compressions. This requires further study and refinement to determine the best alternate means of performing chest compressions.
Conclusions
A weight below 40 kg in this manikin model results in a decline in the ability to perform effective standard chest compressions. For small resuscitators, the jumping and squat-bouncing methods result in sufficient compressions most of the time. However, there are concerns regarding chest recoil, excessive compression depth and off-centre compressions that could result in injury.

