Essex and Herts Air Ambulance Trust (EHAAT) operate two doctor-paramedic, pre-hospital HEMS teams to provide support to local ambulance crews. The service is predominantly helicopter-based but operates a rapid response car outside daylight hours or in poor weather. The total population covered numbers approximately 3 million people. The team responds to major trauma and medical emergencies, with the latter accounting for approximately 20% of all missions. The paramedics who work for the service are employed by the East of England Ambulance Service NHS Trust, and are seconded to EHAAT for a fixed period. A comprehensive selection process is undertaken and an extensive training programme covering aviation practice and extended clinical management is in place for successful candidates. In addition, EHAAT paramedics have been among the first to enrol and undergo enhanced skill training in anaesthetics and intensive care medicine as part of a formal education programme. We believe that one of the strengths of the service provided by EHAAT lies in our paramedics acting as role models and ambassadors for both our service and the ambulance service in general.
The case
A 55-year-old man lost control and was ejected from his motorcycle at approximately 60 miles per hour on a country road. The patient was wearing a helmet and full protective clothing. When the first ambulance service personnel arrived on scene, the patient had a respiratory rate of 22 breaths per minute. He was hypotensive with a blood pressure of 90/60 mmHg and tachycardic with a heart rate of 100 beats per minute. Oxygen saturations were 97% on a reservoir mask. He was conscious, alert, and had not been unconscious at any time. Intravenous access was secured, analgesia with morphine was provided, and manual spinal immobilisation was established. The patient reported difficulty breathing and told the crew: ‘I think I've collapsed my left lung.’ A clinical examination by both the paramedic land crew and the EHAAT team revealed a fractured left clavicle and left-sided posterior rib fractures with palpable sub-cutaneous emphysema and reduced air entry on auscultation of the left side of the chest. Despite a thorough assessment, there were no clinical findings to suggest an alternative cause, such as haemorrhage or spinal cord injury, that may otherwise have explained the patient's hypotension. In addition, during the period of assessment, the patient's respiratory rate had increased to 26 breaths per minute and breathing had become noticeably more laboured indicating a dynamic and progressive disease process. Furthermore, repeat observations yielded a blood pressure reading of 85/68 mmHg. It was decided on the strength of the history and clinical signs that the patient had developed a left-sided tension pneumothorax with the potential for imminent cardiorespiratory arrest if not relieved. The EHAAT team inserted a left-sided intercostal chest drain (ICD) on the basis of this.
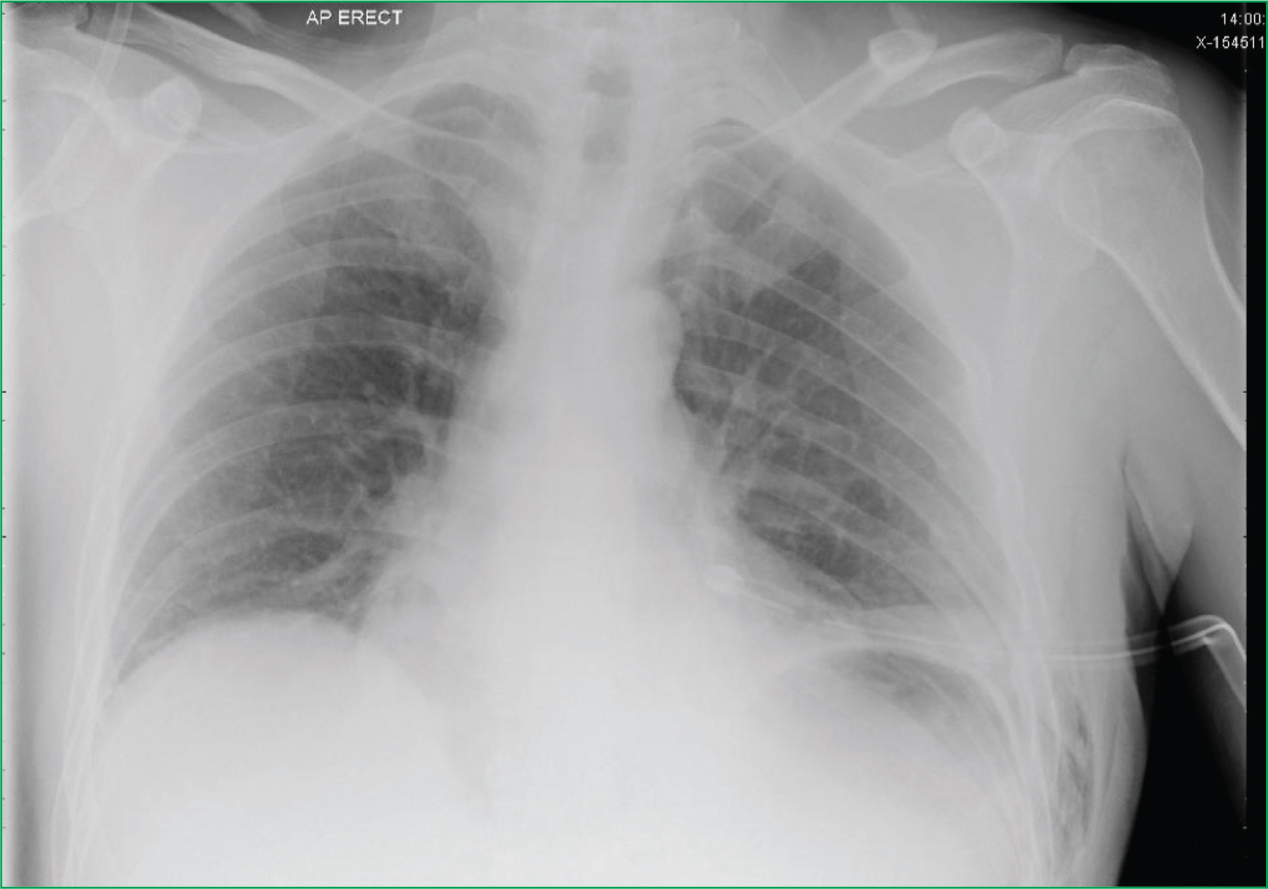
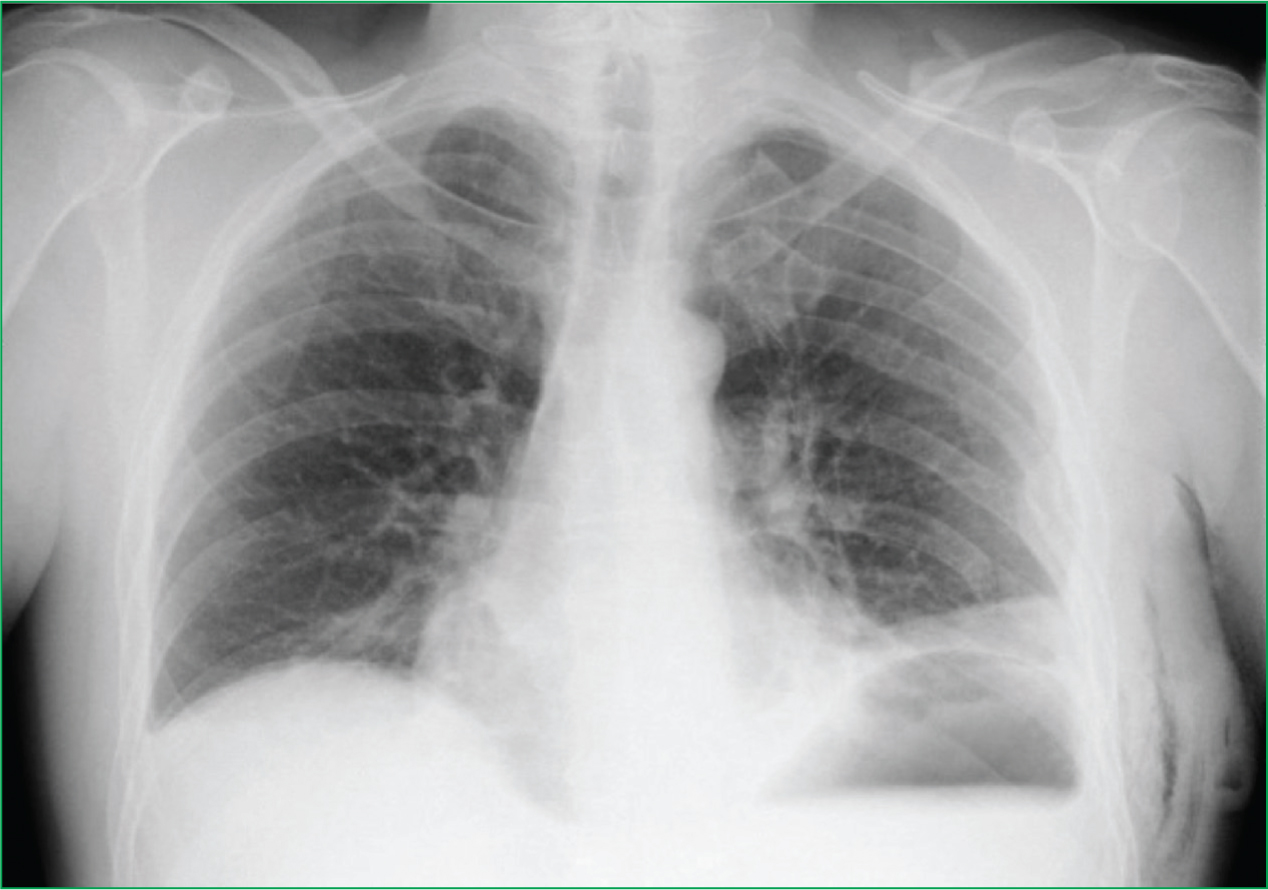
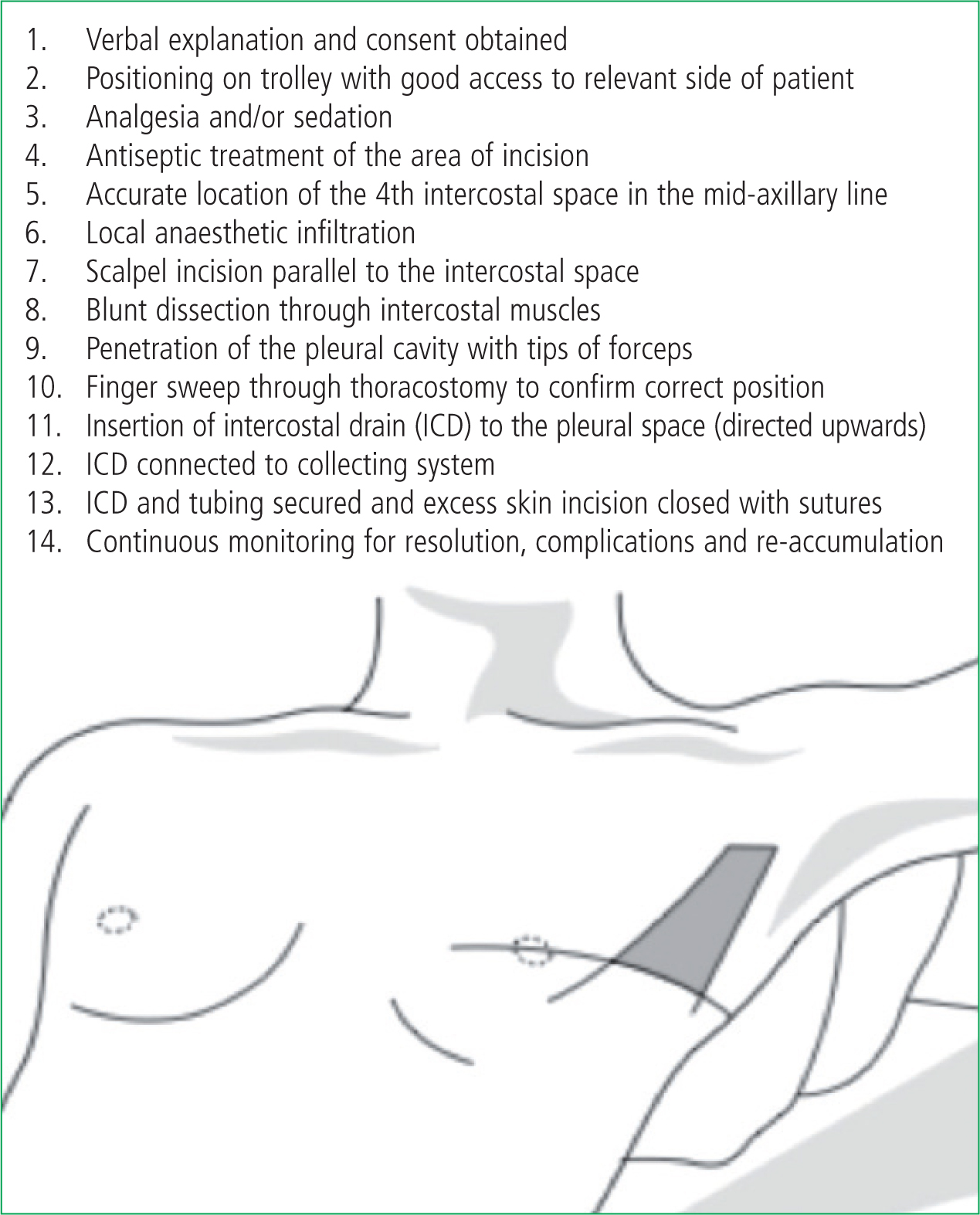
The procedure for the insertion of an ICD is outlined in Figure 3. After a left sided thoracostomy that yielded a ‘hiss’ of air from the accumulated tension in the intra-pleural space, there was an immediate improvement in the patient's symptoms. An intercostal drain was sited via the thoracostomy and secured. The patient admitted to feeling much better and a repeat set of observations showed a blood pressure of 128/73 mmHg and a heart rate of 62/minute. Oxygen saturations improved to 100%. After an uneventful transfer to a major trauma centre, the patient was handed over to the trauma team. A chest X-ray (CXR) after admission to hospital is shown in Figure 1 showing the chest drain and re-expanded lung. A further image after chest drain removal is shown in Figure 2, taken shortly before the patient was discharged from hospital.
Discussion
Applied anatomy and physiology
A pneumothorax occurs when air accumulates in the space between the visceral and parietal pleura of the lung. This can either occur following a disruption to the surface of the lung (such as a laceration from a rib fracture or a ruptured emphysematous bullous) or a penetrating chest injury, which breaches the pleura and/or penetrates the lung tissue itself. In the former, alveolar air enters the pleural space; whilst in the case of penetrating chest trauma, air may also enter through the chest wall. Either may result in a pneumothorax with lung collapse. Some clinical features of a tension pneumothorax in spontaneously breathing patients are listed in Table 1.
| Universal findings |
| Chest pain |
| Respiratory distress |
| Common findings |
| Tachycardia |
| Ipsilateral decreased air entry |
| Less common findings |
| Low oxygen saturations |
| Tracheal deviation |
| Low blood pressure |
| Rare findings |
| Hyper-resonant percussion note over ipsilateral |
| hemi-thorax or sternum |
| Decreasing level of consciousness |
| Hyper-expansion of ipsilateral chest |
Difficulties in clinical assessment
Tension pneumothorax can be a difficult diagnosis to make and ‘classical’ features, such as tracheal deviation and hyper-resonance, are often absent (Leigh-Smith and Davies, 2003). The clinical progression of this condition has been observed to differ between the spontaneously breathing and ventilated patient and is universally fatal if not treated (Perkins and Gunning, 2007). In the spontaneously breathing patient there is often a slower build-up of air within the intra-pleural space over time, leading to a more gradual clinical course. This has led some authors to suggest ‘expanding pneumothorax’ as a better term to more accurately describe the dynamic disease process. In this group of patients, chest pain and respiratory distress have been observed to be universal findings. Other common findings, as illustrated in this case study, include tachycardia and ipsilateral decreased air entry (Leigh-Smith and Harris, 2005). Ultimately, the clinical course is relentlessly progressive with the development of gradually worsening hypoxia and respiratory distress. Cardiac output is preserved until relatively late in the clinical course with hypotension and low oxygen saturations being signs indicative of more advanced disease. In contrast, a tension pneumothorax in the ventilated patient causes a more rapid progression to cardiovascular compromise and cardiorespiratory arrest (Leigh-Smith and Harris, 2005; Lee et al, 2007). This is because the positive pressure from the ventilator causes a faster rate of accumulation of air in the intrapleural space. As we highlight in this case report, there was a clinically discernible progression in the patient's deterioration, which enabled the diagnosis of a tension pneumothorax to be made. This was underpinned by a high index of suspicion in combination with attentive and continuous clinical assessment both to confirm the suspected diagnosis and refute other trauma-related reasons for hypotension, such as haemorrhage and spinal shock.
Treatment options
The two common interventions for tension pneumothoraces are needle decompression or the insertion of an intercostal chest drain (ICD). Pre-hospital enhanced care teams may often consider a third option, a simple open thoracostomy. Needle decompression and ICDs are appropriate in both the spontaneously breathing and ventilated patient. The EHAAT team will use needle decompression as a temporary measure in patients who are either trapped (and therefore inaccessible) or are deemed to be close to cardiac arrest from a tension pneumothorax. The majority of patients attended by the team who require intervention for tension pneumothorax are most efficiently dealt with by ICD insertion or will have required emergency anaesthesia and will therefore be appropriate for open thoracostomies.
Needle decompression is often a safe and therapeutic intervention (Leigh-Smith and Harris, 2005), that when performed correctly and appropriately, leads to improved vital signs (Davis et al, 2005) and clinical status (Barton et al, 1995). The potential pitfalls of needle decompression include kinking and misplacement, blockage by tissue or blood and inadequate cannula length to penetrate the chest wall (Jones and Hollingworth, 2002). False positive aspiration of air can occur in the case of intrapulmonary placement during needle decompression (Fitzgerald et al, 2008), while a false negative result may occur in the case of inadequate cannula length (Zengerink et al, 2008). A study of over 100 adult volunteers using computed tomography (CT) scanning demonstrated that at least a quarter had chest wall depths in excess of five centimetres (Givens et al, 2004). By comparison, a 14 Gauge ‘orange’ cannula is 4.5 centimetres in length). The most common site for needle chest decompression is the second intercostal space in the mid-clavicular line; however, a small study of 25 doctors who were all Advanced Trauma Life Support certified, demonstrated that only 88% knew this landmark and only 60% marked the correct position on the thorax of a mannequin (Ferrie et al, 2005). All of the incorrectly marked points were too medial, which would theoretically increase the risk of inadvertent puncture of underlying anatomical structures, such as the internal mammary artery. However, these misgivings need to be weighed against what is a potentially life-saving measure, which often improves the patient's clinical status (Barton et al, 1995) pending definitive management with an intercostal chest drain. Physicians usually site ICDs in hospital, or less commonly in the pre-hospital setting. The procedure is held to be safe and effective with low morbidity (Schmidt et al, 1998) although complication rates of up to 14% have been sited (Aylwin et al, 2008). The operating procedure for ICD insertion used by the EHAAT team is described in Figure 3.
Open thoracostomies are particularly useful for anaesthetised and ventilated patients in the setting of polytrauma (Perkins and Gunning, 2007) where they are a rapid, safe and effective intervention (Massarutti et al, 2006; Lockey et al, 2008). They allow repeated assessment by re-exploration in the event of further deterioration and can be converted to ICDs in the hospital setting.
Shared experience, decision-making, and teamwork
This case study highlights some important shared learning points. It demonstrates the importance of looking at the whole clinical picture. It highlights the importance of teamwork and consultation with the attending paramedics, who are often first on scene, and illustrates that it is a matter of clinical judgement in deciding to relieve tension in the ‘expanding’ pneumothorax. This decision relates to clinical features that indicate a severity of respiratory and haemodynamic compromise that warrant intervention and it behoves us to review those features that are pertinent to this case. First, there was the initial history with the patient complaining of difficulty breathing and feeling that he had ‘collapsed’ his left lung. Second, there was clinical evidence of respiratory distress along with decreased ipsilateral air entry and the presence of a tachycardia (all common findings in the spontaneously breathing patient—see Table 1). The authors recognise that these features could be present in a trauma patient with a simple pneumothorax. But ultimately, in this case it was the presence of worsening respiratory distress and hypotension in conjunction with the other clinical findings that indicated progression to a more advanced stage in the disease process. This deterioration heralded the potential for further demise and cardiorespiratory arrest. Although it was the haemodynamic compromise that provided the tipping point for immediate and definitive intervention, it is worth mentioning that it is hard to be entirely prescriptive about the point when intervention for an ‘expanding’ pneumothorax should take place. Indeed, some authors draw our attention to the use of more ‘algorithimic’ approaches encompassing clinical features such as oxygen saturations and systolic blood pressure to guide management for pleural decompression (Massarutti et al, 2006; Fitzgerald et al, 2008). What is key here is that the decision to intervene was made after careful consideration of the complete clinical picture, and following the involvement of the entire team on scene attending the patient. This shows the level of teamwork and inclusivity that we strive to achieve. It meant that any delay to definitive management was minimised and the patient could be treated quickly and effectively.
Conclusions
A tension pneumothorax can progress to cardiac arrest unless it is relieved. The decision to perform needle chest decompression depends on the degree of compromise of the patient, and the limitations of the procedure must be borne in mind. Other treatment options are available if enhanced care teams attend. This case emphasises the value of a good initial patient assessment and meticulous continuous evaluation of the clinical situation. It also shows that the diagnosis is not easy to make in a dynamic clinical setting, especially when other potential causes for haemodynamic compromise exist.

