North East Ambulance Service NHS Foundation Trust (NEAS) covers the north east of England and employs around 1 000 accident and emergency staff across 57 locations who serve a population of 2.6 million people.
As part of the NEAS drive to improve patient care, a sepsis screening tool (SST) was introduced into practice in April 2012 (Figure 1) based on the recommendations of the Surviving Sepsis Campaign (Dellinger et al, 2008). These recommendations were later superseded in the ‘Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012’ (Dellinger et al, 2012).
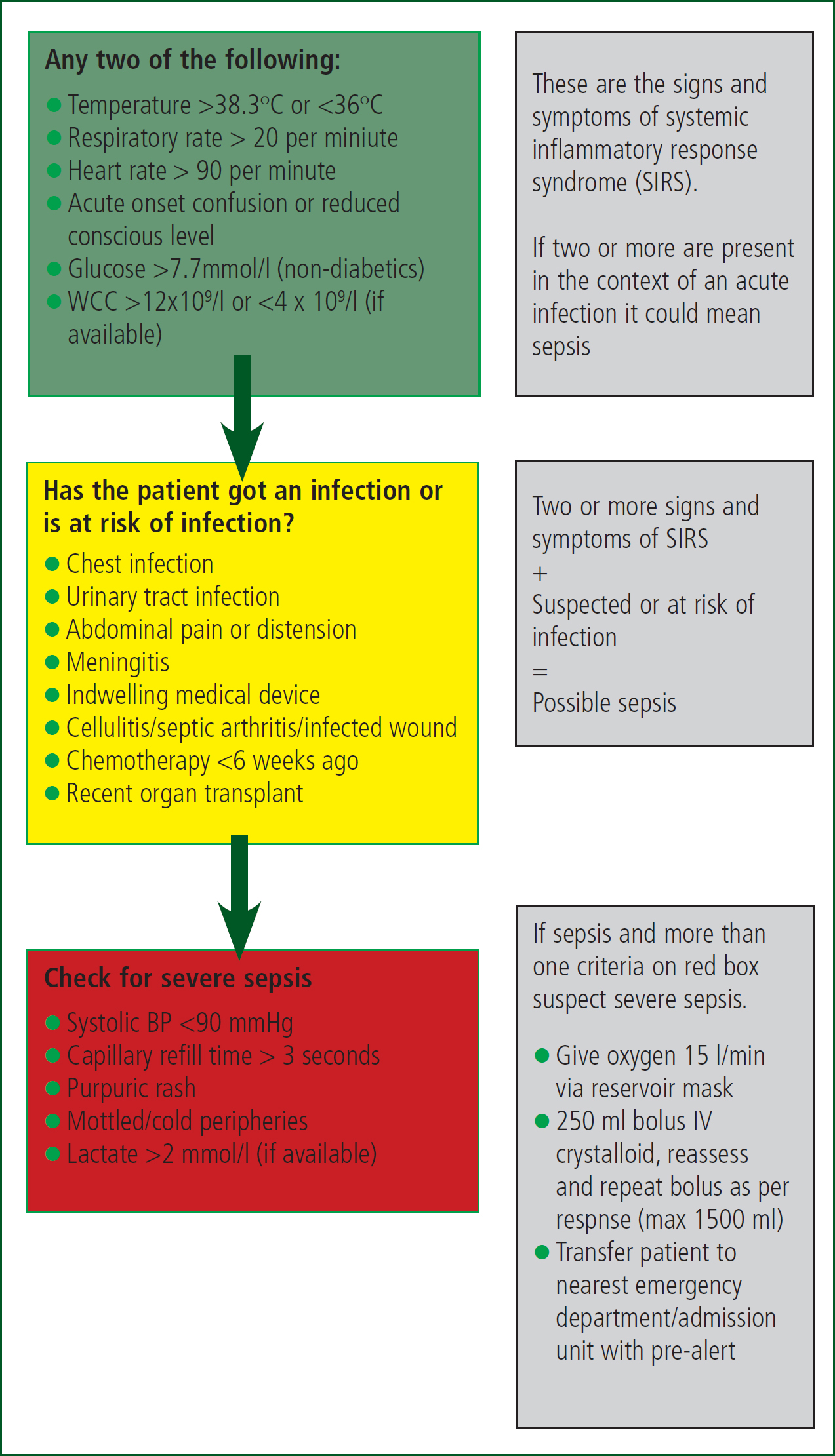
One of the criteria for severe sepsis on the SST is a lactate of >2 mmol/L, which NEAS paramedics have previously been unable to measure. The potential use of lactate in pre-hospital care has been reported elsewhere by the authors (McClelland et al, 2012) and provided some of the background for this study.
Sepsis is a condition which kills between 36 000 and 64 000 people each year in the UK (Daniels, 2011). Recent research has shown that a large number of patients with sepsis arrive at hospital by ambulance (Gray et al, 2013; Groenewoudt et al, 2014) and that paramedic recognition can lead to early access to appropriate treatment with significant impact on patient outcomes (Seymour et al, 2012; Studnek et al, 2012; Guerra et al, 2013).
There have been a number of recent studies examining the use of point-of-care (POC) lactate testing in pre-hospital sepsis care. Hokanson et al (2012) conducted a pilot study of paramedic use of temporal artery thermometers and POC lactate measurement to aid sepsis recognition. This demonstrated that paramedics could reduce the time taken to get an initial lactate reading by between one and two hours and suggested that POC lactate was possible but needed further investigation.
Guerra et al (2013) conducted a small study investigating emergency medical service (EMS) use of a sepsis alert protocol and the use of POC venous lactate meters. In this study EMS staff failed to identify 52% of the patients who were ultimately diagnosed with severe sepsis on arrival at the ED. They concluded that the widespread use of lactate meters could significantly improve the pre-hospital screening tool that was used.
Whereas the studies described above focused on sepsis as a condition where POC lactate may have value, other studies have considered the applicability of POC lactate to a wider population. Mullen et al (2014) looked at non-trauma patients transported by a US aeromedical service and concluded that POC lactate may correlate with mortality but again called for further work. Jansen et al (2008) compared lactate with other traditional pre-hospital observations, such as blood pressure and heart rate. Compared with traditional observations lactate measurement provided improved information regarding mortality.
Tobias et al (2014) conducted a study involving 673 patients, examining the link between prehospital intravenous (IV) resuscitation and mortality, and showed that elevated lactate is moderately associated with mortality. This group compared lactate as a single measure with a pre-hospital critical illness score and found that they were comparable, although the value of lactate may be greatest when combined with other observations in order to identify, or stratify, high-risk patients.
Overall the literature shows that lactate has the potential to aid in identifying and stratifying of critically ill patients, including those with severe sepsis. It has been recognised that there is a gap in the evidence around the use of POC lactate testing within UK ambulance services.
Aims
This study was designed to examine the feasibility, and potential impacts, of introducing POC lactate measurement into pre-hospital care within NEAS. The primary objective was to evaluate the Nova StatStrip Lactate Xpress for POC lactate measurement in the pre-hospital environment. The secondary objectives were to investigate what impact adding POC lactate would have on the SST, and to assess what effect lactate measurement would have on the end disposition of patients.
Methods
Participants for the evaluation were recruited from NEAS Enhanced CARe (ECARe) paramedics. ECARe paramedics are paramedics who have undergone additional training in the assessment and treatment of a range of minor injuries and presentations. The recognition and treatment of sepsis is delivered as part of the ECARe education programme. The participants were recruited by email which was sent to all of the ECARe paramedics. Ten staff responded to the initial invitation. All ten respondents were asked to attend a 90-minute training session. Nine of the ten respondents were able to attend the training session.
The 90 minute training session involved background information on lactate and its potential uses in health care and teaching the volunteers how to take both a capillary and venous lactate sample using the Nova StatStrip Lactate Xpress. The session involved continuous assessment, with the volunteers demonstrating competence taking capillary samples before they were issued with an evaluation device and lactate test strips.
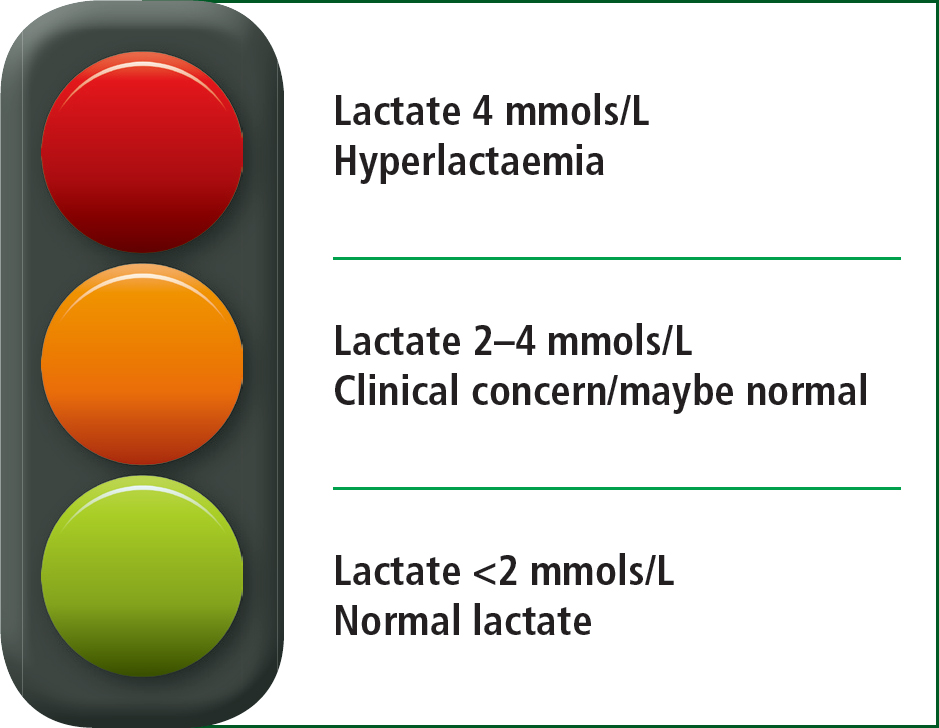
To interpret the results the participants were taught to use the Lactate Traffic Light (Figure 2), which was created by the authors to aid participants to identify normal, raised and hyperlactaemic levels. The participants were also trained to perform quality checks on the devices, and how to complete the relevant paperwork relating to the evaluation.
Participants were directed to take lactate readings on patients that presented with suspected sepsis or those who met the NEAS major trauma bypass criteria. They were asked to record their findings in the patients records and on the devices log sheet. If the reading was taken for suspected sepsis an additional form was completed, which was used to evaluate the paramedic's rationale for using the device. These forms allowed an evaluation of the effect that POC lactate had on the SST, by highlighting which components of the SST that identified patients as having suspected severe sepsis, and whether the inclusion of lactate measurement would have identified additional cases.
Participants only used the lactate meter when blood was already being taken for the purpose of measuring a patient's blood glucose or through the process of IV cannulation so no additional invasive procedure was needed.
In total there were six Nova StatStrip Lactate Xpress devices to evaluate and nine trained staff, so in order to maximise device usage and staff exposure participants had to share devices where practicable. The target sample was 200 patients over six months, this target was set based on an evaluation of ECARe paramedic workload and previous research that the authors had undertaken on sepsis screening (McClelland and Younger 2013). During the evaluation it was decided that the target of 200 was overly ambitious, therefore a decision was made to extend the evaluation period for a further three months with a reduced target of 100 patients.
At the end of the evaluation the participants were asked to complete an overall evaluation of the device and asked for feedback on how they felt the device acted in pre-hospital use and whether it had any effect on their practice. In order to allow for purposeful analysis of the data, a series of questions were asked with the responses being recorded on a five-point Likert scale (Thomas, 2011).
Results
114 patients (58% female, mean age 70 years, range 6–100) had lactate levels recorded, 109 patients with suspected sepsis (61% female, mean age 71 years, range 6–100) and 5 trauma patients (100% male, mean age 51 years, range 10–74).
The three most common patient presentations where lactate readings were taken were ‘Non-specifically Unwell’ (40%), ‘Breathing Problems’ (17%) and ‘Abdominal Problems’ (11%).
Lactate values ranged from 0.7–11.2 mmol/L with a mean of 2.6 mmol/L.
Analysis of the evaluation data showed that 53% (n=58) of the sepsis patients met the criteria for severe sepsis according to the SST. 60% (n=35) of the severe sepsis patients met the criteria on lactate alone. All the participants felt confident using the device with the majority reporting that lactate would influence their decision in patient treatment and that patients would benefit from paramedics having this capability.
The source of the samples were recorded for each patient with 66.7% (n=76) taken from capillary samples, 29.8% (n=34) taken from venous sampling, and 3.5% (n=4) having both capillary and venous samples taken (Table 1).
| Venous reading | Capillary reading | Difference | |
|---|---|---|---|
| Patient 1 | 2.0 mmols/L | 4.6 mmols/L | 2.6 mmols/L |
| Patient 2 | 3.4 mmols/L | Failed | N/A |
| Patient 3 | 9.6 mmols/L | 11.2 mmols/L | 1.6 mmols/L |
| Patient 4 | 1.5 mmols/L | 3.6 mmols/L | 2.1 mmols/L |
Each time a test was conducted on a patient due to the SST, the paramedic was asked if the test results would have influenced their decision to treat or not to treat the patient for sepsis. The users reported that in 60% (n=54) of cases that it did, 16.7% (n=15) that it maybe affected their decision, and 23.3% (n=21) that it did not affect their decision.
93.9% (n=107) of patients were transported to hospital, 1.8% (n=2) were discharged at scene, and 4.4% (n=5) were referred to alternative pathways. Of the 6.1% (n=7) patients not transported to hospital all the patients were screened for sepsis. Two (28.6%) of the patients who were not transported to hospital had a lactate of greater than two. One met the criteria for severe sepsis but refused treatment/transport. The other did not meet the criteria for sepsis but had a slightly raised lactate at 2.1 mmols/L.
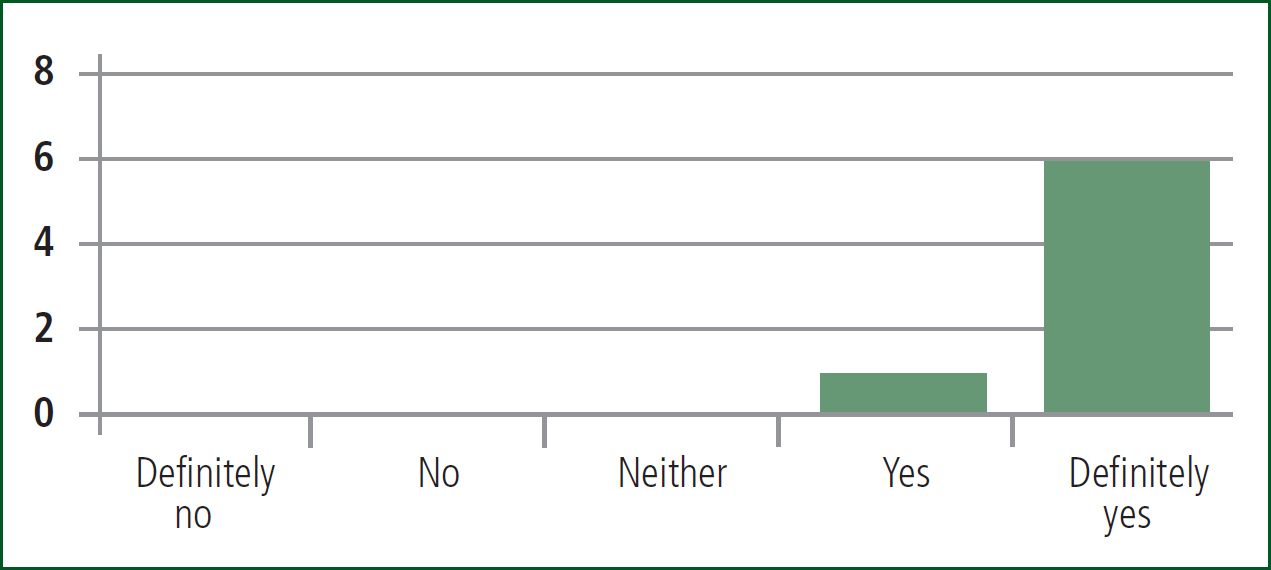
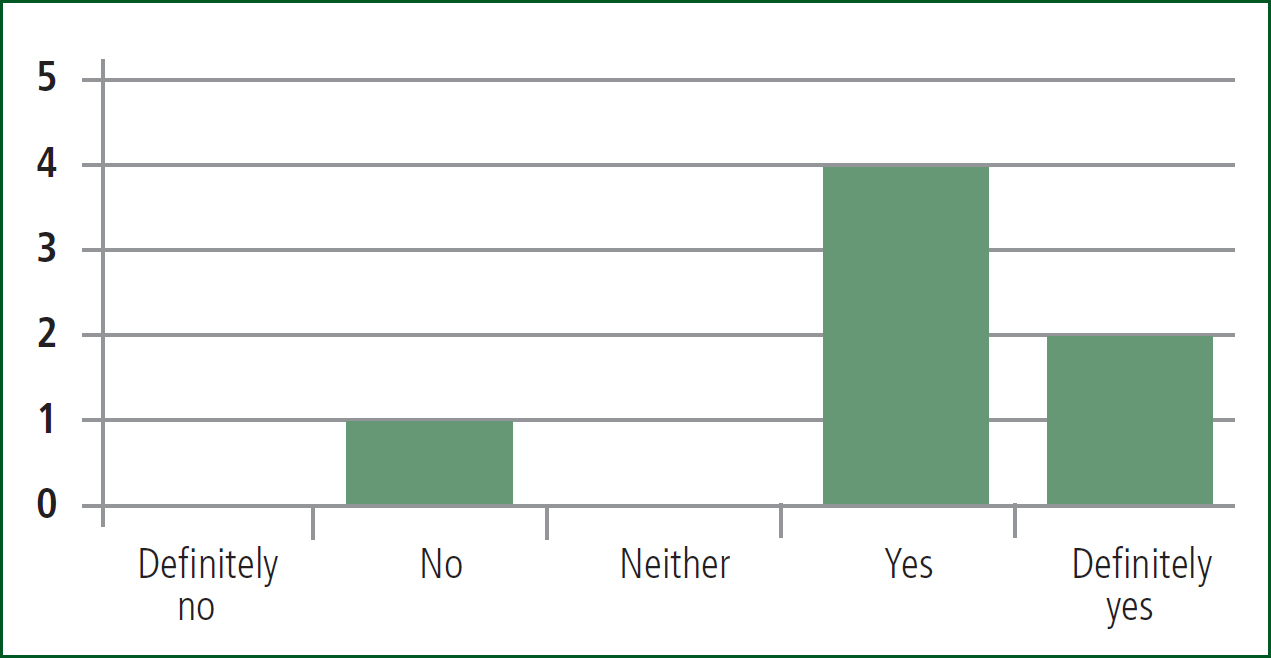
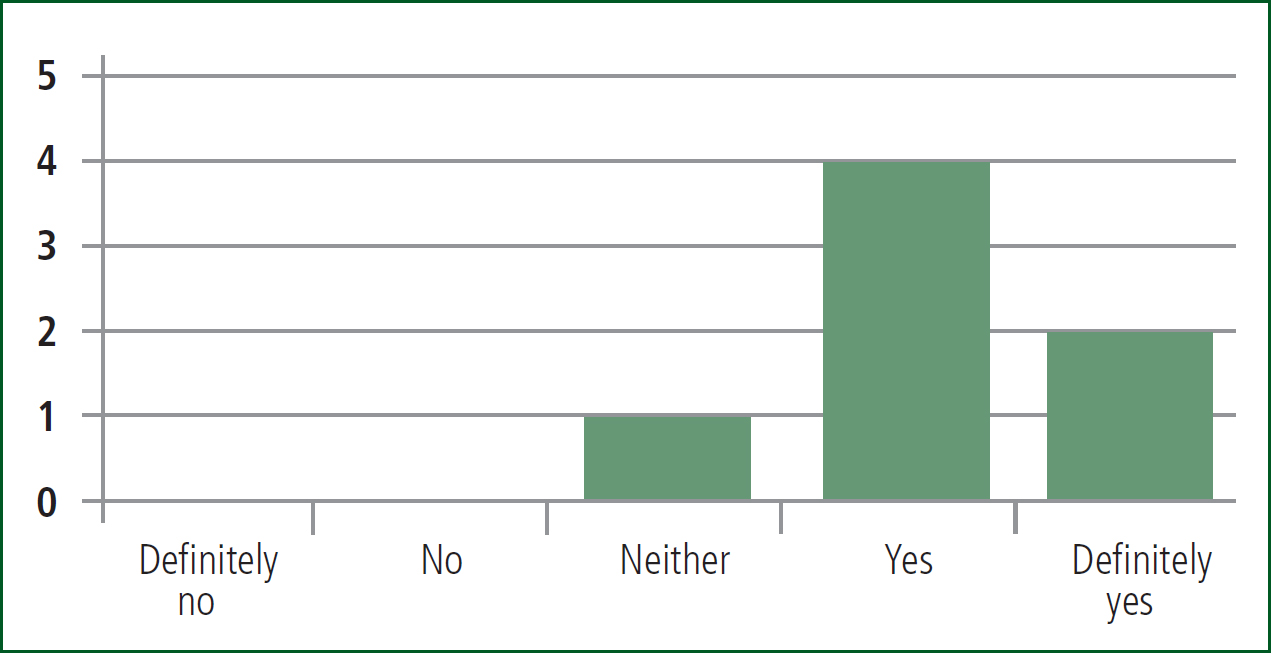
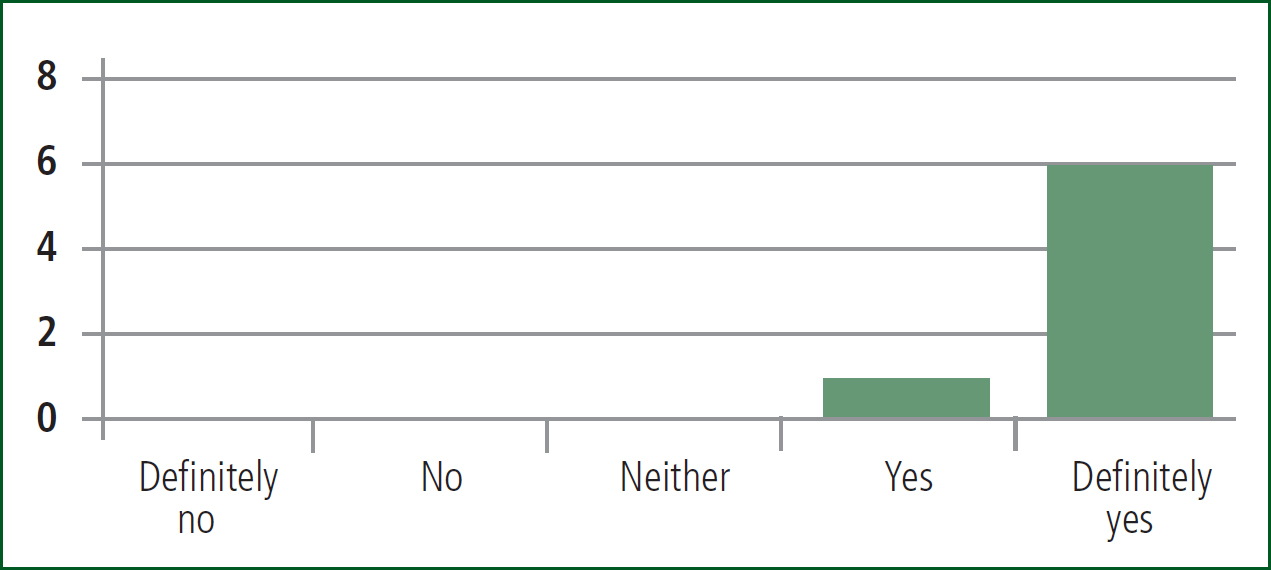
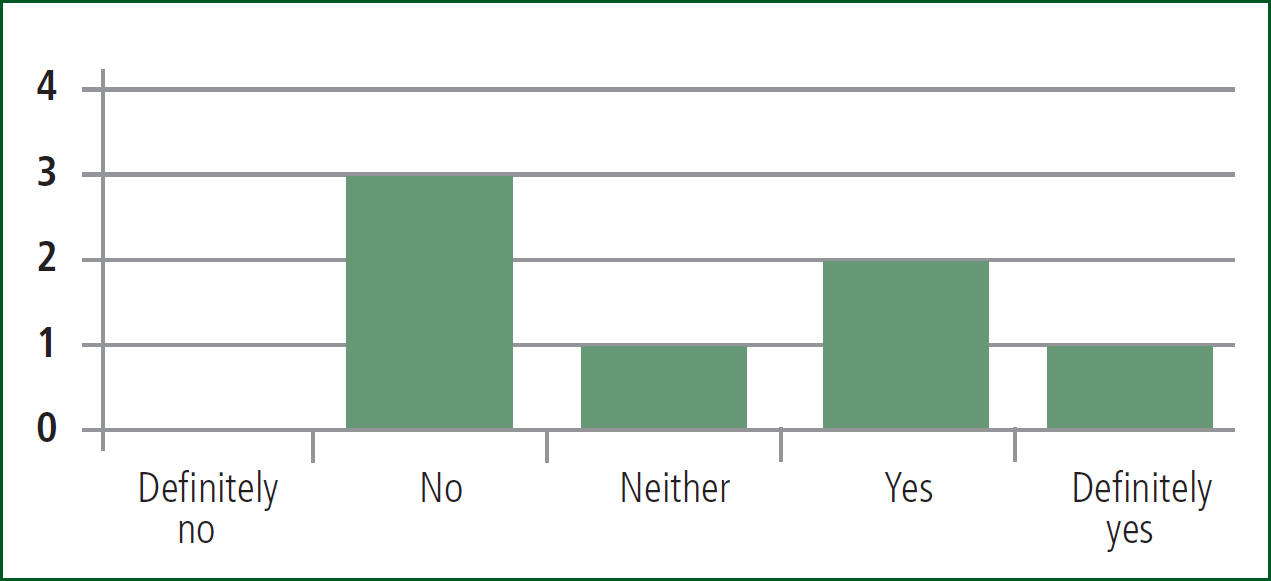
Feedback forms were completed at the end of the evaluation. Summaries of the responses are shown in Figures 3–8 below.
Discussion
This study addresses our primary objective which was to evaluate the Nova StatStrip Lactate Xpress for POC lactate measurement in the pre-hospital environment. Previous work has established that paramedics can improve their detection, and treatment, of sepsis and that POC lactate is one of the ways in which this can be accomplished. This study has focused on evaluating the method of measuring POC lactate and has shown that the Nova StatStrip Lactate Xpress is usable in the pre-hospital environment and appears to aid paramedics in confidently identifying severe sepsis.
Figures 3 and 6 demonstrate the confidence paramedics had using the device. The device is similar to the POC glucose monitor in use by NEAS, which further enhanced the usability. All the participants felt confident using the device with the majority reporting that lactate would influence their decision in patient treatment and that patients would benefit from paramedics having this capability.
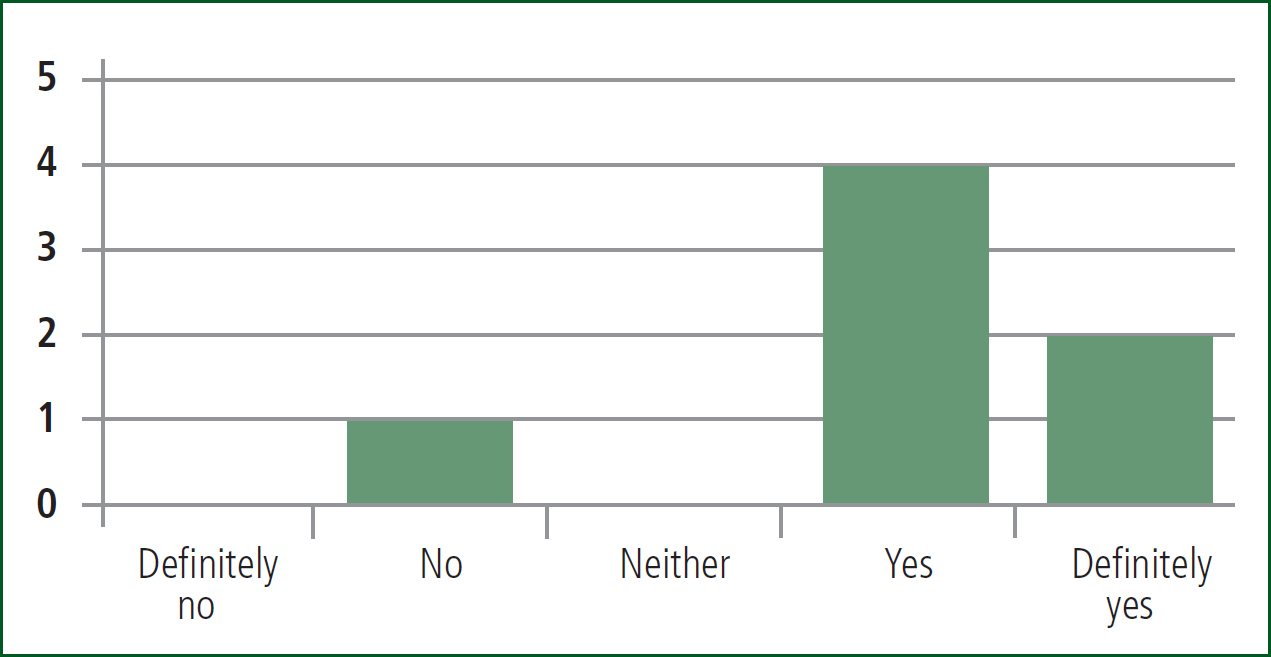
The staff involved in this project were all ECARe paramedics, and therefore experienced clinicians who had all received extra training. The feedback given in Figures 4, 6 and 7 exhibits that although the clinicians would have suspected sepsis in these cases, a lactate measurement reinforced this. The results in Figure 7 are encouraging as they show that in 50% of cases the use of POC lactate had an effect on the treatment delivered.
The large number of patients who presented with lactate as the only sign of organ dysfunction on the SST, raises concerns that without the POC patients are at risk of treatment being delayed. Erwin et al (2011) described that paramedics were able to detect sepsis but were not able to differentiate between sepsis and severe sepsis, so the addition of POC lactate helps to address this issue. The ability to differentiate between sepsis and severe sepsis could help prevent inappropriate hospital admissions, as sepsis can, where appropriate, be managed by primary care in the community.
Although there were only a small number of patients who had both capillary and venous samples taken, there is a suggestion that the values may differ depending on the source of the sample. In cases where both a capillary and venous sample were taken the capillary sample was higher in all cases. This is in contrast to Bakker et al (2013) and Browning et al (2014) who claim that the sample site does not overly affect the result.
Due to the small numbers of patients in this study having both venous and capillary samples taken it has not been possible to form any analysis of these results. Therefore the site for taking lactate samples should be standardised in future protocols and further work could be undertaken to ascertain if lactate based triggers in sepsis screening tools should vary depending on the source of the sample. The difference in lactate measurement between the source sites could lead to patients triggering, or not triggering, a treatment pathway, and therefore further work is required to investigate these differences.
There are a number of limitations to this project. The purpose of the study was to evaluate the feasibility of paramedic use of pre-hospital lactate measurement using the Nova StatStrip Lactate Xpress, to evaluate their feedback, and to analyse the effect of the introduction of lactate measurement on the SST. The study did not assess the effect of lactate measurement on the patient pathway, their end diagnosis, or the effect the introduction of lactate measurement had on the sensitivity and specificity of the SST.
The small number of staff exposed to the device, the lack of follow up to compare pre-hospital measurements with in-hospital measurement and the lack of patient outcome data to judge the impact of POC lactate are all acknowledged as weaknesses in this study. Addressing these elements is of interest for future work, but was beyond the remit of this study.
Further work could explore the accuracy of the sepsis screening tools used by paramedics and what impact the addition, or omission, of lactate measurement would have on the patient pathway, treatment, quality of life, and survival to discharge. There is also scope for exploring the use of lactate in trauma through targeting practitioners with a higher exposure to trauma cases such as the Hazardous Area Response Teams (HART) to examine any impact in this population.
Conclusions
POC lactate testing in the pre-hospital environment has been shown to be feasible. POC lactate measurement may benefit patients by identifying more cases of severe sepsis which then allows paramedics to start appropriate treatment earlier. The population encountered, and the range of lactate values recorded, are in accordance with figures reported in the current literature. The low number of trauma cases was not unexpected and is a population that needs to be studied separately. Further work is needed to examine the impact of adding lactate to the paramedic toolbox and its place in the SST. Concerns were identified with staff conducting quality control checks around POC in the pre-hospital environment which requires further investigation.

