Out-of-hospital cardiac arrest (OHCA) is a major public health concern in industrialised countries, with high mortality rates (Zhou et al, 2018). UK emergency medical services treat 30000 OHCAs annually (Perkins and Brace-McDonnell, 2015) but the survival rate remains persistently low. High-quality cardiopulmonary resuscitation (CPR) and early defibrillation, where indicated, are essential to achieve optimal outcomes (Deakin et al, 2010).
Sudden OHCA results in cessation of cardiac function with haemodynamic collapse leading to anaerobic metabolism (Dadeh and Nuanjaroan, 2018). In anaerobic conditions, tissue hypoxia leads to an accumulation of lactate (Mizock and Falk, 1992).
Patients who have had an OHCA are hypoxic, hypoperfused and experience hyperlactataemia, most likely caused by ischaemia and inflammation resulting from ischaemia-reperfusion injury (Donnino et al, 2007; Cocchi et al, 2011), which is a surrogate marker for hypoxic insult (Orban et al, 2017).
During OHCA, lactate concentrations increase with duration of down time (Carden et al, 1985), and are influenced by quality of bystander CPR (BCPR) and initial rhythm (Zhou et al, 2018), which are known to influence survival.
Current guidelines recommend the measurement of lactate in patients after cardiac arrest to guide therapy, although the International Liaison Committee on Resuscitation recognises a knowledge deficit in the evidence supporting this guideline (Nolan et al, 2008).
Several observational studies suggest hyperlactataemia is prognostic of mortality in patients with cardiac arrest, but comparisons are difficult as research has focused mainly on OHCA patients who achieved return of spontaneous circulation (ROSC) (Nishioka et al, 2021) and involved varying outcome measures and populations of interest (Kliegel et al, 2004; Williams et al, 2016).
The PREDICT study explored serum lactate levels as a predictor of ROSC in patients who experienced OHCA after arrival at hospital (Charlton and Moore, 2021).
The prognostic value of lactate during OHCA and concurrent with CPR remains controversial and unclear (Donnino et al, 2007; Yanagawa et al, 2009).
Method
A single-centre, prospective cohort study was conducted by North East Ambulance Service NHS Foundation Trust between 17 February 2020 and 31 March 2021.
Eligibility
Those eligible for inclusion were patients experiencing OHCA, aged ≥18 years who were receiving resuscitation in accordance with current European Resuscitation Council (ERC) guidelines, in the study area of Newcastle or Gateshead hospitals and attended by a specialist emergency care paramedic (SPEC).
Patients known to be or apparently pregnant, experiencing OHCA as a result of a blunt or penetrating injury and where intravenous (IV) access was absent were excluded.
Lactate collection
SPECs measured lactate concentrations using the StatStrip Xpress (Nova Biomedical) point-of-care (POC) instrument. Samples were taken from either a new IV line if the patient had received intraosseous access from the first crew or an IV line already in situ if it was not possible to secure a dedicated IV line for the purposes of the study. If the latter option was used, 20ml of venous blood was drawn and disposed of before the sample used for the lactate measurement.
Lactate concentrations were measured using 0.6µl of whole venous blood obtained during a non-specified point during a CPR attempt and samples processed immediately. It was not possible to obtain the measurements at the same time point during each resuscitation attempt because of the evolving emergency situation and as numbers of ambulance staff present at each OHCA varied.
Changes in lactate are slow and develop over a period of hours (Vincent et al, 2016). Lactate clearance was therefore unlikely to occur during a standard OHCA because most resuscitation attempts last between 20 and 30 minutes. Consequently, lactate concentrations were measured only once.
Neither SPECs, nor the research team, were blinded to lactate concentrations. Lactate concentrations were recorded on the ambulance electronic patient care record and confirmed against the POC instrument retrospectively by the research team.
All patients continued to receive standard care during study participation. CPR continued until sustained ROSC was achieved and the patient was conveyed to hospital, recognition of life extinct (ROLE) was declared or the patient was conveyed to hospital with CPR ongoing. Patients remained in the study until ROLE was declared or the patient arrived at hospital with either ROSC or CPR ongoing.
Study instruments
Study instruments were calibrated during manufacture and underwent a process of quality control which involved testing against an in-hospital blood gas analyser (IL Gem 5000)—the reference standard, located within the emergency department—before the study started.
Study instruments were subject to continuing quality control on a monthly basis throughout the study period. These instruments could detect lactate in the 0.3–20.0 mmol/l range; measurements above this were reported as HI (the machine's result to indicate high/excessive levels).
Outcomes
The primary outcome was survival to hospital measured by ROSC after arrival at hospital. Secondary outcomes were the percentage ROSC rate at any time during CPR and 30-day survival with neurological outcomes, measured using the modified Rankin scale (mRS) (ranging from 0=no symptoms to 6=death) (Haywood et al, 2018). A favourable neurological outcome was defined as 0–3 on the mRS and a poor outcome as 4–6.
Statistical analysis
Study instruments could detect numerical serum lactate concentrations up to 20.0 mmol/l, with concentrations beyond this reported as HI. The mid value is 10 mmol/l and, for analysis, patients were divided into two dichotomised groups using this value as a cut-off point:
Counts (n) and frequencies (%) are presented for each group. Continuous data were analysed using a t-test, and categorical data using χ2. A logistic regression model was performed to identify lactate measurements associated with survival to hospital. Data are presented to two decimal places. A significance threshold of <0.05 was accepted as statistically significant. Confidence intervals are reported as appropriate. Data were analysed using R 3.6.2 (R Project).
Results were reported in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies (von Elm et al, 2007).
Ethics and trial registration
OHCA is a sudden event where patients unexpectedly lose consciousness and mental capacity, so it was not possible to obtain written informed consent at the time of enrolment. We sought written informed consent to collect data about their care from all surviving patients and from a legal representative where the patient had impaired mental capacity.
Yorkshire and Humber-Bradford Leeds research ethics committee (REC: 19/YH/0363) and the Confidentiality Advisory Group (CAG: 19/CAG/0201) provided ethics approval and support for this study. The study registration number is ISRCTN 24519917.
Results
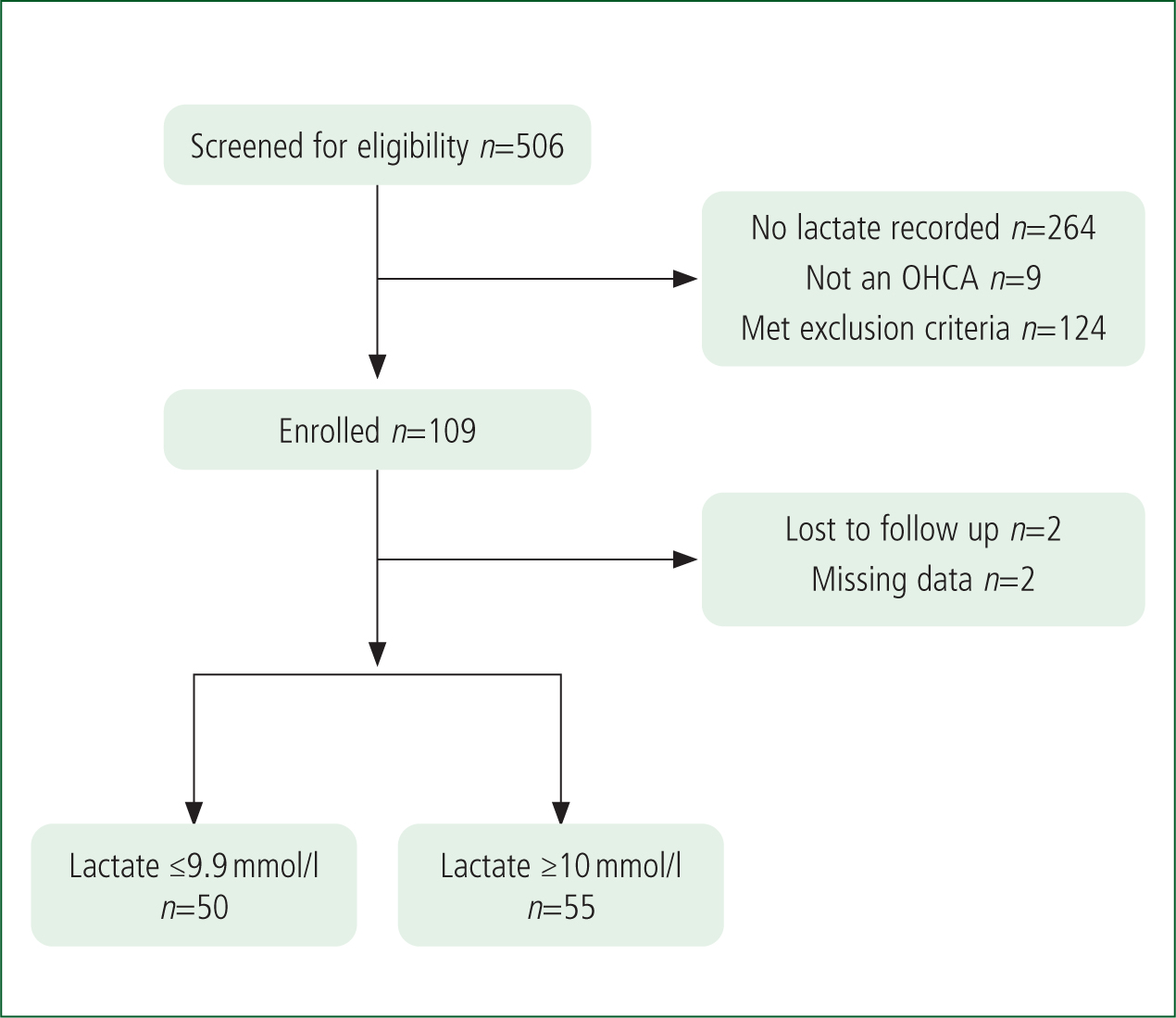
Of the 506 patients attended by the SPECs in the study period, 375 were eligible and 109 (29%) were enrolled. Two patients were lost to follow-up as they survived with poor neurological function and the research team was unable to identify a legal representative to approach regarding written informed consent. Two patients were withdrawn because of missing data. This resulted in 105 patients with data for analysis. Fifty patients were included in group 1 (low lactate) and 55 in group 2 (high lactate) (Figure 1).
Patients in group 1 were slightly older than those in group 2 (63 versus 60.3 years) and significantly more likely to be male (78% versus 50%; P≤0.01). Both groups were similar regarding the location where OHCA occurred, the event being witnessed, rate of BCPR, insertion of supraglottic airway and mechanical CPR. Patients in group 1 were more likely to be in an initial shockable rhythm than those in group 2 (40% versus 14.5%; P≤0.01) and therefore received a higher mean number of shocks (3.2 versus 0.98; P≤0.01).
There was little difference in the mean dose of epinephrine administered between the two groups (4.8 versus 4.3; P=0.18), and the arrest to arrival of emergency medical services interval (the time of OHCA and arrival of first ambulance resource) was also similar (9 minutes 13 seconds versus 9 minutes 58 seconds; P=0.62).
Patients in group 1 had a shorter time to first epinephrine interval (time of arrival of first ambulance resource to time of administration of first dose of epinephrine) than patients in group 2 (12 minutes 48 seconds compared to 14 minutes 3 seconds; P=0.45). In addition, patients in group 1 had a shorter arrest to ROSC interval (time of OHCA confirmed to time of sustained ROSC achieved) compared to group 2 (37 minutes 38 seconds versus 39 minutes 13 seconds; P=0.79). Median lactate concentrations were lower in group 1 than in group 2 (7.4 versus 14.2 mmol/l). OHCA characteristics by group are shown in Table 1.
| Group 1 (lactate ≤9.9 mmol/l) | Group 2 (lactate ≥10 mmol/l) | P | 95% CI | |
|---|---|---|---|---|
| n | 50 | 55 | ||
| Mean age (years) | 63 | 60.3 | 0.4 | -9.2 to 3.2 |
| Male sex | 39 (78%) | 28 (50%) | <0.01 | |
| Median lactate concentration (range) | 7.3 mmol/litre (2.1–7.4) | 14.2 mmol/litre (10.1–HI) | ||
| Public location | 7/50 (14%) | 7/54 (13%) | 0.87 | |
| Witnessed OHCA* | 25/49 (50%) | 31/53 (56.3%) | 0.44 | |
| BCPR* | 41/48 (82%) | 46/53 (83.6%) | 0.84 | |
| Supraglottic airway | 40 (80%) | 47 (85.5%) | 0.45 | |
| Endotracheal tube | 9 (18%) | 6 (11%) | 0.3 | |
| BVM only** | 1 (2%) | 2 (4%) | N/A | |
| Initial rhythm shockable: VF | 20 (40%) | 8 (14.5%) | <0.01 | |
| Initial rhythm non-shockable: asystole/PEA | 30 (60%) | 47 (85.5%) | <0.01 | |
| Mechanical CPR | 16 (32%) | 18 (32.7%) | 0.93 | |
| Intravenous drug route | 30 (60%) | 27 (49%) | 0.26 | |
| Intraosseous drug route | 16 (32%) | 24 (43.6%) | 0.22 | |
| IV and intraosseous drug route** | 4 (8%) | 4 (7.2%) | N/A | |
| Arrest-to-EMS arrival interval | 9 minutes 13 seconds | 9 minutes 58 seconds | 0.62 | −2.2 to 3. |
| Arrest-to-ROSC interval | 37 minutes 38 seconds | 39 minutes 13 seconds | 0.79 | −11 to 14 |
| Arrest-to-ROLE interval | 45 minutes 57 seconds | 47 minutes 3 seconds | 0.71 | −4.7 to 6. |
| Number of adrenaline mg (mean) | 4.8 | 4.3 | 0.18 | −1.2 to 0. |
| Number of shocks (mean) | 3.2 | 0.98 | <0.01 | 0.8 to 3.6 |
| Time to first epinephrine interval (mean) | 12 minutes 48 seconds | 14 minutes 3 seconds | 0.45 | −2 to 4.7 |
*Missing data; **insufficient data to compute χ2test.
BCPR: bystander cardiopulmonary resuscitation; BVM: bag-valve mask; CPR: cardiopulmonary resuscitation; HI: lactate concentrations >20.0 mmol/l; IV: intravenous; OHCA: out-of-hospital cardiac arrest; PEA: pulseless electrical activity; ROLE: recognition of life extinct; ROSC: return of spontaneous circulation; VF: ventricular fibrillation; P: probability value for differences in OHCA characteristics between groups
Primary and secondary outcomes
Outcome data are shown in Table 2. Fifteen out of the 50 (30%) patients in group 1 and 17/55 (31%) patients in group 2 were conveyed to hospital. Eleven out of 50 (22%) patients in group 1 and 14/55 (25.5%) patients in group 2 had a ROSC after arrival at hospital (P=0.67) and a similar number of patients were conveyed with CPR ongoing (8% versus 5.5%; P=0.61). A comparable rate of ROSC at any time during CPR was observed in both groups (36% versus 34.5%; P=0.87.
| Group 1 (lactate ≤9.9) mmol/l | Group 2 (lactate ≥10) mmol/l | P | |
|---|---|---|---|
| Total conveyed to hospital (n) | 15 | 17 | |
| Primary outcome | |||
| Survival to hospital with ROSC | 11/50 (22%) | 14/55 (25.5%) | 0.67 |
| Conveyed with CPR ongoing | 4/50 (8%) | 3/55 (5.5%) | 0.61 |
| Secondary outcomes | |||
| ROSC at any time | 18/50 (36%) | 19/55 (34.5%) | 0.87 |
| Other outcomes | |||
| Survived to 30 days** | 1/15 (7%) | 1/17 (6%) | N/A |
| Favourable neurological outcome (0–3 mRS)** | 1/15 (7%) | 1/17 (6%) | N/A |
| Deceased in emergency department | 8/15 (53%) | 12/17 (70.5%) | 0.31 |
| Survived ≥24 hours | 6/15 (40%) | 4/17 (23.5%) | 0.32 |
| ROLE on scene | 35/50 (70%) | 38/55 (69%) | 0.91 |
** insufficient data to calculate χ2. P value is for outcome between groups
CPR: cardiopulmonary resuscitation; mRS: modified Rankin scale; ROLE: recognition of life extinct; ROSC: return of spontaneous circulation
One patient in each group was alive at 30 days with good neurological function (0–3 on the mRS). From the remaining surviving patients, more in group 1 survived ≥24 hours than in group 2 (40% versus 23.5%), p=0.32.
Lactate as a predictor
Logistic regression indicated no statistical evidence that lactate concentrations were an independent predictor of ROSC after arrival at hospital (P=0.99) or at any time during CPR (P=0.83). Other numeric and binary factors were also non-predictive of either outcome.
Initial rhythm of ventricular fibrillation was predictive of ROSC after arrival at hospital compared to asystole (P≤0.01) and ventricular fibrillation (P≤0.01) and defibrillation (P=0.02; 95% CI (0.06–0.42)) were predictive of ROSC at any time.
Independent predictors of ROSC at both time points are shown in Table 3.
| ROSC after arrival at hospital | ROSC any time | |||
|---|---|---|---|---|
| P | 95% CI | P | 95% CI | |
| Numeric predictors | ||||
| Lactate | 0.99 | −0.20 to 0.20 | 0.83 | −0.18 to 0.22 |
| Adrenaline | 0.22 | −0.27 to 0.12 | 0.11 | −0.04 to 0.34 |
| Defibrillation | 0.16 | −0.05 to 0.32 | 0.02 | 0.06 to 0.42 |
| Age | 0.89 | −0.2 to 0.18 | 0.51 | −0.13 to 0.25 |
| Binary predictors | ||||
| Male sex | 0.65 | N/A | 0.80 | N/A |
| BCPR | 0.16 | N/A | 0.30 | N/A |
| Multilevel predictors | ||||
| Asystole versus PEA | 0.09 | N/A | 0.10 | N/A |
| Asystole versus VF | <0.01 | N/A | <0.01 | N/A |
BCPR: bystander cardiopulmonary resuscitation; P: probability value for independent predictors of ROSC after arrival at hospital and any time;
CI: confidence interval;
PEA: pulseless electrical activity; ROSC: return of spontaneous circulation; VF: ventricular fibrillation
Discussion
In this study, patients who were observed to have lower lactate concentrations (group 1) were older, more likely to be male, be in an initial shockable rhythm, have received their first dose of epinephrine more quickly, have obtained an ROSC more quickly and be associated with short-term survival (≥24 hours). However, the study did not show that lower compared to higher lactate concentrations could predict long-term survival, as both groups contained one patient who survived to 30 days with good neurological recovery.
Furthermore, the authors did not identify the cut-off point at which lactate concentrations were predictive of ROSC after arrival at hospital or at any time during resuscitation.
Evidence supporting prognostication of serum lactate and survival after cardiac arrest is dominated by research involving patients experiencing an in-hospital cardiac arrest or those conveyed to hospital after an OHCA, and the predictive cut-off points vary from study to study.
Wang et al (2015) retrospectively analysed data for 340 patients experiencing an in-hospital cardiac arrest and reported a mean lactate of 9.6 mmol/l and a mean resuscitation duration of 28.8 minutes. A serum lactate of <9 mmol/l was positively associated with survival to hospital discharge (OR 2.00; 95% CI (1.01–4.06)).
In an observational study measuring ammonia and serum lactate concentrations after arrival at hospital after resuscitation, Shinozaki et al (2011) reported median lactate concentrations of 9.2 mmol/l and 12.1 mmol/l in favourable and poor outcome groups respectively. The authors report an optimal cut-off point of 12 mmol/l correlated with survival, but this was observed in patients admitted to the acute care unit and is not representative of the wider cohort of patients who experience cardiac arrest in the community.
Seeger et al (2013) retrospectively analysed data for 206 patients experiencing cardiac arrest who were admitted to an intensive care unit. Data indicated the median lactate after hospital admission was 6.88 mmol/l and a cut-off point of 6.94 mmol/l, combined with a pH of 7.21, were associated with positive outcomes.
In a retrospective study exploring lactate in OHCA patients arriving at hospital with ongoing CPR, Dadeh and Nuanjaroan (2018) reported cut-off points of 9.1 mmol/l and 9.4 mmol/l to predict survival to 24 hours and 48 hours respectively, but found initial lactate had no association with sustained ROSC. In this study, only 14% of patients received BCPR and 11.6% were in an initial shockable rhythm, both of which increase the chance of survival.
The present study differs from previous research in several ways. First, the lactates measured were taken shortly after circulatory cessation rather than when ROSC had been restored or the patient had a prolonged resuscitation interval. Lactate is a marker of prolonged circulatory standstill (Ralston et al, 1985; Carden et al, 1987) and OHCA frequently involves periods of no or poor-quality CPR (possibly from non-recognition or reluctance or inability to perform BCPR), making ROSC less likely.
This may explain why many of the lactate concentrations in this study were higher than those discussed earlier. In addition, patients in this study were subject to prolonged arrest to ROLE or ROSC intervals. This may be a result of the study design, which required patients to still be receiving CPR at the point of enrolment. Patients who obtained ROSC as a result of initial CPR, defibrillation or epinephrine were ineligible as ROSC had been restored, leaving those with a requirement for prolonged resuscitation being included.
Patients in our study did not benefit from lactate clearance, which is known to favour improved outcomes (Donnino et al, 2007). Patients who experience a rapid drop in lactate concentration are more likely to recover. A prospective, multicentre study involving 543 OHCA patients reported that, irrespective of initial lactate level, effective lactate reduction 6 hours after cardiac arrest was associated with survival and good neurological outcomes (Hayashida et al, 2017). The short duration of most OHCAs, the varied aetiologies behind why these events occur and limited prehospital therapies to resolve hyperlactataemia preclude the initiation of lactate clearance during OHCA.
It is unsurprising that an initial shockable rhythm as an independent predictor was associated with ROSC after arrival at hospital and ROSC at any time during CPR, compared to asystole and pulseless electrical activity. The link is well established (Stiell et al, 1999; Wissenberg et al, 2013) and is known to correlate with various factors such as a younger age and male sex (Rajan et al, 2016). Patients enrolled in our study in group 1 were more likely to be in an initial shockable rhythm despite being similar at baseline to group 2, except for female sex. It remains unclear why women patients were underrepresented in this group.
Patients in group 1 also had a shorter time to first dose of epinephrine and arrest-to-ROSC interval, which, although not statistically significant, are known to be clinically advantageous regarding favourable outcomes. Patients with a lower initial lactate concentration have a higher possibility of ROSC (Koami et al, 2017) although the authors of the present study observed similar rates of ROSC in both groups. It was short-term survival that differentiated the groups once ROSC had been restored.
Limitations
The SPECs were not blinded to the POC lactate concentrations and, as such, some bias towards treatment and decisions may have been introduced. However, given that lactate in this population is under-reported and optimal cut-off points are unknown, the authors do not believe that SPECs altered decision-making or interventions because of this.
Participant recruitment was devolved to SPECs rather than non-specialist paramedics so all patients received an enhanced level of care during their resuscitation. This may have influenced the primary and secondary outcomes, although these were balanced across both groups.
Two patients who survived to 30 days were removed from analysis as we were unable to obtain written informed consent. Given the small number of OHCAs in this study, it is possible that the absence of these cases denies the study valuable data regarding lactate concentrations and quality of survival.
The authors did not collect data regarding the time between collapse and lactate concentration being measured, prehospital post-ROSC lactate or lactate concentrations measured in hospital. These data would undoubtedly offer insights regarding the trajectory of lactate concentrations and their association with short and long-term survival.
The authors were unable to undertake all data analysis as planned. The small dataset resulted in insufficient data to identify a lactate cut-off point. Lactate concentrations did not correlate to ROSC and the authors were thus unable to calculate the sensitivity or specificity, positive and negative predictive value, receiver operating characteristic curve or area under the curve, statistics.
The study was not statistically powered so any indication of short-term survival should be viewed with caution. The authors acknowledge different results could be produced were a different cohort of patients enrolled; a larger, statistically powered study is required.
The study was conducted at the beginning of the coronavirus pandemic when paramedic management of OHCA became more complex, delays in paramedics delivering CPR were likely because they had to don personal protective equipment (Ong et al, 2021) and response times became longer (Perkins and Couper, 2020). These may have influenced the outcomes of patients in this study.
Conclusion
This observational cohort study presents one perspective of the relationship between lactate and OHCA. Lower lactate levels in OHCA patients appear to be associated with better short-term outcomes. The study did not demonstrate that lower lactate wwconcentrations could predict long-term survival and the optimal cut-off point at which survival could be predicted remains unclear.
Although this study did identify areas of interest regarding advantageous clinical characteristics and short-term survival, the role of lactate in OHCA remains unclear.
Further research involving a larger sample is required to determine the role of lactate regarding long-term survival.

