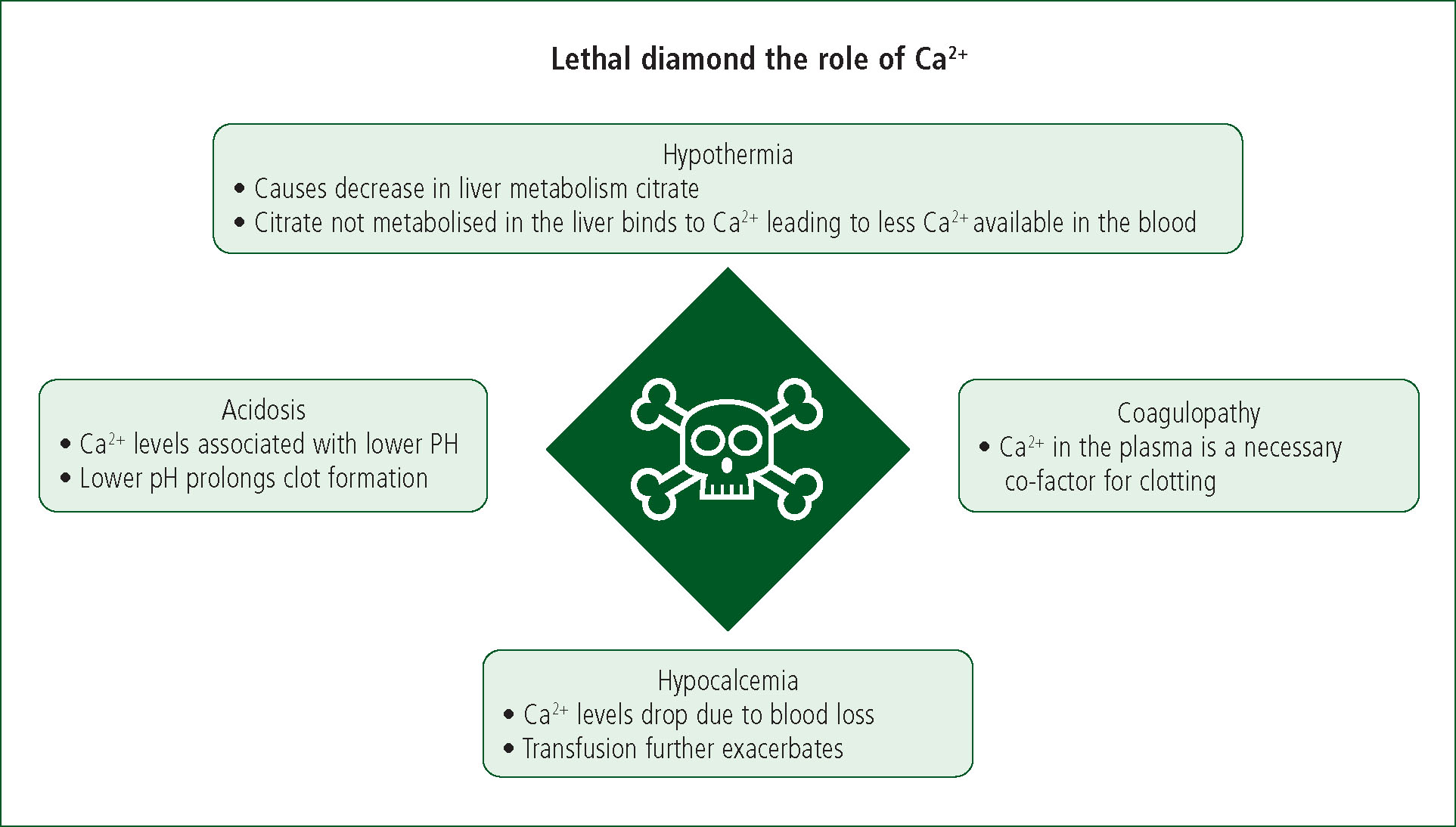
Hypothermia, coagulopathy and acidosis are known collectively as the lethal triad (Ditzel et al, 2020). Together with haemostatic measures and replacement of blood, managing the lethal triad is a significant focus of ‘damage control resuscitation’ for haemorrhagic shock (Joint Trauma System, 2019). Calcium ion (Ca2+) depletion is also suspected of influencing mortality in traumatic haemorrhage, leading to the addition of hypocalcaemia to the lethal triad and the theorisation of the lethal diamond (Figure 1).
Calcium and haemorrhagic shock
Calcium ions initiate actin-myosin filament binding, resulting in myofibril (muscle-fibre) shortening and muscle contraction. Depletion of calcium ions because of loss during haemorrhage and consumption from clot formation can therefore reduce myocardial contractility and vascular smooth-muscle tone, thereby reducing cardiac output and blood pressure, exacerbating shock (Spahn et al, 2019).
Calcium is also essential for platelet adhesion and factors II, VII, IX and X in the clotting cascade. Hypocalcaemia therefore has the potential to exacerbate coagulopathy, leading to further haemorrhage. Patients who receive transfusions to replace blood loss are at risk of experiencing further depletion of calcium ions from citrate, a chelating (ion-binding) agent that is added to transfusion products to prevent calcium from causing donor blood to coagulate (Spahn et al, 2019). This is a pertinent consideration for prehospital administration of blood products, as well as for paramedics who may not carry or transfuse blood products but expect a patient with shock from traumatic haemorrhage to receive blood transfusions on arrival at hospital.
Many trauma centres now supplement multiple blood transfusions with intravenous calcium within their mass transfusion protocol (MTP) (Spahn et al, 2019; Cornelius et al, 2020). Some prehospital services, including several UK-based helicopter emergency medical services, do this too. In Australia, Ambulance Victoria flight paramedics administer intravenous calcium gluconate when they administer four or more units of packed red blood cells (pRBC) (Ambulance Victoria, 2020).
The purpose of this systematic literature review was to determine whether paramedic administration of intravenous calcium for haemorrhagic shock in trauma has the potential to reduce morbidity and mortality.
Methods
The MEDLINE and CINAHL databases were searched on 20 August 2021 using the strategy shown in Table 1.
| Database search terms | Results | |
|---|---|---|
| MEDLINE | CINAHL | |
| Calcium | 576949 | 47 704 |
| Hypocalcaemia | 2233 | 2165 |
| Hypocalcemia | 11875 | 2165 |
| #1 OR #2 OR #3 | 582524 | 48 841 |
| Haemorrhage | 32 619 | 67 767 |
| Hemorrhage | 279646 | 67 767 |
| Bleeding | 188899 | 49 106 |
| Blood loss | 56 824 | 34 616 |
| #5 OR #6 OR #7 OR #8 | 445178 | 123919 |
| Trauma | 247824 | 112830 |
| #4 AND #9 AND #10 | 189 | 75 |
| Limit #17 to year ‘2016-Current’ | – | – |
| #11 AND #12 | 42 | 23 |
One person screened the titles of peer-reviewed articles investigating hypocalcaemia associated with traumatic haemorrhage published from 2016 onwards. Articles before 2016 (older than 5 years) were excluded to ensure relevance to current practice, especially given recent evolutions in prehospital transfusion practice. Studies unrelated to trauma were also excluded.
A manual search of references within the articles that met the inclusion criteria was also conducted to capture all relevant publications.
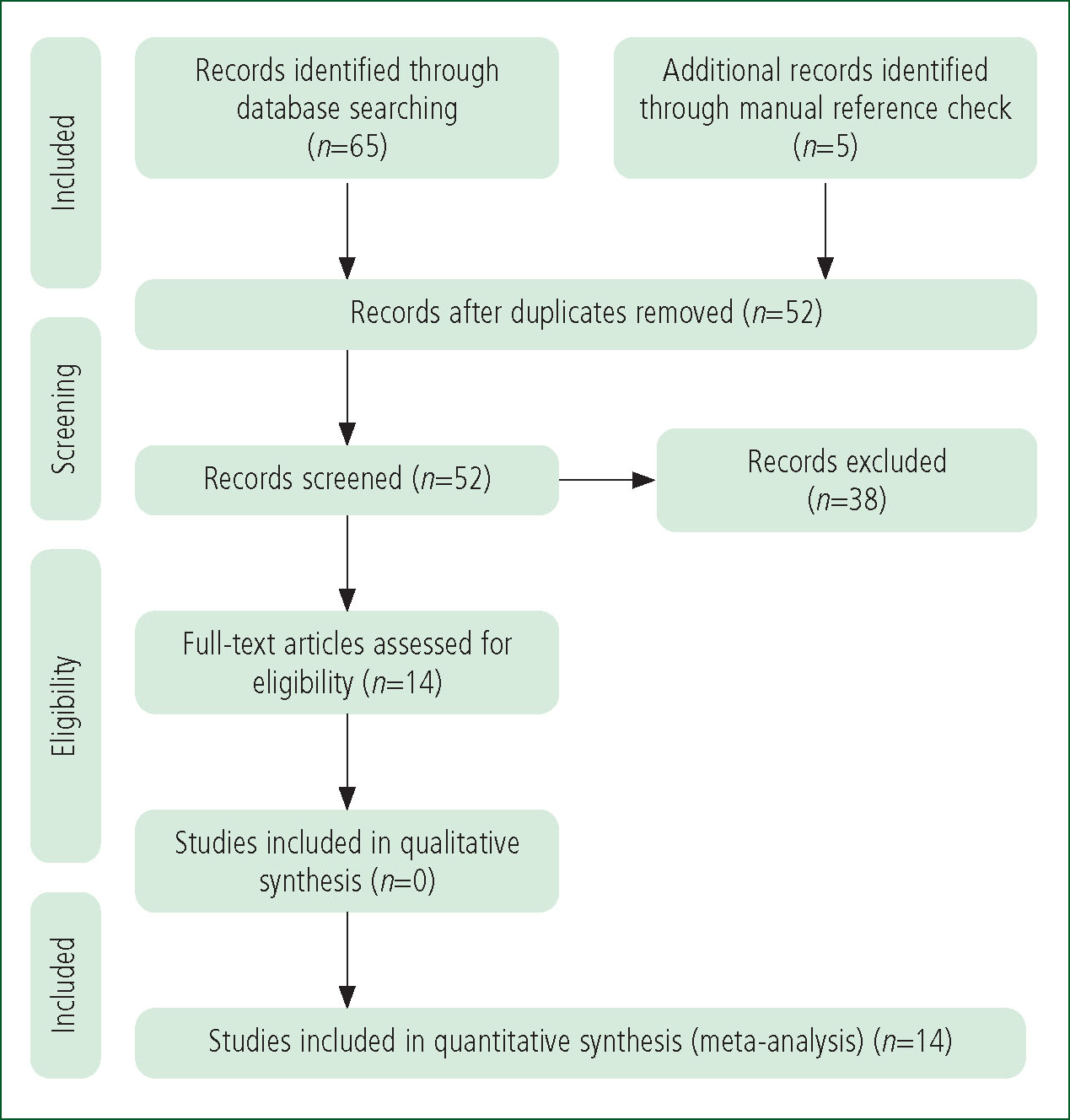
A total of 52 abstracts were screened from the database search with nine articles meeting the inclusion criteria. A further five studies were found after the references of these articles were manually checked. This yielded 14 articles (Figure 2).
Prehospital studies were keenly sought; five met the inclusion criteria. The remaining nine studies assessed hospital patients within the emergency department (ED) or trauma centre. All hospital and prehospital articles included in this review were relevant to paramedic practice in that they assessed aspects of patient management during or immediately after receiving paramedic care and had findings pertinent to paramedic practice.
Both military and civilian studies were included to assess whether injuries in either setting were associated with similar or differing patterns of hypocalcaemia.
The hierarchy of evidence was considered for all recommendations in this review. The rating system developed by Harbour and Miller (2001) was used to determine the level of evidence for each finding and to grade each recommendation (Table 2). These ratings are expressed alongside each finding and recommendation.
| Level of evidence | Type of study |
|---|---|
| 1++ | High-quality meta-analyses, systematic reviews of randomised controlled trials (RCTs) or RCTs with a very low risk of bias |
| 1+ | Well-conducted meta-analyses, systematic reviews of RCTs or RCTs with a low risk of bias |
| 1– | Meta-analyses, systematic reviews or RCTs or RCTs with a high risk of bias |
| 2++ | High-quality systematic reviews of case-control or cohort studies or high-quality case-control or cohort studies with a very low risk of confounding, bias or chance and a high probability that the relationship is causal |
| 2+ | Well-conducted case-control or cohort studies with a low risk of confounding, bias or chance and a moderate probability that the relationship is causal |
| 2– | Case-control or cohort studies with a high risk of confounding, bias or chance and a significant risk that the relationship is not causal |
| 3 | Non-analytic studies, e.g. case reports, case series |
| Grades of recommendations | |
| A | At least one meta-analysis, systematic review or RCT rated as 1++ and directly applicable to the target population or a systematic review of RCTs or a body of evidence consisting principally of studies rated as 1+ directly applicable to the target population and demonstrating overall consistency of results |
| B | A body of evidence including studies rated as 2++ directly applicable to the target population and demonstrating overall consistency of results or extrapolated evidence from studies rated as 1++ or 1+ |
| C | A body of evidence including studies rated as 2+ directly applicable to the target population and demonstrating overall consistency of results or extrapolated evidence from studies rated as 2++ |
| D | Evidence level 3 or 4 or extrapolated evidence from studies rated as 2+ |
Source: Harbour and Miller (2001)
Results
Table 3 summarises the included studies.
| Study (year) Country Demographic | Study design | Aim | Overall outcome (Level of evidence) |
|---|---|---|---|
|
Giancarelli et al (2016) |
Retrospective analysis of 156 adult trauma patients who had received MTP | To assess calcium levels and calcium repletion in association with delivery of MTP |
|
|
Webster et al (2016) UK |
Retrospective analysis of 55 adult and paediatric trauma patients | To assess the incidence of hypocalcaemia in trauma patients who received prehospital blood transfusion |
|
| MacKay et al (2017) United States Civilian population in a trauma centre | Retrospective analysis of 41 adult trauma patients where MTP was activated |
To assess calcium levels and calcium repletion in association with delivery of MTP, and morbidity and mortality |
|
|
Kyle et al (2018) |
Retrospective analysis of 297 combat casualties in Afghanistan who received blood products during aeromedical transport with a doctor, two paramedics and an emergency nurse | To compare calcium levels of those given calcium replacement (10 ml of 10% intravenous calcium chloride) versus those who were not |
|
| Byerly et al (2020) United States Civilian population in a trauma centre | Retrospective analysis of 7341 trauma patients over a period of 10 years | To determine if transfusion of blood products is an independent predictor of hypocalcaemia |
|
|
Cornelius et al (2020) |
Retrospective analysis of 197 adult and paediatric trauma patients | To determine the incidence of hypocalcaemia and the effect of calcium replacement in severely injured trauma patients |
|
| Matthay et al (2020) United States Civilian population in an ED | Analysis of 538 blood samples from adult trauma patients | To determine effects of serum calcium concentrations on platelet activation, platelet aggregation and clot strength |
|
| Moore et al (2020) United States Prehospital, civilian population | Systematic review of two RCTs (PAMPer and COMBAT
|
To investigate the effects of plasma administration in adults with traumatic haemorrhagic shock that required long-duration transport |
|
|
Vasudeva et al (2020) |
Retrospective analysis of 226 shocked adult trauma patients | To assess association of coagulopathy and mortality with hypocalcaemia |
|
|
Chanthima et al (2021) |
Retrospective analysis of 346 trauma patients aged ≥15 years | To assess whether hypocalcaemia and calcium administration are significantly associated with mortality |
|
|
Conner et al (2021) |
Retrospective analysis of 101 adult combat casualties in Afghanistan
|
To assess calcium levels before and after blood product administration |
|
|
Cornelius et al (2021) |
Retrospective analysis of 1305 paediatric trauma patients | To determine the incidence and management of hypocalcaemia in severe paediatric trauma |
|
| Hall et al (2021) United States Civilian population in multiple EDs | Retrospective analysis of 71 adult trauma presentations who received MTP | To investigate calcium monitoring and supplementation for adult trauma patients receiving MTP |
|
|
Vasudeva et al (2021) |
Systematic review of three retrospective studies of 1213 adult trauma patients | To assess for association between hypocalcaemia on arrival to ED and blood transfusion requirement, coagulopathy and mortality |
|
ED: emergency department; MTP: mass transfusion protocol
Aetiology of hypocalcaemia in severe traumatic haemorrhage
Hypocalcaemia was present in 50–55% of adult trauma patients arriving at ED with significant haemorrhage (Webster et al, 2016; Vasudeva et al, 2020; Conner et al, 2021; Hall et al, 2021) (level 2+ evidence). Collectively, these retrospective studies represent a large sample size of both civilian and military populations with strong generalisability and external validity.
The highest prevalence of hypocalcaemia found in both civilian and military settings was in patients with blast and penetrating injuries (Byerly et al, 2020; Conner et al, 2021) (level 2++). A large study by Cornelius et al (2021) also found that paediatric patients developed hypocalcaemia in traumatic haemorrhage situations that required operative intervention or where blood transfusions had been administered (level 2++).
Prehospital administration of blood products increased the incidence of hypocalcaemia, with Kyle et al (2018) and Conner et al (2021) demonstrating this in 70% and 75% of patients respectively (level 2++). Webster et al (2016) demonstrated a fall in ionised calcium levels with 95% of patients who received any amount of transfused blood (level 2+). The magnitude of hypocalcaemia was found to be proportional to the amount of blood product transfused, with greater severity seen with transfusions of four or more units of pRBC or fresh frozen plasma (Byerly et al, 2020) (level 2++).
Hypocalcaemia and coagulopathy
Matthay et al (2020) assessed the effect of calcium on coagulation, and found ionised calcium levels independently influenced platelet activation and clot strength, and that clotting was impaired from hypocalcaemia (level 2++).
Key Points
Morbidity and mortality of hypocalcaemia in trauma
A systematic review by Vasudeva et al (2021) demonstrated higher incidences of prehospital hypotension, coagulopathy and transfusion requirements in hypocalcaemic trauma patients (level 2++).
Increased mortality was demonstrated in both adult and paediatric trauma patients with hypocalcaemia in all but one study that assessed this (Moore et al, 2020; Cornelius et al, 2021; Vasudeva et al, 2021) (level 1++ and 2++). Chanthima et al (2021) did not find a significant association between initial ionised calcium measurement and mortality (level 2–). In this study, however, more than half of patients received calcium replacement, significantly more than in the other studies. Whether calcium replacement independently reduced mortality could not be assessed by retrospective data collection.
Calcium administration
Kyle et al (2018) found that when prehospital teams administered a single dose of 1 g of calcium chloride to patients who had received an average of four units of blood products, only 28% arrived to ED hypocalcaemic versus 70% who had not received calcium (level 2++).
Giancarelli et al (2016) found patients receiving MTP (≥10 units blood products) who were administered an average dose of 2 g of calcium chloride did not reach normal calcium levels nor experience hypercalcaemia on subsequent measurements (level 2++).
MacKay et al (2017) assessed MTP patients who received even higher calcium doses, finding 22% developed hypercalcaemia (level 2–). This hypercalcaemic group had a 78% mortality rate, which was equal to the mortality rate found with severe hypocalcaemia.
These studies highlight the need for determination of optimal calcium dosage, particularly given the potential for hypercalcaemia and mortality from overcorrection, although the pilot study by MacKay et al (2017) that found this had a very small sample size (n=41), which raises questions over validity.
Cornelius et al (2020) found mortality was greater when calcium was not replaced in hypocalcaemic trauma patients (level 2+), while Chanthima et al (2021) did not demonstrate adverse events or mortality associated with calcium administration (level 2–).
CPD Reflection Questions
Discussion
This is the first systematic literature review investigating prehospital hypocalcaemia management for trauma patients with haemorrhagic shock.
The evidence suggests that hypocalcaemia manifests in at least half of these patients before blood transfusion and three-quarters after transfusion, and is associated with hypotension, coagulopathy, increased transfusion requirements and mortality (Webster et al, 2016; Kyle et al, 2018; Vasudeva et al, 2020; Conner et al, 2021; Hall et al, 2021). Early calcium correction may benefit these patients and paramedicine can potentially play a key role.
Matthay et al (2020) recommend maintaining normal ionised calcium levels during critical bleeding given the association between hypocalcaemia and coagulopathy. It is important to note that prehospital intravenous administration of calcium was shown to halve the incidence of hypocalcaemia in patients who had received blood products (Kyle et al, 2018). Ambulance services therefore should and regularly do give calcium supplementation to trauma patients receiving multiple units of blood products (grade B recommendation).
However, should consideration also be given to empirical administration of calcium when blood transfusion is foreseeable for trauma patients in haemorrhagic shock? Considerations regarding policy for this might include mechanism of injury, injury patterns and signs such as hypotension associated with traumatic haemorrhage.
Logistical considerations might also be important. Longer duration transport or increased time on scene in situations such as entrapment or where lengthy interventions are required for stabilisation might lend to greater patient benefit from calcium replacement. Conversely, if administering calcium delays the arrival of a trauma patient to definitive care or distracts a small prehospital team from performing other critical interventions, it might be detrimental to the patient.
It is worth noting that it is recommended to give 1 g of calcium gluconate over 2–5 minutes intravenously, as it can cause hypotension and bradycardia if administered too rapidly (Ambulance Victoria, 2020).
Treatment methods for hypocalcaemia varied in the literature as did some of the results. Kyle et al (2018) found prehospital administration of 1 g intravenous calcium chloride normalised calcium levels on ED admission for the majority of patients who had received an average of four units of pRBC or fresh frozen plasma (grade B). Giancarelli et al (2016), however, found that twice that amount of calcium chloride was still not enough to normalise calcium levels in patients receiving mass transfusion in the ED (grade B). MacKay et al (2017), on the other hand, found incidences of overcorrection when greater amounts of calcium were given with their MTP, linking hypercalcaemia to increased mortality (lower-quality evidence).
These results underscore the need for clear protocols to guide paramedic administration of calcium during haemorrhagic shock in trauma. Choice of calcium preparation may also be important and paramedic practice may benefit from a standardised approach. It is important to note that calcium chloride contains three times as much calcium per millilitre as calcium gluconate and carries a greater risk of tissue necrosis than calcium gluconate if extravasation occurs (Ambulance Victoria, 2020). They must therefore not be used interchangeably.
Limitations in the data gathered are evident in this review as all studies except two are retrospective. Controls therefore could not be implemented to determine whether hypocalcaemia and calcium replacement have causative or correlative relationships with trauma mortality.
While it appears that empirical calcium administration may reduce hypocalcaemia, the safest and most effective indications, dosage and preparations need to be determined. A double-blinded randomised control trial could determine whether prehospital calcium administration would benefit patients with severe traumatic haemorrhage.
Conclusion
The findings in this systematic literature review link the ramifications of hypocalcaemia to poor yet potentially modifiable outcomes in trauma.
Ambulance services should consider treatment with calcium when patients receive or are expected to receive a blood transfusion for haemorrhagic shock in trauma. The significance of hypocalcaemia has been established, and further research is needed to differentiate whether hypocalcaemia is a cause or a predictor of trauma mortality and to guide prehospital calcium administration protocols.

